Playlist
Show Playlist
Hide Playlist
Cirrhosis: Clinical Presentation, Diagnosis, and Treatment
-
Slides GIP Cirrhosis.pdf
-
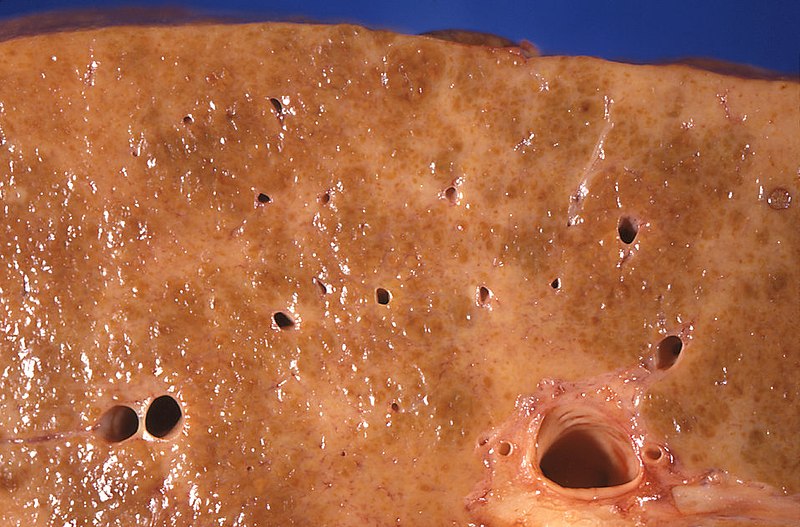
Download Lecture Overview
00:01 So the clinical presentation. 00:04 In cirrhosis that is no longer being adapted to and compensated, patients will have fatigue and weight loss. 00:13 They'll clearly be jaundice. 00:15 Because of the increased bile salts peripherally in the skin, they will develop pruritus that is pretty intense. 00:22 Asterixis can be one of the manifestations that you see involved in the encephalopathy. 00:28 And if you don't know what asterixis is, you would have your patient close their eyes, hold up their hand as if they're stopping traffic. 00:36 Now for me because I don't have cirrhosis, not that I know of, my hand stays up. 00:41 But if a patient has CNS effects, secondary to cirrhosis, they will do this. 00:49 And not be aware that they are flapping their hands, that's asterixis. 00:54 Patients can get Dupuytren's contractures. 00:57 So abnormal fibrosis typically of the ring finger. 01:00 For reasons that are not entirely clear, it's just one of those associations. 01:04 We'll see a hepatomegaly. 01:06 End stage, the liver tends to be smaller, but in earlier stages of cirrhotic injury, you may have an enlarged liver. 01:12 And because of that hypersplenism, and the impact on the portal circulation, you may have splenomegaly. 01:19 And then hyperestrogenism. 01:21 And that can present as increased vascular ectasia or telangiectasia, and even gynecomastia, in patients who have severely elevated levels of estrogen. 01:32 This is just showing you ascites, remember ascites is going to because of the portal hypertension, but also the hypoalbuminemia. 01:39 And this is going to be largely a serous effusion, so it's going to be water and electrolyte relatively protein poor. 01:46 On the right hand side, we're demonstrating esophageal varices. 01:49 So these very dilated Porto esophageal connections with very minimal epithelium over them. 01:56 And you can imagine a potato chip going down there and eroding the epithelium and now you would have a massive bleed. 02:03 How are we going to make the diagnosis? Well, we're going to look at a variety of laboratory studies. 02:09 But also it's going to be based on history, obesity, or alcohol, or hepatitis, in most cases is going to be our underlying etiology. 02:19 Early findings in cirrhosis in the laboratory diminished platelet count. 02:23 Some of this is due to hypersplenism. 02:25 But the other part of it is the liver, is the source of thrombopoietin. 02:31 And if liver doesn't make that, you don't make adequate platelets. 02:37 The AST and the ALT are going to be elevated. 02:41 So these are going to be markers of hepatocyte injury, those are transaminases that are involved in normal liver metabolism as hepatocytes die, they release those enzymes and we can detect them in the blood. 02:55 Now, in the later stages of cirrhosis, when the patient is going to be more symptomatic with other things that we've already talked about. 03:03 You may actually have normal or even low levels of AST/ALT. 03:07 That means that we've pretty much killed all the liver parenchyma that we can or that we will and so we don't see release of those enzymes. 03:17 We will see that the partial thromboplastin time and the prothrombin time, so PTT and PT are elevated. 03:25 That means that the international normalization ratio, the INR will also be up and that's because of the inability to synthesize the normal coagulation factors. 03:34 Bilirubin will be up and it may be both direct and indirect. 03:38 Glucose will be down because we don't have the ability to store glycogen and albumin will be way down. 03:45 We can also do some imaging. 03:46 So typically on ultrasound or CT, we will see a small granular or smaller more granular looking liver. 03:54 And what's been demonstrated here is actually an angiogram showing the formation of a Caput medusae. 04:00 The arrow is pointing to this dilation of the systemic vasculature around the umbilicus. 04:07 Cirrhosis is shown in a intact liver from an autopsy on the left hand side. 04:14 You see nodules of regenerating hepatocytes and intervening zones with depression that's the scarring. 04:22 We can see on histology, the correlation to that. 04:25 This is not your typical H and E stain, this is a trichrome stain. 04:30 And in the stain, the fibrosis, the scarring is blue. 04:34 So you can see that there are numerous regenerating nodules throughout those are kind of pink with more white, the whiteness there is actually steatosis because this was a drinker who kept drinking, so ended up with alcoholic steatosis. 04:48 But then you have outside the regenerating nodules, all this bridging fibrosis. 04:53 And by seeing this image, hopefully you can appreciate why there would be abnormal flow into this liver, blood supply wise, and abnormal flow out of the liver in terms of say bilirubin, but also why we have diminished synthetic function. 05:07 So what are we going to do about this? I've already said a couple of different times that this is end stage, there is no going back, the liver will not ever get back to normal, and we're stuck with whatever level of cirrhosis is already present. 05:20 We want to minimize accumulating any more. 05:23 And we want to avoid things that will injure whatever residual hepatocytes are present. 05:28 So we're going hepatotoxic substances, alcohol, acetaminophen, things that can potentially injure the liver. 05:35 For the secondary manifestation, the varices, were going to band those, basically put a rubber band around them, and then they will thrombose. 05:44 Or, if necessary, we can do vascular shunts. 05:47 So there's a procedure by which we can put in by interventional radiology, a shunt, that takes blood from the portal vein and goes right into the inferior vena cava. 05:58 In that way, we reduce the portal hypertension, of course that shunts, the materials coming out of the GI tract directly into the brain. 06:08 So encephalopathy may be exacerbated. 06:12 For severe ascites, we'll give diuretics and salt restriction and paracentesis literally pull off the fluid. 06:17 For the encephalopathy, it turns out if we reduce the amount of protein in their diet, so we reduce the ammonia that we can reduce the encephalopathy. 06:27 However, since patients with cirrhosis are often malnourished, protein intake restriction is no longer recommended. 06:34 One of the other ways we can do it is a laxative called lactulose, which causes increased quicker transit time through the GI tract so we don't get as much absorption. 06:48 And it also will reduce the bacterial content because they're clearly also a source of protein. 06:54 Coagulopathies are treated with vitamin K, we give as much support as we can for whatever the liver can synthesize. 07:03 And in end stage disease, we will do liver transplant. 07:07 Now you won't transplant someone if they continue to be a drinker, you won't transplant someone if they won't lose weight because then the same disease will recur in the new liver. 07:20 And the liver transplant is expensive, limited resources and requires constant then surveillance for the possibility of rejection. 07:29 So we won't treat with a liver transplant unless the patient is willing to play fair with us and to be a good citizen. 07:41 how do we decide whether or not we want to who's going to get a liver transplant. 07:46 So there is a Child-Pugh score, it's based on various biomarkers and signs. 07:51 Not important that you be able to rattle this off on the tip of your tongue but just be aware that we do have these criteria upon which we can decide life expectancy and the need for liver transplant. 08:09 With that, we will conclude and you've learned quite a bit in just about 10 minutes on cirrhosis.
About the Lecture
The lecture Cirrhosis: Clinical Presentation, Diagnosis, and Treatment by Richard Mitchell, MD, PhD is from the course Disorders of the Hepatobiliary System.
Included Quiz Questions
What leads to jaundice in cirrhosis?
- Bilirubin deposition
- Bile salt deposition
- Lead deposition
- Lead poisoning
- Portosystemic shunting
What leads to telangiectasia in cirrhosis?
- Hyperestrogenism
- Bilirubin deposition
- Bile salt deposition
- Portosystemic shunting
- Lead overload
Which of the following is a laboratory finding in cirrhosis?
- Prolonged PT
- Decreased INR
- Decreased bilirubin
- Increased platelet count
- Decreased AST
What are the steps in the management of cirrhosis? Select all that apply.
- Avoidance of hepatotoxic substances
- Banding of esophageal varices
- Lactulose for encephalopathy
- Salt restriction for encephalopathy
- Paracentesis for varices
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |