Playlist
Show Playlist
Hide Playlist
Alpha-1 Antitrypsin Deficiency
-
Slides GIP Alpha-1 Antitrypsin Deficiency.pdf
-
Download Lecture Overview
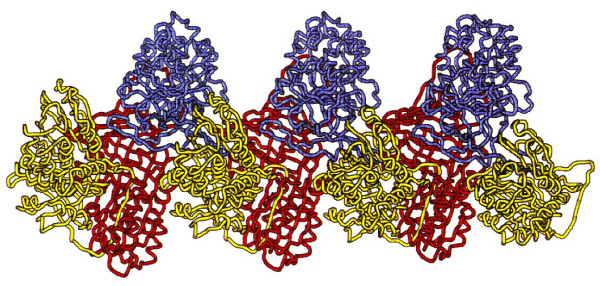
00:01 Welcome, in this talk, we're going to be covering an entity called Alpha-1 Antitrypsin Deficiency, or AAT. 00:08 This is going to be a disorder that largely affects the liver but can also have manifestations in the lung. 00:15 Alpha-1 antitrypsin deficiency is an autosomal disorder, resulting in reduced production and function of the protease inhibitor Alpha One antitrypsin AAT. 00:27 Let's look at the epidemiology. 00:29 So this is not super common, but it's something that you should recognize about 1 in 2000 live births is the incidence. 00:38 It can be diagnosed as early in life as two months of age, and is the most common genetic cause of pediatric hepatic pathology. 00:47 It can lead to chronic liver disease. 00:49 Patients with Alpha-1 antitrypsin deficiency can develop cirrhosis. 00:53 But also importantly, it is a cause of emphysema, and typically emphysema occurring either at an earlier age than one would expect or in a nonsmoker. 01:06 So what's the pathophysiology of this? The severity overall of the disease depends on the genotype of the protease inhibitor SERPINA1. 01:20 And if you make more of the SERPINA1, you are in better shape. 01:24 If you make less of it, or it's functionally impaired in terms of its protease inhibitory activity, you're in worse shape. 01:32 So this is an autosomal gene, the SERPINA1, and it is an autosomal recessive disease. 01:39 So if you just have one mutated copy, in the vast majority of cases, you're fine. 01:43 But if you have one mutated copy from mom, and even a different, mutated copy, mutated in a different region from dad, then you are at increased risk. 01:58 Pi stands for protease inhibitor. 02:01 So this is an ancient nomenclature. 02:04 It's based on what we can do in terms of protein electrophoresis. 02:09 So this is before we understood what was going on, but we will look at various proteins. 02:14 So Pi is protease inhibitor, and MM is the wild type. 02:18 So that's the normal 100% level of expression of a normal functional SERPINA1 protein. 02:26 The typically mutated alleles are called S and Z. 02:30 There are other mutations, there are actually a whole bunch of different mutations, but we're going to just look at S and Z. 02:35 If you are P i M and S that means you're a heterozygote. 02:38 You will have about 80% of the level of expression. 02:42 And in most cases, you will have a modest increase for lung disease but not really significant. 02:47 But if you're PiSS, so to mutated alleles, or PiMZ or PiZZ, Z is actually the lowest level of expression and is going to be the most severe disease. 03:01 So you can kind of work through in your own mind if I'm PiMS or PiSS, and I'm gonna say what that spells, PiMZ, PiSZ, etc, those are all going to be about 50% activity. 03:16 And then if you are PiZZ, so the least level in the least functionality of the protein, you have the most severe disease involving both the lung and the liver. 03:29 So the mutated gene is making a protein the Alpha-1 antitrypsin, the gene may also have impact on how much has been synthesized, but the normal protein has to go through a conformational folding that goes on and rough endoplasmic reticulum, and then it is excreted from the cell. 03:52 If there are mutations, there's misfolding that tends to retain the abnormal misfolded protein within the endoplasmic reticulum. 04:01 So this is just a demonstration of that happening. 04:04 The misfolded Alpha-1 antitrypsin is retained in the grid and in the endoplasmic reticulum and if you have a relatively low level of this, if you're a heterozygote, your ER in your liver is more or less able to accommodate that. 04:20 However, if you have significantly elevated levels of misfolded protein or certain forms of misfolded protein that trigger more of the misfolded protein response, the ER stress response, then you can get apoptosis of the hepatocyte. 04:38 The liver cell just gives up because it says we are unfortunately overwhelmed with misfolded protein. 04:45 And if you're interested in this process, I refer you back to the basic cellular pathology talks that are elsewhere within the Lecturio portfolio. 04:56 Now, that's what's going on in the liver, and that's why you can have cirrhosis and liver damage. 05:02 But what about not making enough of this normal protein to get out into the circulation? Well, normal Alpha-1 antitrypsin is an anti protease. 05:12 It's going to protect alveoli and other tissue structures from the noxious effects of released exoproteases, from neutrophils. 05:22 So neutrophil elastase and some of the other proteases are inhibited by Alpha-1 antitrypsin. 05:28 If you don't have enough of that, every time you release neutrophil activity, you will get more damage than you would otherwise normally get. 05:36 And when this happens in lung, this is going to give rise now to emphysema with big dilated airspaces due to the effects of elastase degrading the normal interstitium. 05:49 How does this clinically present? So it presents in two different organs at kind of two different times. 05:54 In the liver, with patients who are going to have severe disease, it's usually neonatal within the first few months. 06:01 There is impaired coagulation factor synthesis, so there's bleeding, there'll be bleeding from the umbilical stump, from the GI tract, from the intracranial space. 06:08 So injury, trauma associated with childbirth may lead to bleeding around the brain, or any unexplained bruising. 06:15 So it's kind of a signal that something may be going on with regards to a liver. 06:21 There will also be inflammation of the liver due to the ongoing injury and a hepatocyte death. 06:30 And then we're also going to get cholestatic jaundice. 06:32 So the baby will be bleeding, and will be yellow. 06:35 Again, additional liver findings in the pediatric population. 06:39 It is a progression to cirrhosis. 06:41 And if you want to know about cirrhosis, that is another talk within this GI pathophysiology series. 06:48 There will hepatomegaly, splenomegaly, ascites, esophageal varices, scleral icterus. 06:54 And if you're interested in any of those, go to that other talk on cirrhosis. 06:59 In the lungs, now this is not in the neonatal period, but in later life, there will be beginning in the second third and fourth decade of life, signs of emphysema, coughing, dyspnea, chronic sputum production, wheezing associated with a loss of interstitial parenchyma. 07:16 How are we going to make the diagnosis? This is going to be largely based on: one, clinical suspicion, but two, we're going to do testing looking for the levels of Alpha-1 antitrypsin in the bloodstream. 07:29 We will then do a genetic analysis and try to assess whether we have an S mutation or a Z mutation, and whether we have a heterozygote or homozygote. 07:39 We want to clearly assess for the degree of pulmonary disease in addition to the liver disease, and liver disease, we're gonna look at a variety of liver markers. 07:49 But we're also going to do a biopsy. 07:50 And this is just showing you a very characteristic appearance on the liver biopsy. 07:55 It is a periodic acid-Schiff stain or a PHS shiff stain that is highlighting glycoprotein. 08:01 And what we're seeing in the hepatocytes are these big pink globules. 08:06 Those are misfolded, Alpha-1 antitrypsin glycoprotein within the endoplasmic reticulum, and cells that have these big accumulations will eventually undergo apoptosis, due to the ER stress response and they will die. 08:23 How are we going to manage this? So it's going to be supportive treatment. 08:26 For lung disease, we're going to want to give vitamin E and that's thought to reduce the amount of inflammation and free radical damage that is going on in the lungs. 08:36 That is not really supported by studies but it doesn't hurt. 08:40 We will want to have the patient stop smoking because smoking will recruit the neutrophils which will release - which will exacerbate the emphysema and we don't want that. 08:52 We will try to prevent them getting infections. 08:55 So every vaccination possible against a respiratory illness, influenza pneumococcus, COVID, other things will be something that we recommend and strongly try to enforce. 09:07 And we also want to minimize if at all possible any injury to the liver from other sources, such as hepatitis. 09:18 For pulmonary form only. 09:19 So, in many of the patients who have Alpha-1 antitrypsin deficiency, the accumulation of the protein in the liver is not sufficient to trigger the ER stress response. 09:33 And so the liver is largely okay, but they can still have severe lung disease. 09:37 So for those pulmonary forms, only we can give exogenous Alpha-1 antitrypsin. 09:43 For very severe forms, patients may be eligible for liver and or lung transplantation. 09:50 So with that, an uncommon entity that you should recognize and it has a really interesting kind of pathophysiology: Alpha-1 antitrypsin deficiency.
About the Lecture
The lecture Alpha-1 Antitrypsin Deficiency by Richard Mitchell, MD, PhD is from the course Disorders of the Hepatobiliary System.
Included Quiz Questions
What is the inheritance pattern of A1AT deficiency?
- Autosomal codominant
- Autosomal dominant
- X-linked recessive
- X-linked dominant
At what stage of development does liver damage typically manifest in individuals with A1AT deficiency?
- Neonatal
- Adult
- Teenager
- Senior
In which decade of life do the pulmonary symptoms of A1AT deficiency present?
- Third or fourth decade of life
- Send decade of life
- Fifth or sixth decade of life
- Seventh decade of life
- Eighth or ninth decade of life
Which of the following is NOT a component of the management of A1AT deficiency?
- Vitamin A
- Vitamin E
- Smoking cessation
- Vaccination
- Replacement therapy
Which statement about the management of A1AT deficiency is true?
- Liver and lung transplantation are treatment options for severe disease.
- Liver transplantation, but not lung transplantation, is a treatment option for severe disease.
- Lung transplantation, but not liver transplantation, is a treatment option for severe disease.
- Lung transplantation is a treatment option for newly diagnosed patients.
- Liver transplantation is a treatment option for newly diagnosed patients.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |