Playlist
Show Playlist
Hide Playlist
Management of Osteoporosis in Women
-
Slides Osteoporosis Menopause.pdf
-
Download Lecture Overview
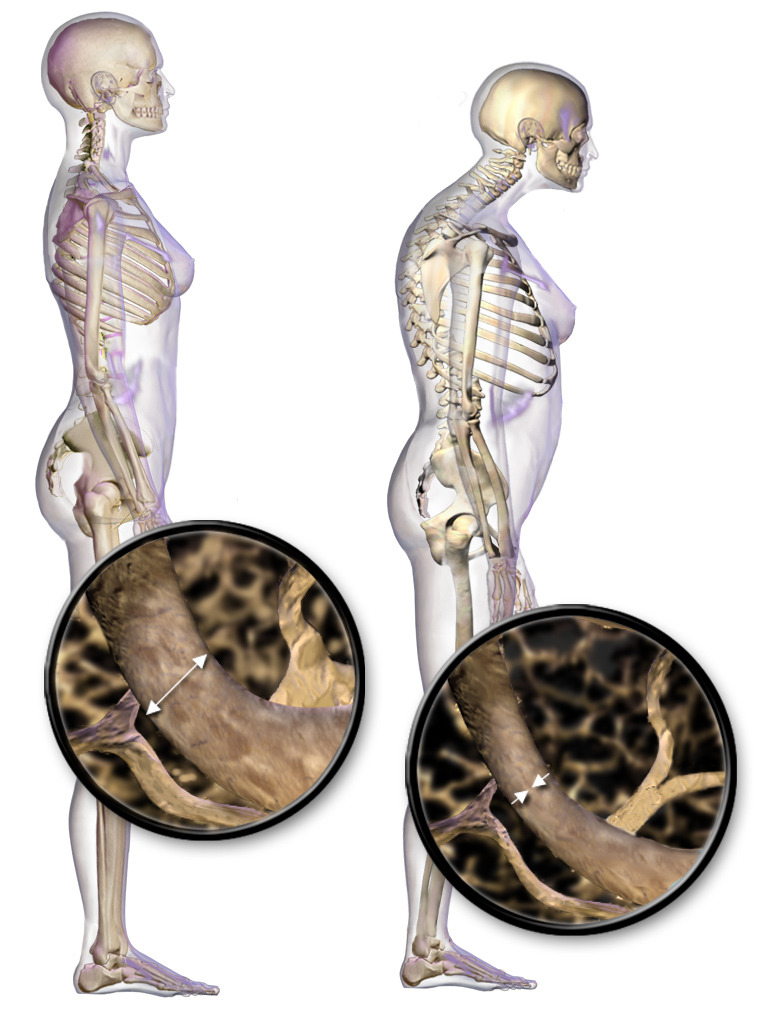
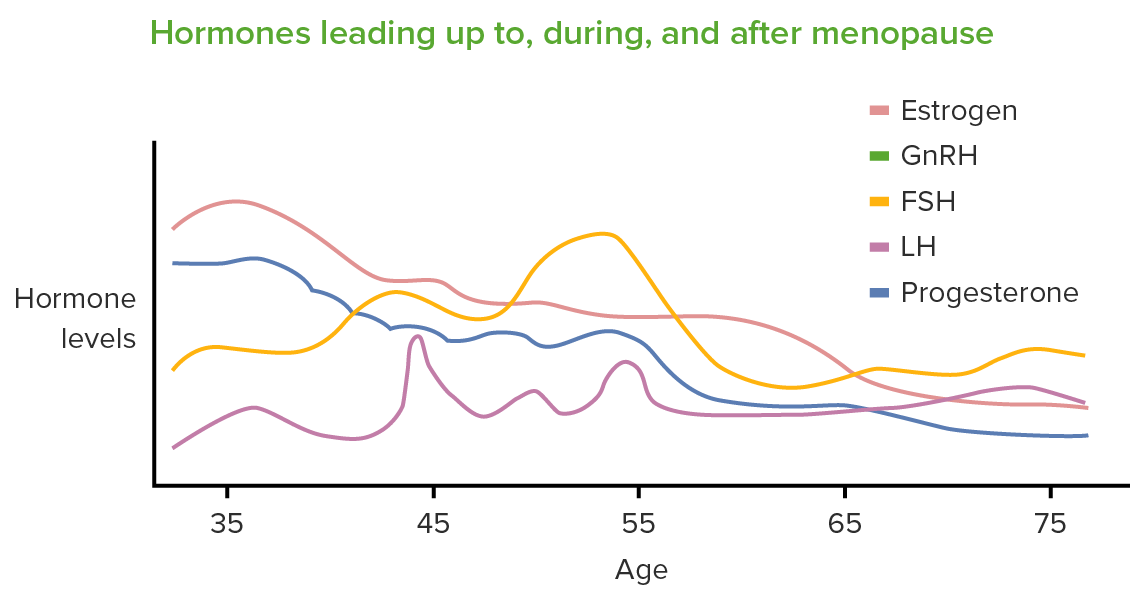
00:01 Hi, let's now go over the treatment for Osteoporosis. 00:05 The first line pharmacotherapy is usually a bisphosphonate. 00:10 It can be taken orally or IV. Other therapies include calcitonin, denosumab, raloxifene, or teriparatide. There are some clinical criteria that would encourage you to actually initiate therapy, hip or vertebral fracture, major osteoporotic risks including a growth of 3% risk of hip fracture or an overall risk of fracture of more than 20%. 00:38 Also, low bone mass would also alert the clinician that the patient needs to be started on medical therapy. 00:45 There are FDA-approved options and there are different categories. 00:49 Let's first review antiresorptives or bone-retaining medications. 00:55 Bisphosphonates fall into this category, also, calcitonin as well as SERMS. 01:01 We've reviewed SERMS in another lecture. 01:03 Also, hormone replacement therapy which we've also reviewed in another lecture. 01:09 There are anabolic options as well. These are bone-forming options and this includes PTH which is also called teriparatide. 01:20 Also, human monoclonal antibody to the RANK-ligand which is cause of the pathophysiology of osteoporosis. 01:29 Let's review bisphosphonates. In the US, we have alendronate, ibandronate, and risedronate, as well as zoledronic acid. 01:39 These are classified as antiresorptive medications. 01:43 They bind the hydroxyapatite crystals in the bone as well as osteoclast and inhibit osteoclast activity. 01:52 They inhibit resorption of the bone and may lead to increased bone density and reduced fracture risks. However, I'd like to tell you that these medications can stay within the bone for 10 years and we are not sure how they could affect a woman or developing fetus during pregnancy. 02:11 So if the woman has done her reproduction then perhaps, that's when you should initiate these therapies and not before if she's considering pregnancy. 02:20 But overall, these medications do reduce the fracture risk. 02:26 Let's now review the side effects of bisphosphonates. 02:30 You can have hypocalcemia, abdominal pain, bone, joint, or muscular pain, you can also have inflammation of the eye or other eye disorders, women who take these medications may develop a rash or allergy, renal dysfunction, also one that you may have heard about in the news is osteonecrosis of the jaw, we'll review that in just a moment. 02:57 Atrial fibrillation is also another important and very morbid side effect, and we can find that these patients have atypical subtrochanteric fractures and that is still under review by the FDA. 03:14 Let's now look at osteonecrosis of the Jaw, not a pretty picture. 03:20 However, if patients present with this, they need to stop therapy immediately. 03:25 Fortunately, osteonecrosis of the jaw has a very low incidence. 03:29 It's most likely to occur in cancer patients who are receiving high doses of IV bisphosphonates. 03:35 It's rarely diagnosed in patients who are on oral bisphosphonates. 03:40 In 2005, the FDA required a statement about osteonecrosis of the jaw as a risk factor for all bisphosphonates. 03:48 Let's now talk about esophageal cancer. 03:53 Recall that an oral bisphosphonate needs to be taken by a patient who can sit upright for 30 minutes. 03:59 There might be some esophagitis that occurs as a result of taking bisphosphonates orally. 04:05 You can have other side effects with IV bisphosphonates. 04:10 Anything that you take IV can cause flu-like symptoms which might be an auto-immune phenomenon. 04:16 They can also cause arthralgia which is pain in the joints. 04:20 Headache is also a common complaint, as well as fever and myalgia which are generalized body aches. With IV bisphosphonates, you can have calcium, creatinine, and 25OHD levels that should be checked before you initiate therapy. 04:36 Let's now review the women's health initiative study. 04:42 They did show that with hormone replacement therapy that there was a 34% reduction in hip fracture risk, there was a 34% reduction in clinical vertebral fractures, a 24% reduction in osteoporosis-related fractures, and estrogen alone was similarly effective to reducing fracture risk throughout the skeleton. 05:05 So who should get hormone replacement therapy? Women who are at risk for osteoporosis should be considered for hormone replacement therapy. 05:13 Let's now think about who's at risk for osteoporosis. 05:17 Well, a woman who is thin, smokes, Caucasian, a person who has been on life-long glucocorticoids, those are all risk factors so perhaps we should discuss HRT with those women. 05:30 But why' Why would you give women a hormone replacement therapy? We've reviewed hormone replacement therapy and how it works in another lecture but based on the study from the Women's health initiative, we know that HRT prevents fractures. When' When should you give it? Well, you should give it within five years of menopause. 05:50 We have another lecture that talks about menopause and we know that the average age is at 51 years old. 05:57 What and how long? Well, there's lots of different preparations and that's addressed in the hormone replacement therapy lecture. 06:05 Usually, five years, but it's an individualized decision based on what the patient needs and the risk factors that are present. 06:13 Let's now talk about combination therapy. 06:16 Candidates for combination therapy include patients who are already been on an antiresorptive agent for two years, who continue to have bone loss despite treatment, or they have fractures after being on treatment, or they have a persistent low bone mineral density. 06:32 How can we prevent osteoporosis in our patients? Well, we should consider lifestyle modifications. 06:41 If they're smoking, they should stop. If they have a poor diet, you should actually encourage the patient to actually eat foods that are high in calcium and vitamin D, or take supplementation. 06:53 Also, early intervention. Recall that I discussed that maximal bone density occurs during adolescence so primary prevention should actually occur during the adolescent period. Let's now talk about calcium supplementation. 07:07 When a child, a young girl is young. She should be taking 500 milligrams a day. 07:13 Usually, a toddler or an infant will get this through milk. 07:17 When she's a bit older and she starts school, she still needs maximal calcium intake, this time at 800 milligrams per day. 07:26 As she heads into adolescence and puberty occurs, she should be taking 1,300 milligrams per day. 07:33 As she gets older, closer to the menopause, you can reduce that to 1,000 milligrams per day. 07:40 But after menopause and the average age is 51, that should go back up to 1,200 milligrams per day. 07:47 Let's talk about the foods that actually contain calcium. 07:50 Oftentimes, we tell our patients to eat dairy. 07:53 However, there are lots of patients who are lactose intolerant, have an allergy to dairy, or just simply don't want dairy in their diet. 08:01 However, if they can tolerate dairy, yogurt is a good way to improve calcium in your diet. Sardines with bones in oil are another good way. 08:10 Cheddar cheese, another dairy product is also excellent. 08:15 Milk, any form of milk actually is good. 08:19 Tofu, this is helpful for our vegan and vegetarian patients who find it difficult to include dairy in their diet. 08:27 Many fruit juices in the US are actually supplemented with calcium. 08:31 However, too much juice intake can lead to other health problems and this should be limited. Salmon is another good way to include not only calcium, but also some vitamin D through the fish oils that are present. 08:43 Most cereal in the US also has been fortified with other vitamins and minerals including calcium. Turnip greens which are actually my favorite are very good to include calcium into your diet. 08:55 Ice cream, either low-fat or high-fat is another good way. 09:00 And again, for our vegans and vegetarians, soy milk that is fortified with calcium is another good way to include calcium into your diet. 09:08 I'd like to now talk about vitamin D. 09:10 This is an essential vitamin for the absorption of calcium from the GI tract. 09:14 It may help in bone metabolism as well. Calcitriol or 1,25-dihydroxvitamin D3 is the biologically active form of vitamin D but this should not be measured to assess deficiency. Actually, what we do measure and practice is 25-hydroxyvitamin D. We should maintain blood concentrations of 25-hydroxyvitamin D of 30 nanograms per mL or higher. 09:40 Less than that is actually insufficiency from 20 to 30 nanograms and less than 20 is actually deficiency. 09:47 You find that people who are vitamin D deficient who live in regions where it may be cold and not have a lot of sunshine, and you also find vitamin D insufficiency and deficiency in people who have darker skin tones who may not absorb the sun in those conditions. 10:03 So as we age we need more vitamin D. 10:08 Those 50 and older need at least 800 to 1,000 IUs per day of vitamin D, those under 50 need about 400 to 800 IUs of vitamin D. 10:19 Supplementation is advisable for many individuals. 10:22 It can be synthesized in the skin upon exposure to sunlight, but of course the recommendation is that we wear sunscreen and sunblock, and that actually prevents production. Skin production of vitamin D with sunlight actually declines with age. Let's now look at fall prevention. 10:41 As a woman ages, her increased risk of hip fracture can actually be very morbid for her overall health. So we should ask about proper accommodations in the home to prevent falls. So if a patient doesn't have handrails on stairs or in bathrooms, you need to encourage her to actually have those installed. 11:02 If she cannot afford it there may be some programs available through the state to help accommodate her home. Also, you should encourage the patient to keep her floors clean but not slippery. Slippery floors can lead to falls, and falls can lead to fractures. You should also encourage the patient to eliminate clutter on the floors as tripping can also lead to fractures. 11:26 The home should be well lit with 100 watt light bulbs that are installed everywhere to help illuminate the home. That also can prevent falling which can actually lead to fractures. Use skid proof rugs with rubber bath mats so that a patient does not slip and fall. 11:45 This should be implemented in the hospital as well as patients may be disoriented and have increased risk of fracture. 11:52 Thank you for listening and good luck on your exam.
About the Lecture
The lecture Management of Osteoporosis in Women by Lynae Brayboy, MD is from the course Menopause. It contains the following chapters:
- Bisphosphonates
- For Strong Bones
Included Quiz Questions
Which of the following is NOT part of the first line of treatment for osteoporosis?
- Selective estrogen receptor modulators
- Bisphosphonates
- Calcitonin
- Denosumab
- Teriparatide
Which of the following bone-forming drugs is approved by the FDA?
- Teriparatide
- Bisphosphonates
- Calcitonin
- Selective estrogen receptor modulators
- Estrogen therapy
Which of the following is NOT a side effect of use of bisphosphonates?
- Flushing of face and hands
- Hypocalcemia
- Osteonecrosis of jaw
- Muscle and joint pains
- Uveitis
Which of the following is associated with the use of bisphosphonate therapy?
- Esophageal cancer
- Stomach cancer
- Colorectal cancer
- Prostate cancer
- Breast cancer
What is the mechanism of action of bisphosphonates?
- Inhibit osteoclast activity
- Inhibit osteoclast activity Estrogen agonist activity
- Increase in osteoclast activity
- Estrogen antagonistic activity
Which of the following age groups requires about 1000 mg of daily calcium intake?
- 19 to 49 years
- 9 to 18 years
- 4 to 8 years
- 1 to 3 years
- More than 50 years
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |