Playlist
Show Playlist
Hide Playlist
Referred Pain
-
Slides Referred Pain.pdf
-
Download Lecture Overview
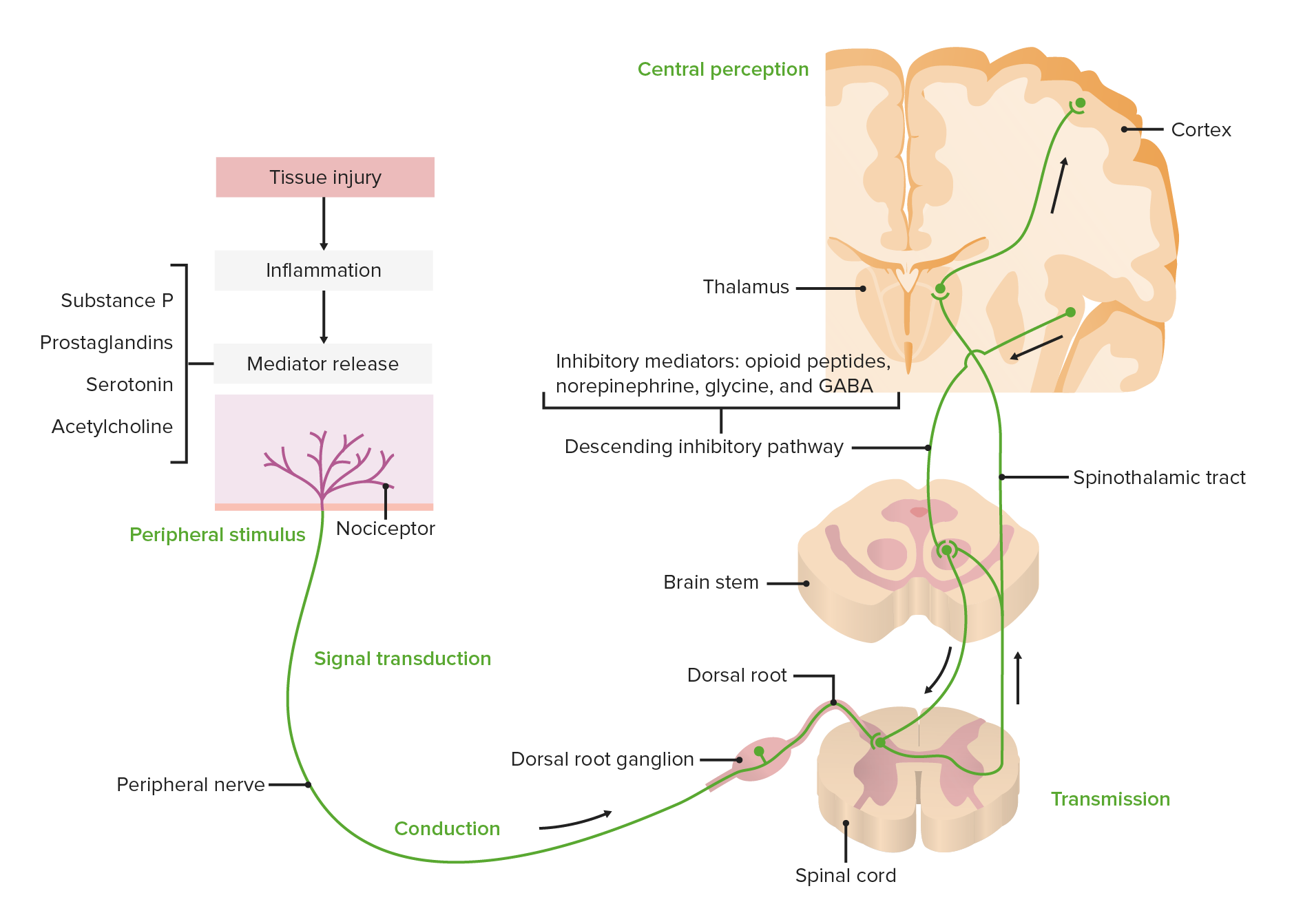
00:01 So let's spend some time looking at referred pain. 00:05 So let's go first of all, and look at the somatic nervous system. 00:09 So here we can see we've got a spinal nerve. 00:12 And if someone was to apply pressure or pain, or to touch the surface of the skin, then that cutaneous branch of that somatic spinal nerve would receive that stimulus, and it will pass it back towards the spinal cord. 00:26 Now, once it's gone back to the spinal cord, that will be highly localized to a specific dermatome. 00:33 And that'll be relayed to the brain that sensation has come from that specific area of the skin. 00:39 However, if there was sensation coming from the organ, then you don't actually have that physiological sensation picked up. 00:48 Because imagine if you could sense the movement of the stomach and the intestines as we're digesting food. 00:54 So, the brain doesn't appreciate that movement and that sensation coming from various physiological instances. 01:01 Although, there is a afferent pathway that comes back to the spinal cord to help regulate the process. 01:08 It's not a pain to such pressure sensation during normal physiological instances. 01:14 But we can see how that afferent fiber is going to run alongside the splanchnic nerves back to the sympathetic trunk, and ultimately to the spinal cord. 01:23 However, if there's some sort of pathological stress, inflammation, for example, then that can actually become such a strong visceral stimulus that the brain recognizes it. 01:35 It's not able to just remove it from its consciousness because it's going on a daily occurrence. 01:41 If something unusual occurs, some pathological state, then it breaches a threshold, which means the brain is now consciously aware. 01:49 But because it's not used to having this sensation coming from this region, it is often poorly localized. 01:57 The brainstem and the central nervous system cannot actually understand precisely, unlike the distribution of the dermatome, where it's come from. 02:06 So this is where you have referred pain. 02:09 You have the pain, but you can't pinpoint is exact location. 02:14 So it refers it to a specific area of the skin, which may not be the precise location that that organ is under pathological stress. 02:24 So eventually, it will be localized to a dermatome, but it won't be as acutely located as with the somatic nervous system. 02:33 So let's use an example of appendicitis. 02:36 Now, the appendix is located at roughly at McBurney's point. 02:39 Two-thirds to 1/3 of the way between the umbilicus and the anterior superior iliac spine. 02:45 So if he were to have an appendicitis, you'd expect perhaps, to have the pain directly in that position. 02:51 But because the body is not aware of that location, unlike the somatic nervous system, it tends to localize around the umbilicus within the kind of tummy region, and you'll come with central abdominal pain. 03:03 But over time, it will eventually start localizing to that right lower quadrant. 03:09 Initially, it's referring it to the central tummy region. 03:13 Over time pain will then be located around that right lower quadrant.
About the Lecture
The lecture Referred Pain by James Pickering, PhD is from the course Lymphatics and Nerves of Abdominopelvic Region.
Included Quiz Questions
Which statement is correct about referred pain and visceral pain?
- Visceral stimuli are poorly localized.
- Somatic stimuli are poorly localized.
- Visceral stimuli are associated with sensation in physiological instances.
- Inflammation is not associated with visceral stimuli.
- There is no sensation associated with a visceral stimulus.
Where is McBurney point?
- One-third of the distance from the right anterior superior iliac spine to the umbilicus
- Two-thirds of the distance from the right anterior superior iliac spine to the umbilicus
- One-half of the distance from the right anterior superior iliac spine to the umbilicus
- One-half of the distance from the left anterior superior iliac spine to the umbilicus
- One-third of the distance from the left anterior superior iliac spine to the umbilicus
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |