Playlist
Show Playlist
Hide Playlist
Hereditary Hemochromatosis: Epidemiology and Pathophysiology
-
Slides GIP Hereditary Hemochromatosis.pdf
-
Download Lecture Overview
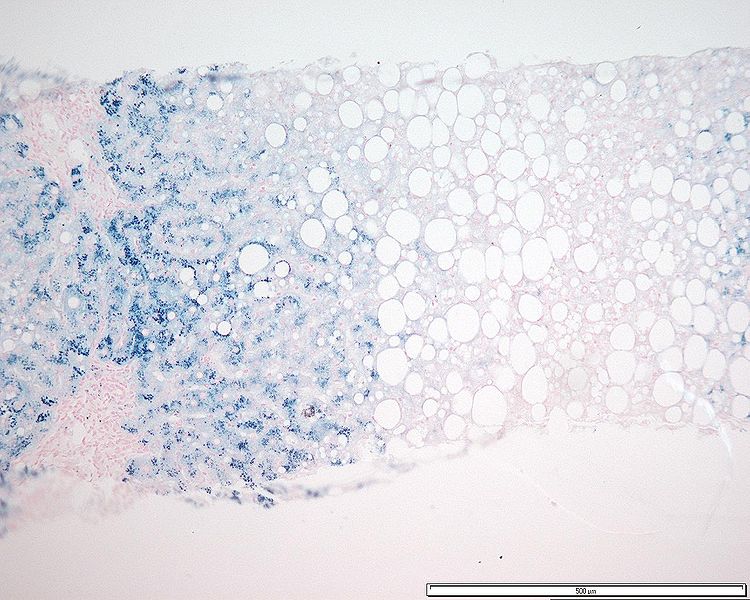
00:01 Welcome. 00:02 With this talk we're going to be covering a rather interesting topic of hereditary hemochromatosis. 00:09 Hereditary hemochromatosis, or HH is an autosomal recessive disorder. 00:13 And it's caused by gene mutations primarily in the iron sensing apparatus in the liver. 00:20 That will lead in turn to a low production of hepcidin, which is the major hormone that regulates systemic levels of iron. 00:27 And if we don't make enough hepcidin, because we're not sensing it appropriately, that results in increased iron absorption. 00:35 Let's cover some of the epidemiology. 00:37 It is a reasonably common entity, HH. 00:42 It's about one and 200 to 500 people, it's much more common people of Celtic or Nordic origin, the most common mutation is a cysteine to a tyrosine substitution at amino acid 282 is called C282Y. 00:57 And it's in the HFE protein, otherwise known as the human homeostasis iron regulatory protein that's going to be part of the sensing apparatus in the liver. 01:07 That's the most common mutation in patients with HH. 01:11 In about 85% of patients will be homozygous for the C282Y mutation. 01:18 You probably don't need to memorize the exact mutation. 01:22 But you do need to understand that this is in the sensing apparatus in the liver and the liver is going to be the major overall regulator of iron levels. 01:30 It's also the liver is going to be one of the major organs most negatively impacted by too much iron. 01:40 Overall, HH is going to be much less common in people of African descent, it occurs more frequently or seen and expressed more frequently in men than in women. 01:50 That's probably in part because women who go through regular menstrual cycles are regularly losing blood, and therefore don't have an iron accumulation. 02:02 The age of onset in men is after the age of 40. 02:05 So it takes a while for you to accumulate iron to the point that you become symptomatic. 02:10 In women, it's going to be after the childbearing years after they're no longer menstruating where they can now accumulate the iron. 02:17 There is a form of HH that's juvenile hemochromatosis, or the onset is at a much earlier age. 02:25 The pathophysiology. 02:27 So the common missense mutation is just a change from one amino acid to another as the cysteine 282 to a tyrosine. 02:35 There are other mutations in the same sensing protein, the HFE protein, such as a histidine, to aspartic acid and amino acid position number 63, both of these change the ability of that protein to participate in the iron sensing apparatus. 02:54 There are also other non HFE genes. 02:57 So there are several proteins that are involved in the sensing apparatus. 03:01 Most of the other mutations in these other proteins are relatively rare, but they are found in juvenile hemochromatosis, and particularly a mutation or protein called hemojuvelin. 03:14 To really understand what's going on here, we have to understand normal iron homeostasis. 03:20 We have a schematic of the GI tract, and it's connected by the portal circulation to the liver. 03:27 Iron is absorbed in the duodenum about 1-2 mg per day. 03:32 We only lose about 1-2 mg per day. 03:35 So it is a very tightly regulated loss and absorption. 03:43 The absorption is occurring in the duodenum, that's the only place that we get iron absorption, and the iron is being absorbed by the enterocytes by the duodenal epithelial cells. 03:55 What is happening is that a protein called ferroportin on the basal surface of the enteroctyes allows the iron to move from the GI tract from the duodenum where it's been absorbed and into the bloodstream and that iron then binds up with transferrin in is then circulated around the body. 04:16 So we need to have that ferroportin to act as a mechanism to get the iron from the enterocytes into the bloodstream. 04:25 From the bloodstream bound to transferrin and the iron will go to bone marrow into a variety of other tissues. 04:32 So the total iron content is four grams roughly in the body. 04:37 We're only changing about 1-2 mg each day, absorbing and loss. 04:43 Most of the iron ends up going to the bone marrow and his skeletal muscle. 04:48 So in the bone marrow, the iron is going to erythroid precursors eventually going to become red blood cells. 04:56 In skeletal muscle, it's going to myoglobin. 04:59 And basically 70% of the total body iron is in these two areas, red cells and skeletal muscle. 05:07 But there's a substantial amount of iron in other places within the body. 05:11 And in particular, the liver can be a major store. 05:15 It's also going to be a mechanism a buffer, by which too much iron will be taken up and tried to protect the rest of the organs in the body. 05:24 Another place where iron is stored is within macrophages. 05:28 And in both of these storage places, the iron is stored in association with an intracellular protein called ferritin. 05:35 So we're still talking about normal activities, in terms of the iron absorption. 05:40 Here we have our iron within the duodenum, and it is going to be transported via ferroportin. 05:47 Now the liver can say, you know what, everybody, we have enough iron, we don't need any more iron. 05:55 And when we are replete, the liver releases a protein called hepcidin. 06:01 Hepcidin circulates in the bloodstream and when it interacts with ferroportin, it causes the down regulation ferroportin on the basal surface of enteroctyes. 06:12 Hmm. 06:13 Now, iron cannot be transported across into the bloodstream. 06:19 So they hepcidin is now allowing us to keep that iron in the GI tract. 06:23 And when it goes in the GI tract, you just defecate it out and you're not absorbing it. 06:29 And that's how we regulate normal iron. 06:33 However, if we don't have normal sensing, and we don't make hepcidin at the appropriate levels, we won't cause the down regulation of the ferroportin and now the iron happily just keeps going across into the bloodstream at very high levels. 06:50 And we just keep absorbing and absorbing and absorbing. 06:53 So if we don't sense iron appropriately in the liver, or we don't make hepcidin appropriately in response to that iron sensing, then we absorb in the duodenum too much iron. 07:05 When that happens, we have hereditary hemochromatosis. 07:10 So instead of just one to two mg of iron a day, we double that, and that excess iron accumulation accumulates in the liver and again the liver is going to be a very important storage overall for the iron. 07:23 And in many ways we'll protect the rest of the body by taking it up. 07:27 But too much iron is going to end up being pathologic. 07:32 There can be other causes besides a primary defect in sensing or in hepcidin production. 07:39 So secondary iron overload can occur when we just take in too much iron. 07:44 Main way this happens is with increased transfusions. 07:48 We may also have ineffective erythropoiesis where we don't turn over the iron appropriately, and it will accumulate. 07:55 If we lose hepatocyte mass, then we also reduce our capacity to make hepcidin and so in chronic liver disease and cirrhosis, patients will tend to have less hepcidin and tend to absorb more iron as a result. 08:10 The iron regulation is mediated by a variety of proteins. 08:13 The iron sensing involves the HFE gene that we've talked about. 08:17 It involves the transferrin receptor to and involves hemojuvelin and those are the sensing apparatus and then the product when the liver says, we have enough iron is hepcidin. 08:32 Another way to kind of think about this with increased iron, the hepcidin goes up, that reduces the amount of iron that we absorb. 08:40 It's interesting with increased inflammation, hepcidin also goes up. 08:45 And the thought is teleologically. 08:47 This is to limit the iron availability to micro organisms. 08:50 So it turns out, hepcidin is an acute phase reactant. 08:54 And whenever there is systemic inflammation, we tend to reduce iron systemically. 09:01 You may hear of the anemia of chronic disease. 09:05 That's because chronic inflammation leads to increased hepcidin and production and reduced iron absorption. 09:12 If you have increased erythropoietin, that's a signal that we need, and this the signals coming from the kidneys. 09:19 That's a signal that we need to make more red cells. 09:22 In that setting, we want to reduce the hepcidin that so we get more iron absorption and more iron going into the hematopoietic precursors so that we can make more red cells. 09:32 So hopefully this all kind of makes sense. 09:36 In hereditary hemochromatosis, the gene mutations involve abnormal sensing of iron levels in the liver. 09:44 And when they don't sense it appropriately, they don't realize that gee, we're iron replete, we have enough. 09:51 And so there's not enough hepcidin produced and as a result, the duodenum absorbs more iron. 09:58 With increase iron absorption, we get a progressive increase in intracellular iron bound to the ferritin and that's going to be within macrophages, and it's going to be within the liver for the most part. 10:08 But then increased iron results in excessive oxidative stress because basically, it can induce oxygen free radicals, leading to cell injury, and leading inflammation and eventually organ damage. 10:22 Now, the main organs that are going to be affected is where iron tends to accumulate, the liver is going to be a major site of accumulation, but many other organs in the body with excess iron floating around will also eventually accumulate iron. 10:36 So it can go to the brain, it can go to the heart, it can go to the pancreas and go to the skin. 10:41 And we're going to see those manifestations in a moment.
About the Lecture
The lecture Hereditary Hemochromatosis: Epidemiology and Pathophysiology by Richard Mitchell, MD, PhD is from the course Disorders of the Hepatobiliary System.
Included Quiz Questions
What is the inheritance pattern of hereditary hemochromatosis?
- Autosomal recessive
- Autosomal dominant
- X-linked recessive
- X-linked dominant
- Mitochondrial
What best defines hereditary hemochromatosis?
- Iron-sensing mutation that leads to low production of hepcidin
- Iron-sensing mutation that leads to low production of transferrin
- Iron-sensing mutation that leads to high production of hepcidin
- Iron-sensing mutation that leads to high production of transferrin
- Hemoglobin-sensing mutation that leads to high production of hepcidin
What is the most common mutation leading to hereditary hemochromatosis?
- Cysteine-to-tyrosine substitution at amino acid 282
- Cysteine-to-tryptophan substitution at amino acid 282
- Tyrosine-to-tryptophan substitution at amino acid 282
- Tyrosine-to-tryptophan substitution at amino acid 82
- Cysteine-to-tyrosine substitution at amino acid 82
Which of the following is NOT a common or clinically significant location of iron storage in hemochromatosis?
- Lungs
- Skeletal muscle
- Liver
- Bone marrow
- Macrophages
Which of the following can be a cause of secondary iron overload?
- Thalassemia
- Phlebotomy
- Wilson disease
- Hepatosis
- Cooper disease
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |