Playlist
Show Playlist
Hide Playlist
Hepatocellular Carcinoma (HCC) and Liver Metastases
-
Slides GIP Hepatocellular Carcinoma HCC and Liver Metastases.pdf
-
Download Lecture Overview
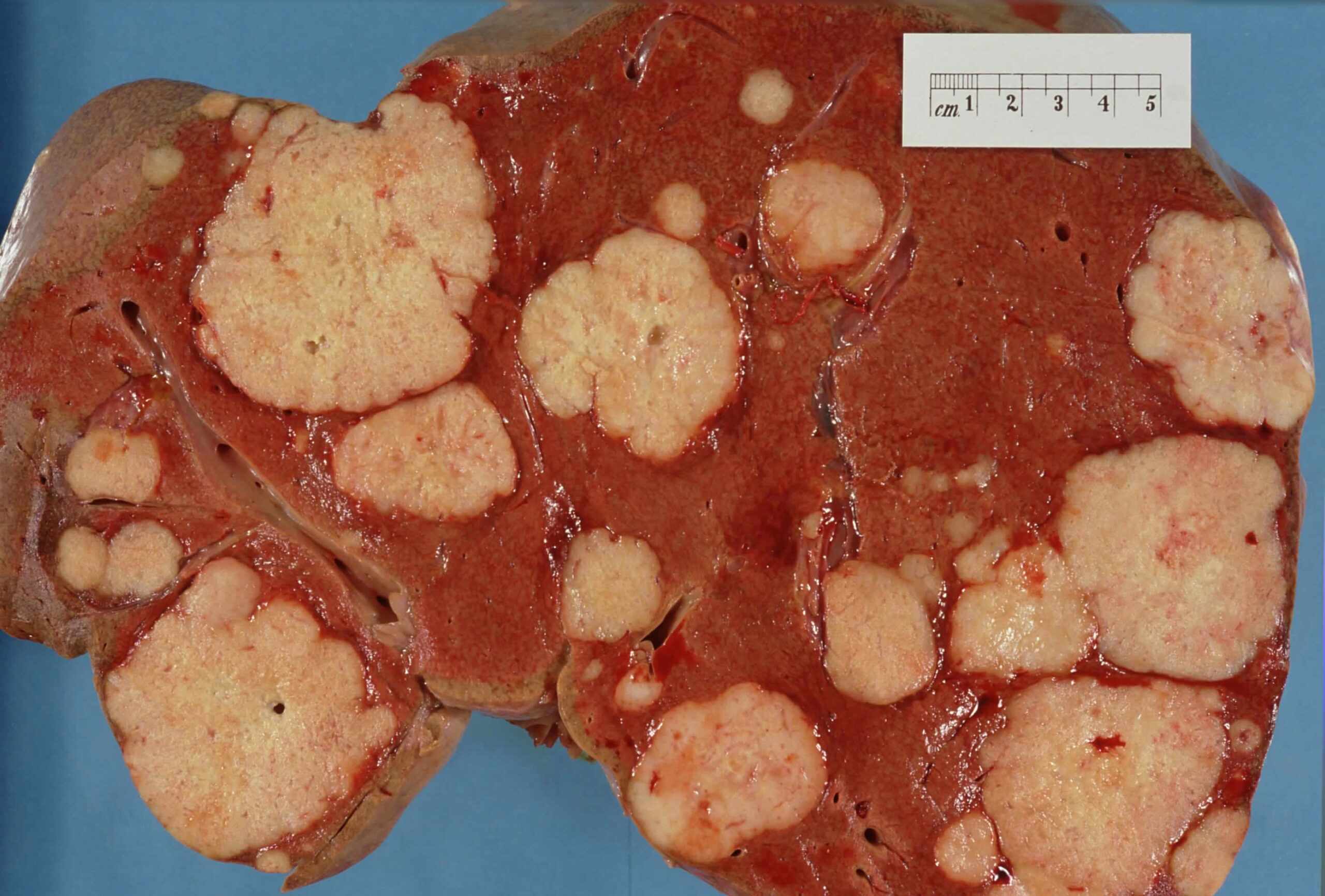
00:01 Welcome! With this talk, we're going to cover cancer in the liver. 00:06 And there's primary cancer in the liver, which is hepatocellular carcinoma, and they're also liver metastases from someplace else. 00:14 As we'll see, liver metastases are much, much, much more common than primary liver cancer, but we'll talk about that. 00:23 Let's do a little epidemiology first. 00:26 So primary, hepatocellular carcinoma accounts for about 90% of primary liver cancers. 00:33 The other primary liver cancers are cholangiocarcinomas for the most part. 00:37 The overall incidence is relatively low. 00:40 So primary hepatocellular carcinoma, only an incidence of about 5 per 100,000 people. 00:46 The vast majority of liver cancers. 00:49 30 times more frequently or metastatic. 00:51 For example, up to about a quarter of colon cancers will metastasize to the liver. 00:57 And overall malignancy in the liver, primary or secondary is the fourth most common cause of all cancer deaths because we lose liver function. 01:08 We're going to talk mostly about hepatocellular carcinoma in this part at the very end, we will return to talk about metastatic cancer. 01:16 But let's talk here about risk factors for HCC. 01:20 Cirrhosis of any cause, confers about a 35% lifetime risk of developing primary hepatocellular carcinoma. 01:29 So you want to avoid cirrhosis. 01:31 Cirrhosis can be due to infections such as hepatitis B or C and can be non alcoholic fatty liver disease, alcoholic liver disease, iron overload, hemochromatosis, copper overload, Wilson's disease, Alpha-1 antitrypsin deficiency, and there are other causes of cirrhosis, including autoimmune hepatitis etc. 01:54 The other causes to be considering in terms of driving hepatocellular carcinoma are primary toxins such as aflatoxin. 02:03 This is associated with Aspergillus flavus, which is a fungal contamination of peanuts and corn, for example. 02:11 That will actually cause primary mutations within the liver and is not associated necessarily with cirrhosis. 02:18 Smoking, alcohol, chronic biliary disease, sclerosing cholangitis, for example, and autoimmune hepatitis, or other causes for having hepatocellular carcinoma. 02:30 Let's discuss pathophysiology. 02:32 You see here the normal hepatocyte architecture with cords of hepatocytes in a nice linear array sitting on a basement membrane, and they will be interfacing with a space, a virtual space between the hepatocyte cord and the sinusoids which are lined by endothelium. 02:51 In that space are quiescent stellate cells, these are precursor cells. 02:55 They regulate fibrosis within the liver, and a variety of other activities. 03:00 And then, cruising around in this space, the space of disse and also within the vasculature are the macrophages of the liver called Kupffer cells. 03:09 In the normal liver, everybody is happy. 03:11 The stellate cells are acquiescent, the Kupffer cells are not activated, and we are going about our business. 03:19 With liver injury, we cause damage to the hepatocytes and that will elicit an inflammatory response, so that we will activate the Kupffer cells which will make inflammatory cytokines. 03:30 A combination of hepatocyte injury and the activated Kupffer cells will then crank the stellate cells into action. 03:39 They will proliferate and their response to injury and inflammatory cytokines etc. 03:45 Is going to be making increased extracellular matrix, they will make a fibrosis and this is the process by which with recurrent bouts of injury to deliver, we can end up with cirrhosis. 03:58 I would refer you back also to the cirrhosis talk in the series of gastrointestinal pathology lectures in the Lecturio series. 04:07 The pathogenesis of hepatocellular carcinoma is that typically arises not always but typically arises in chronic liver disease when there is cirrhosis. 04:16 So about 80% of the cases of HCC are with a pre existing cirrhosis. 04:23 What happens in cirrhosis is that you have ongoing hepatocyte proliferation, regeneration, the hepatocytes are constantly turning over. 04:31 They're constantly proliferating in a sea of inflammatory mediators, including reactive oxygen species, and other mediators that can cause new mutations. 04:42 Proliferation in the setting of possible mutations is a recipe for malignancy disaster. 04:50 And that's what happens, we just have hepatocytes that are proliferating, they are being bathed in reactive oxygen species, they acquire mutations as they proliferate and then we cement those new mutations into the progeny of the proliferating hepatocytes. 05:07 In many cases, we can identify the driver mutations. 05:10 So mutations in the beta catenin gene occurs in about 40% of hepatocellular carcinomas. 05:17 Upregulation of telomerase activity, so mutating the TERT gene promoter will occur and over half of hepatocellular carcinomas. 05:27 And inactivation mutations of p53, which are important for protecting the genome and identifying mutations. 05:36 So these are very common, they're not the only mutations, they don't always have to occur, but these are relatively frequent. 05:44 In non cirrhotic livers, so about 20% of the cases of HCC, other damages occurring I've already mentioned aflatoxin, which will be converted by the liver by the hepatocytes to a very toxic epoxide, which will cause primary DNA damage, particularly involving p53 and it will inactivate p53. 06:05 Rarely, hepatocellular adenomas that are associated with beta-catenin activating mutations will acquire additional mutations and become malignant. 06:15 But when we talked about benign hepatic neoplasms, we talked about hepatocellular adenoma and it's a relatively rare occurrence that it mutates into hepatocellular carcinoma. 06:27 There is a fibrolamellar variant of hepatocellular carcinoma, typically associated with a fusion gene that will lead to increased constitutive activity of protein kinase A, and that in turn will drive cyclic-AMP to be involved in increased proliferation of the hepatocytes. 06:50 So how will your patients present with hepatocellular carcinoma. 06:54 For small tumors, they're going to be largely asymptomatic and the cancer will only be found incidentally on imaging for some of the reason. 07:02 And in most cases, 80% of the time, when the cancers will arise in a cirrhotic liver. 07:09 The signs and symptoms are all going to be about cirrhosis. 07:12 So I'd refer you to the talk elsewhere within Lecturio on cirrhosis. 07:18 With decompensated cirrhosis, there's variceal bleeding, there's uncontrolled ascites. 07:23 You may also have extension of the hepatocellular carcinoma into the hepatic or portal veins which will cause obstruction of blood flow from the lower extremities. 07:33 When hepatocellular carcinoma does become symptomatic, it's usually as a vague abdominal pain or right upper quadrant discomfort. 07:41 There may be associated malaise, fatigue and weight loss. 07:44 The liver will be enlarged, palpably enlarged below the right lower costal margin. 07:51 There will be splenomegaly usually because of associated cirrhosis, and a mass may be actually palpable. 08:00 Making the diagnosis formally. 08:03 There are biochemical markers, Alpha-fetoprotein is actually pretty good. 08:08 It is not entirely specific, so you wouldn't use it as a screening tool. 08:14 But once you have identified that a patient has hepatocellular carcinoma, you can follow alpha-fetoprotein levels as a marker of disease or tumor burden. 08:22 Ultrasound, CT or MRI, all of these will identify tumor lesions within the liver. 08:29 It's indicated on the panels on the right hand side and to confirm the diagnosis and make sure it's not something else that's potentially benign., you would do a biopsy. 08:40 On biopsy or on excision, there are kind of two general patterns. 08:46 On the left hand side here is a well differentiated, hepatocellular carcinoma. 08:50 It looks a lot like normal liver, except it doesn't have the normal portal triad architecture, doesn't have the normal sinusoids but it does have cords and sheets, a reasonably well differentiated in this case, hepatocytes. 09:05 On the right hand side is a different stain. 09:07 This is a trichrome stain, with trichrome stains fibers connective tissue blue. 09:13 In the fibrolamellar variant associated with the protein kinase A fusion proteins, you see these dense bands of fibrous connective tissue and you then see sheets of very poorly differentiated hepatocytes. 09:27 Overall, this particular variant has a much better prognosis than the primary hepatocellular carcinoma that you see on the left. 09:36 The gross appearance is one of a infiltrating tumor mass, there may or may not be invasion into the portal vein with extension into the inferior vena cava and even the right side of the heart, so tumor can extend all the way up and may actually present as right sided heart failure, which is fairly impressive. 09:56 Cancers of the kidney will also do this incidentally. 10:01 So, how are we going to manage this? Well, overall the prognosis is kind of poor for primary hepatocellular carcinoma. 10:10 There are non surgical options, if the tumor is small, you can do radiofrequency ablation or microwave ablation, you can freeze it, you can do embolization. 10:20 Less than 10% of the tumors are going to be resectable. 10:23 It's not because they are way big, although that can be a reason. 10:28 But it's limited by the poor quality of the rest of the liver. 10:32 If there's pre existing cirrhosis, you don't really have a lot of latitude to carve out the tumor, that liver will not regenerate in the same way that a normal healthy liver will. 10:44 And in some cases, by the time we detected, it's rather large and so non resectable. 10:50 The prognosis depends on the severity of the underlying liver disease on the size of the tumor on how well or how far it is extended into adjacent structures, whether there is metastatic disease. 11:03 The overall five year survival, all comers is about 10%. 11:08 If we are able to get the patient to liver transplantation, so the underlying etiology for a cirrhosis, for example, is something that I will not recur, then you can do quite well with those patients and about three quarters of them will have a decent five year survival. 11:26 With tumor limited just to the liver, survival for five years about 30%. 11:31 If there's regional extension into adjacent structures or into the draining veins, the five year survival goes down to about 10%. 11:40 And if there's distant metastases, it's a very bad prognosis and 2% to 3% five year survival. 11:49 Okay, so that's all about hepatocellular carcinoma. 11:52 Very briefly, in the last couple slides, we're going to talk about liver metastases. 11:56 These tumors, liver metastases, 30 times more common than primary liver cancers. 12:03 Importantly, half of patients who are going to die from malignancy will have liver metastases, and a significant portion of them will be dying because of liver metastases. 12:12 You can see the long list of tumors that like to go to the liver. 12:17 Colorectal cancer is probably number one on the list, mainly because when tumor gets into the veins, in the primary site in the colon or rectum, it goes via the portal circulation and the next capillary bed it will encounter is the liver. 12:34 So GI malignancy going to the liver is actually quite common, but pretty much any tumor anywhere and it's travels around the bloodstream, we'll find its way to delivering can metastasize. 12:48 The diagnosis is one of imaging for the most part, in the setting of a known primary someplace else, you can do a CAT scan, a positron emission tomography or a PET scan will also allow you to assess the degree of tumor. 13:04 Importantly, our imaging, even our very best imaging can only detect down to about 0.2 - 0.3 centimeter size. 13:11 So you can have multiple, very small tumors that have substantial number of tumor cells up to 10 million, and you can't detect that on best imaging. 13:21 Imaging will typically show what is shown here on the picture, multiple rounded, smooth border tumors, often there will be a central umbilication, so called umbilication, indicating that there is central tumor necrosis. 13:37 The management depends on the primary cancer site and if the primary cancer is going to be chemo responsive, then you might be in good shape, or if it's going to be responsive to immunotherapy. 13:47 In general, it's going to be very difficult, especially with multiple metastatic tumors to surgically resect these but if there's a limited number, surgeons will attempt to treat to achieve cure by resecting those known metastases. 14:06 With that we've covered hepatocellular carcinoma and metastatic carcinoma within the liver.
About the Lecture
The lecture Hepatocellular Carcinoma (HCC) and Liver Metastases by Richard Mitchell, MD, PhD is from the course Disorders of the Hepatobiliary System.
Included Quiz Questions
What are the risk factors for hepatocellular carcinoma? Select all that apply.
- Cirrhosis
- Smoking
- Aflatoxin
- Paget disease
- Reye syndrome
What percentage of hepatocellular carcinoma arises in the context of chronic liver disease?
- 80%
- 50%
- 30%
- 5%
- 95%
What are the possible initial symptoms of hepatocellular carcinoma? Select all that apply.
- Abdominal pain
- Malaise
- Hepatomegaly
- Hematochezia
- Change in bowel habits
What percentage of hepatocellular tumors are resectable?
- < 10%
- > 90%
- 60%
- 50%
- 30%
Which of the following statements about liver metastases is true?
- Liver metastases are 30 times more common than primary liver cancer.
- Liver metastases are 15 times less common than primary liver cancer.
- Liver metastases are as common as primary liver cancer.
- Half of all patients dying from malignancy have primary liver cancer.
- Ninety percent of patients dying from malignancy have liver cancer.
What is the most common primary tumor that metastasizes to the liver?
- Colorectal
- Melanoma
- Gastric
- Anal
- Prostate
What is an imaging finding of a tumor that points toward a metastatic liver tumor?
- Central umbilication due to central necrosis
- Solitary tumor
- Infiltrative borders
- Poorly defined peripheral borders
- Portosystemic shunting
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |