Playlist
Show Playlist
Hide Playlist
Budd-Chiari Syndrome and Veno-occlusive Disease (VOD)
-
Slides GIP Budd-Chiari Syndrome and Veno-occlusive Disease.pdf
-
Download Lecture Overview
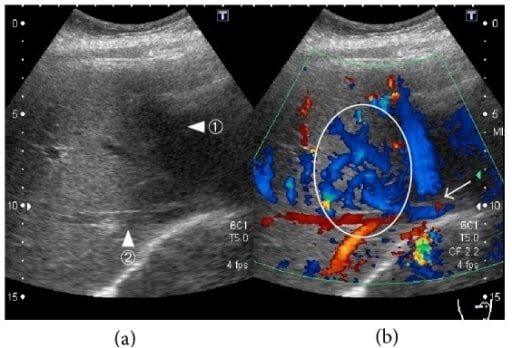
00:01 Welcome. 00:02 In this talk we're going to be covering disorders in the liver that occur due to venous outflow obstruction. 00:09 In Budd-Chiari syndrome, that's going to be larger venous occlusions. 00:13 In veno-occlusive disease, we're going to be talking about occlusion at the level of the central vein within the hepatic lobules. 00:20 So Budd-Chiari syndrome and veno-occlusive disease are simply these disorders associated with hepatic venous outflow obstruction. 00:29 In primary Budd-Chiari, the obstruction is due to thrombosis or inflammation, mostly of the hepatic vein into the inferior vena cava. 00:39 And secondary Budd-Chiari, it's an extrinsic compression or invasion of the hepatic veins and or the IVC due to tumor or other causes. 00:49 In veno-occlusive disease, this is much more within the liver parenchyma at the level of the central veins in the hepatic lobules. 00:57 So it's sinusoidal obstruction due to endothelial damage at that level. 01:02 Here's the epidemiology. 01:04 So overall, not a public health menace, Budd-Chiari is usually kind of in the range of one in a million annual incidents. 01:14 Overall, in the population at large because it is somewhat of a chronic disease, we will have 11 in a million patients affected at any particular time. 01:24 In Asian countries versus non-Asian countries, there's a slight difference in epidemiology. 01:29 And for reasons I don't entirely understand. 01:32 In Asian countries, men are more commonly affected than women. 01:35 And it's going to tend to be larger vessel obstruction inferior vena cava, or combined IVC and hepatic vein. 01:43 In non-Asian countries, women are affected more commonly than men, and it tends to be more near the liver parenchyma, so it's more hepatic vein occlusion, and than it is IVC. 01:55 In veno-occlusive disease, the epidemiology is really related to transplantation and the chemotherapy regimen that is instituted prior to hematopoietic stem cell transplantation. 02:11 The pathophysiology overall. 02:13 So in Budd-Chiari syndrome, the most kind of general global cause is hypercoagulability. 02:19 About 4/5ths of patients will have some underlying procoagulant diathesis. 02:26 So polycythemia Vera and other myeloproliferative disorders, malignancy, paroxysmal, nocturnal hemoglobinuria, and I would refer you to the talk in general cellular pathology, if you're interested in PNH. 02:40 Antiphospholipid antibody syndrome, typically associated with lupus, or mutations in say factor V Leiden or anti thrombin three, protein C, protein S, that lead to thrombophilia, a procoagulant diathesis. 02:55 Pregnancy also makes you hypercoagulable and may make you more prone to the Budd-Chiari syndrome where you're going to get thrombosis of the inferior vena cava or the hepatic vein and that will occlude vascular outflow from the liver. 03:11 The secondary Budd-Chiari syndrome caused by malignancy, the direct invasion or compression of the hepatic vein or the inferior vena cava. 03:20 Most common cause is going to be hepatocellular carcinoma, but renal or adrenal cancers can do this as well. 03:25 You can also have infections or benign liver lesions such as an abscess that's responsible. 03:31 And there are a variety of miscellaneous things, autoimmune disorders, leading to inflammation within that vascular bed or toxic exposures and in particular plant, alkaloids. 03:43 And there is a disease an entity called bush tea disease, which will give you a Budd-Chiari -like- Syndrome by damaging the endothelium and causing a thrombosis in the IVC or the hepatic vein. 03:57 Veno-occlusive disease is very closely associated with plant alkaloids and as they said, chemotherapy for bone marrow transplant or malignancy. 04:04 So the conditioning, chemotherapy that will do that. 04:08 In all of these cases, you're damaging the endothelium. 04:11 And why is it happening in that location, the hepatic veins, central veins, or in the IVC and that's because whatever compound is going to be entering the endothelium in those locations, has been metabolized by the liver. 04:27 So it's not going to be something that's going to cause systemic thrombosis, but it will be something that's going to be caused by thrombosis in the draining vessels coming out of the liver because of the metabolism. 04:39 So you can have on this schematic here, you can have hepatic vein thrombosis or obstruction for a variety of reasons that we just talked about. 04:48 So that's the intrahepatic vein. 04:50 So you can have extra hepatic venous congestion or obstruction. 04:54 Clearly because we're not now not able to flow out of the liver, we're gonna get sinusoidal congestion with backup of blood into the liver. 05:03 And that increased sinusoidal pressure will lead to relative cellular hypoxia, you are not moving through good oxygenated blood anymore, which will lead in turn to liver cell damage. 05:14 And by backing up the pressures from the hepatic vein to the central vein into the portal system, you'll end up with portal hypertension. 05:23 So the manifestations kind of come out of this pathway, in terms of what's happening overall. 05:30 The clinical presentation, the classic symptom triad is abdominal pain. 05:34 And this is mostly due to the portal hypertension but also the dilated liver that is filled up with blood quite congested stretching of Glisson’s capsule around the liver that's invested with a variety of sensory nerves and it's perceived as pain or discomfort. 05:49 There will be hepatomegaly, the liver will be large and you can palpate it below the right lower costal margin. 05:56 There will be ascites and this is because of the portal hypertension and the increased vascular pressure. 06:01 We also expect to see jaundice as we alter the normal metabolism of bilirubin. 06:07 As we have less production of albumin and as we have increased, now poor flow through the inferior vena cava, you will have lower extremity edema. 06:18 If the liver is not functioning appropriately, you'll have encephalopathy. 06:21 And then of course, with portal hypertension, you can develop portal systemic shunts and you can have various bleeding. 06:30 So the symptoms and findings are going to vary by onset and you can have very abrupt onset or more chronic course. 06:38 Not commonly you can have fulminant liver failure. 06:41 Still these common presentation, patient develops out of the blue hepatic encephalopathy. 06:46 Within about eight weeks of jaundice onset, there are markedly elevated transaminases, there is a profound coagulopathy but because all this damage is happening so quickly, they're basically very few of any Porto-systemic shunts. 07:02 Acute syndrome is somewhere in between, it's going to be a little bit longer than 8 weeks. 07:07 But the symptoms and signs will depend on the degree of liver failure and jaundice, abdominal pain, ascites will all occur. 07:16 And these also tend not to develop Porto-systemic shunts due to the acuity of the illness. 07:22 A subacute syndrome is the most common presentation. 07:24 So a rather slow and progressive occlusion of hepatic outflow. 07:31 It may be completely asymptomatic as you develop collateralization. 07:36 And the most common finding is that you develop symptoms over the course of months to even years. 07:43 And because it's slower in terms of the accumulation of the occlusion, you develop Porto-systemic shunts and so you can have bleeding. 07:52 Again, in the chronic syndrome, it's going to be much more typical of a chronic poorly functioning liver rather than the acute which is going to be primarily CNS in terms of the manifestations. 08:06 In the chronic syndrome you will have cirrhosis, and you will develop all the stigmata associated with cirrhosis including spider angiomata, palmar erythema, signs of portal hypertension and hepatic encephalopathy not being very common because everything that you're absorbing through the GI tract that would normally be passed through the liver that's not working in into the systemic venous circulation, it can't get into the systemic circulation. 08:33 So the brain is relatively protected in a chronic onset of Budd-Chiari or venous occlusive disease. 08:42 Making the diagnosis. 08:44 Ultrasound is probably your best bet. 08:46 You can look for flow through the venous circulation, you can actually measure blood flow in the inferior vena cava and the hepatic vein. 08:55 It's your first line diagnostic test. 08:58 You may also see dilated walls with hepatic veins. 09:01 And you may even be able to visualize the thrombus or other obstructions, so this is the way to make the diagnosis. 09:07 CT and MRI may be helpful in indicating areas where you have either loss of perfusion to the liver due to a partial obstruction in a subset of the area within the liver parenchyma. 09:20 Venography is a gold standard, although increasingly ultrasound is the way that most clinicians will make the diagnosis. 09:27 If the non invasive testing is inconclusive, you will do this and demonstrate that you do not get egress of your radiopaque dye out of the liver. 09:39 Laboratory tests include looking at elevated transaminases and coagulation parameters. 09:46 But those are nonspecific, they just give you a rough sense of the degree of liver injury and liver biopsy can be performed although that's going to be somewhat nonspecific, for anything other than veno-occlusive disease, which will show small central venous obstructions. 10:04 How do we manage this disease? Well, depends on the cause. 10:08 So you want to treat the underlying pathology and if it is a hypercoagulable state, you want to treat that, if it's due to malignancy, you treat that. 10:16 If it's due to a therapeutic intervention, you try to stop that. 10:21 So chemotherapy etc. 10:23 We want to prevent propagation of the clot. 10:25 So we'll give anticoagulation, typically heparin or other anticoagulants. 10:31 If there is a definable physical obstruction, we will remove that, hopefully restoring blood flow. 10:38 In extreme cases, we made progress to a Trans-Jugular Intrahepatic Porto-systemic Shunt. 10:44 So this is a way by which you can go from the portal vein directly bypass the liver and dump into the inferior vena cava. 10:53 So if there's an area of obstruction, you can bypass that and restore normal flow. 10:59 Now this will return the possibility of having hepatic encephalopathy because the GI tract is dumping it's contents directly into the inferior vena cava. 11:08 And for causes that are due to intrinsic liver disease, you can progress to liver transplantation. 11:17 The prognosis of without treatment, quite bad. 11:21 This is a lethal disease, three year survival of only 10%. 11:26 However, with appropriate therapy and identify the causal agent or the underlying pathology, you can do quite well with 75%, 5-year survivals. 11:38 The causes of death will include ascites that is just intractable with associated renal dysfunction hyponatremia, etc. 11:46 Gastrointestinal bleeding due to the varices or profound liver failure. 11:52 With that, we've concluded talking about poor outflow of the liver, Budd-Chiari syndrome and veno-occlusive disease.
About the Lecture
The lecture Budd-Chiari Syndrome and Veno-occlusive Disease (VOD) by Richard Mitchell, MD, PhD is from the course Disorders of the Hepatobiliary System.
Included Quiz Questions
What causes primary Budd-Chiari syndrome?
- Thrombosis or phlebitis
- Extrinsic compression by tumor
- Extrinsic compression by abscess
- Extrinsic compression by hemangioma
- Fistula
What is the most common etiology of Budd-Chiari syndrome?
- Hypercoagulability
- Polycythemia vera
- Malignancy
- Paroxysmal nocturnal hemoglobinuria
- Antiphospholipid syndrome
What is the classic triad of symptoms in Budd-Chiari syndrome? Select all that apply.
- Abdominal pain
- Hepatomegaly
- Ascites
- Nausea
- Jaundice
What are the symptoms of Budd-Chiari syndrome? Select all that apply.
- Abdominal pain
- Jaundice
- Encephalopathy
- Lower extremity edema
- Tinnitus
What is the preferred first-line diagnostic test for Budd-Chiari syndrome?
- US
- CT
- MRI
- CBC
- PET/CT
What is the gold standard test for Budd-Chiari syndrome?
- Venography
- CT
- MRI
- CBC
- CMP
What is the site of obstruction in veno-occlusive disease?
- Sinusoidal obstruction due to endothelial damage
- Portal vein thrombosis due to coagulation factors
- Obstruction at the level of hepatic artery due to atherosclerosis
- Central venous blockage due to fibrin clots
- Biliary duct obstruction due to bile salt deposition
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |