Playlist
Show Playlist
Hide Playlist
Intracranial Pressure (ICP) and Blood Pressure: Interventions
-
Emergency Medicine Head Injury.pdf
-
Download Lecture Overview
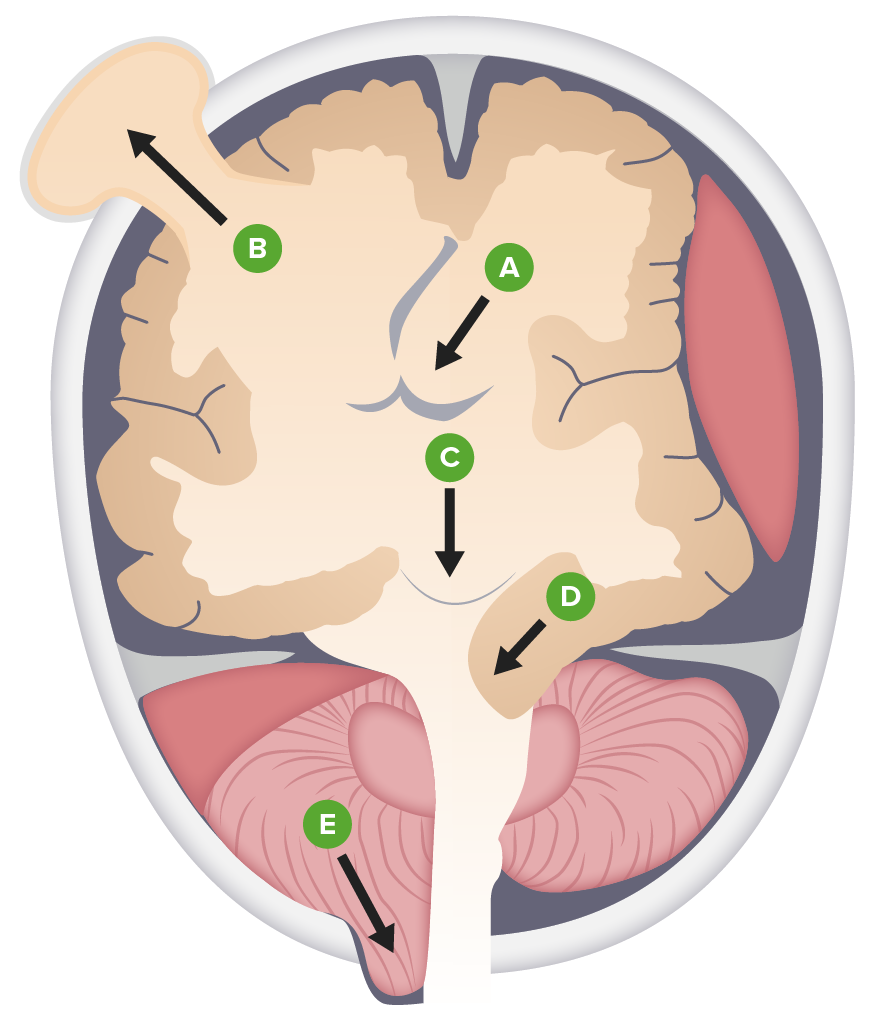
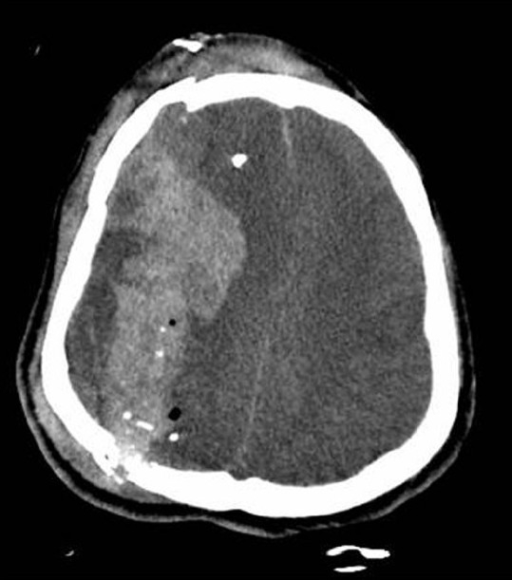
00:01 So what can we do to lower the intracranial pressure? Well, there’s several interventions that we commonly perform. 00:07 The easiest and quickest one is just elevating the head of the bed and that works by enhancing venous drainage out of the cranium. 00:13 Basically, you know, gravity helps us. 00:15 So we put the head of the bed up more blood flows out of the head and decreases the amount of intracranial blood volume. 00:21 It can be safely used for anyone and if you’re not able to sit your patient up because their spine isn’t cleared you can just use the reverse Trendelenburg position to put the head up a little bit above the heart. 00:34 Another common intervention that we use is mannitol. 00:36 So mannitol is an osmotic diuretic and basically what it does is it pulls water osmotically out of the neurons and into the intravascular space. 00:47 So it’s actually physically shrinking the brain. 00:50 It’s dehydrating the neurons and making the brain volume smaller. 00:54 This is a great treatment option for patients who are normotensive or hypertensive. 01:00 However, remember, it is a diuretic, so it’s gonna cause increased urine output and volume depletion. 01:06 So if your patient is hypotensive to begin with, you wouldn’t wanna give them this, ‘cause it’s gonna decrease their circulating volume. 01:14 So really only appropriate for normo or hypertensive patients. 01:18 And you wanna make sure you watch the blood pressure after you give it because the diuretic effect can cause hypotension as well. 01:24 Hypertonic saline works basically the same way. 01:27 So if you give saline that is hyperosmolar relative to the intracellular space, it’s gonna also pull water out of the neurons and into the serum thereby decreasing the volume of brain tissue. 01:42 The nice thing about hypertonic saline is it can be used pretty much for any patient unless they’re grossly hypernatremic because it’s gonna increase you circulating volume and increase you blood pressure. 01:53 So it’s safe for you hypertensive multi trauma patients and it probably will be the treatment of choice for our patient who presented in hemorrhagic shock. 02:01 Another option we can use is hyper-ventilation. 02:04 And hyper-ventilation works by constricting the cerebral vasculature. 02:09 So basically, in response to respiratory alkalosis the cerebral vasculature clamps down thereby decreasing the circulating blood volume in the brain. 02:19 Now, this is a great treatment option for patients who have impending herniation. 02:23 If you really think, "Wow. 02:24 This patient’s got a blown pupil, he’s got a massive bleed in his head and I’ve got to keep him from herniating until he gets up to the operating room." Hyper-ventilation is a really good option. 02:36 But a couple of important things to remember about hyper-ventilation is one, it’s got a transient effect. 02:41 So there’s no point in doing it unless you are bridging the patient to a more definitive intervention. 02:49 Basically, it’s only gonna work for an hour or two at which point the whole system resets itself and you’re not gonna get any benefit from it. 02:57 So it’s not something that you would use as a long term treatment alternative for somebody who is not going to the operating room. 03:04 It would really just be used as a bridge for somebody like our patient who is gonna get definitive management. 03:10 The other thing to remember is that you know, cerebral vasoconstriction is a little bit of a double-edged sword. 03:16 So a little bit of vasoconstriction is nice cause it’ll decrease the circulating blood volume in the brain and decrease your pressure. 03:24 As you can imagine though, a lot of cerebral vasoconstriction is problematic because then that’s gonna impaire cerebral blood flow and cause ischemia. 03:33 So you wanna be very, very careful with hyper-ventilation that you don’t overdo it. 03:38 You wanna have your patient on continuous end-tidal CO2 monitoring and you wanna aim for a pCO2 of 30-35. 03:45 Do not go below 30 because if you do, you’re gonna cause cerebral vasospasm and ischemia. 03:52 So really important to remember, you can only use this briefly and you have to monitor closely and not overdo it. 03:59 All right. 04:00 The last option is not really something we do in the Emergency Department but it’s placement of a ventriculostomy catheter. 04:06 Which basically allows one direct monitoring of intracranial pressure, and two manipulation of intracranial pressure because you can pull off CSF if you need to in order to lower the pressure. 04:19 This is used for patients with severe ICP elevation who really aren’t surgical candidates, who have non-surgical disease process and it’s not done in the Emergency Department. 04:30 It’s done by a neurosurgeon, but it is something for you to be aware of as a potential treatment for patients who has severe ICP elevations. 04:40 All right. 04:41 Moving on to control of bleeding. 04:43 One thing you wanna make sure you do is to check coagulation studies and platelet levels in every single patient with intracranial hemorrhage. 04:51 In the event that your patient is coagulopathic or they’re on an anti-coagulating agent, you wanna reverse that immediately. 04:58 This is one of the few situations where you wanna just completely normalize the coagulation status regardless of their reason for anti-coagulation. 05:09 If they are coagulopathic, you can consider treating them with fresh frozen plasma in order replace clotting factors and help improve the clotting of the blood. 05:18 And if they’re thrombocytopenic, you can give platelet transfusion. 05:22 There have been studies looking at patient who are anti-platelet agents like aspirin, ticagrelor or clopidogrel. 05:29 And there’s no evidence that giving those patients platelets actually produces clinical benefits. 05:35 So it’s probably not necessary to do that, although you will probably see it done in some cases regardless. 05:43 All right. 05:44 Last thing to talk about is blood pressure. 05:46 So both hypertension and hypotension are problematic for patients with intracranial injuries. 05:52 Hypotension is strongly associated with poor outcomes and that’s because of impaired cerebral perfusion. 05:58 So if your patient is hypotensive, you need to be aggressive. 06:00 you need to treat them with fluids. 06:02 If you’re not getting good response with fluids, you need to treat them with pressors. 06:06 And you need to identify the underlying cause. 06:08 So head injury in it of itself would never cause hypotension. 06:12 You need to look for some other explanation either hemorrhagic shock or some medical cause of their shock and address that underlying problem. 06:23 So head injury does not cause hypotension. 06:27 By contrast, elevated blood pressure can potentially be problematic. 06:32 Now, a little bit of hypertension is a good thing because if your intracranial pressure is elevated having a high blood pressure actually will improve your cerebral perfusion. 06:42 But if the blood pressure is too high that raises the hydrostatic pressure in the vasculature and can actually make bleeding worst. 06:50 So your goal is to be judicious in your treatment of hypertension. 06:55 You generally want a goal systolic pressure of about 160. 06:59 So if your patient is much above that you probably wanna bring them down a little bit. 07:03 But you don’t need to bring them down to normal. 07:05 In fact, normalizing their pressure rapidly can be very harmful. 07:09 So you do wanna make sure that you use agents that you can readily titrate. 07:13 So use a continuous infusion of the medication like Nicardipine for example, so you can turn it up and down as needed to attain your goal blood pressure rather than giving them something oral that is gonna have an unpredictable long term effect. 07:30 All right, so back to our patient. 07:32 We already talked about his large subdural hematoma. 07:35 And he actually had an anisocoria with a blown pupil on his physical exam. 07:40 So we’re very concerned that he has signs of impending herniation. 07:44 So if he wasn’t already intubated which I’m thinking he should have been, we definitely would wanna intubate him at this juncture and make sure we have adequate IV access. 07:53 We’re gonna get our neurosurgical team on board, because he needs surgical evacuation of this hematoma. 07:59 We’re gonna reduce his ICP by elevating the head of the bed. 08:03 We’re gonna use hypertonic saline for him. 08:05 And he is somebody that we probably would hyper-ventilate, because we would be bridging him to a definitive treatment that being surgical evacuation of his hematoma. 08:15 His blood pressure right now is adequate so we’re gonna keep an eye on it. 08:18 But definitely, if he gets hypotensive again we’re gonna wanna be very aggressive about treating that. 08:24 And then, he doesn’t have any anti coagulant user coagulopathy but we are gonna check his coags and platelets just to make sure that all of his levels are normal. 08:32 So just to wrap it up, take home points from this lecture are one that GCS is a very reliable way to quantify mental status and it is useful for predicting outcomes at least up to a point. 08:45 Your essential neurologic primary survey is gonna include an assessment of the GCS, a pupillary exam, and four extremity motor exam. 08:54 You need to obtain a non-contrast head CT in any patient with a GCS of less than 13, and you might consider CT in patients with higher GCS if they have complicating factors. 09:05 The injury pattern that you observed on CT is what’s gonna determine your management. 09:10 And your management in the ED is gonna focus on stabilization of the ABCs, regulating the ICP, managing the blood pressure, and stopping bleeding. 09:21 Thank you very much.
About the Lecture
The lecture Intracranial Pressure (ICP) and Blood Pressure: Interventions by Julianna Jung, MD, FACEP is from the course Trauma (Emergency Medicine). It contains the following chapters:
- Interventions to Lower ICP and Bleeding Control
- Blood Pressure
Included Quiz Questions
Which intervention to lower the intracranial pressure is the easiest and quickest to apply to all patients without a spine injury?
- Head elevation
- Mannitol administration
- Hypertonic saline
- Blood pressure control
- Hyperventilation
What is the mechanism of hyperventilation in decreasing intracranial pressure?
- Cerebral vasoconstriction
- Enhance venous drainage
- Osmotic diuresis
- Decrease in blood pressure
- Increase in oxygen supply
What blood product is the best option to be given to patients with coagulopathies?
- Fresh frozen plasma
- Packed RBC
- Cryoprecipitate
- Buffy coat
- Whole blood
Which of the following statements regarding blood pressure control in intracranial pressure management is INCORRECT?
- Hypertension must be managed aggressively to decrease blood pressure within the normal range.
- Hypotension is associated with poor outcomes.
- Hypotension is treated aggressively with fluids and/or vasopressors.
- Titratable agents are used in the management of hypertension.
- Excessive hypertension may worsen bleeding.
Which of the following interventions for raised intracranial pressure is NOT done in the emergency department?
- Placement of a ventriculostomy
- Assessment of A-B-C-D
- Intracranial pressure regulation
- Blood pressure control
- Cessation of bleeding
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
That was a really good high-yield class, props to her.