Playlist
Show Playlist
Hide Playlist
Gastroschisis
-
Slides GIP Gastroschisis.pdf
-
Download Lecture Overview
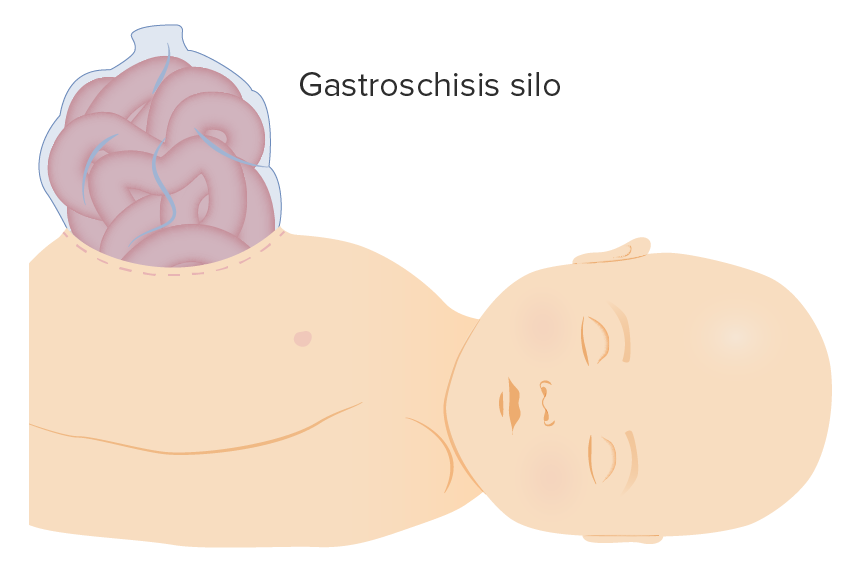
00:01 Welcome. 00:03 In this talk, we're going to be discussing gastroschisis, which is part of gastrointestinal pathology. 00:09 You will see we have a lot to talk about when we talk about GI pathology. 00:14 It's more or less from the top to the very bottom with a lot of other organs attached on the side. 00:21 In some of these initial talks on GI pathology, we're going to talk about anomalies, maldevelopment, and gastroschisis will top the list. 00:29 So gastroschisis is a full thickness defect of the anterior abdominal wall. 00:34 And the intestines or some of the viscera such as liver will protrude outside but there will be no membrane or sac covering this. 00:42 This is to be distinguished from omphalocele that we're going to talk about next. 00:47 So the defect is often also just to the right of the umbilical insertion site. 00:52 And we'll talk in a moment about developmental biology, so that will explain why there's this typical location for gastroschisis. 01:00 This roadmap, we will see over and over again, throughout all of the talks on gastrointestinal pathology. 01:07 And we'll use this again here where we'll talk about epidemiology. 01:11 Then we'll go through pathophysiology, we'll do clinical presentation, diagnosis and monitoring, and management and prognosis. 01:19 So first, for epidemiology. 01:21 It's a relatively rare prevalence for this disease. 01:24 So a gastroschisis occurs in roughly 3-4 babies born out of 10,000 births. 01:31 And there's a similar incidence whether the baby happens to be male or female. 01:36 In 10% of the cases, however, gastroschisis is also associated with anomalies outside of the GI tract. 01:41 And this raises the specter as we'll see in a moment of basic genetic defects. 01:47 There's also a very higher risk of preterm delivery and pregnancies when there's gastroschisis. 01:52 So about a quarter of babies with gastroschisis will have earlier preterm delivery that's compared to those who do not which is about 5% of the total. 02:02 So there are a number of maternal risk factors that put babies at risk of developing gastroschisis. 02:08 A very young mom, for example, will be a good reason. 02:12 Women who are pregnant in her less than 20 years of age have an increased risk for delivering a baby with gastroschisis. 02:18 Also very low body mass index. 02:21 So someone who just doesn't have a lot of meat on her bones. 02:25 We will also have increased risk associated with certain ingestion such as exposure to cigarette smoke, or the intake of aspirin and ibuprofen, nonsteroidal anti-inflammatory drugs. 02:38 In addition, the intake of decongestants can be associated with gastroschisis for unclear reasons. 02:45 Let's get into the pathophysiology. 02:48 So we're looking here at a very early, about four weeks embryo. 02:54 It doesn't look like much. 02:55 This is a transverse slice, at the top is going to be anterior at the bottom is going to be posterior. 03:04 The yellow is yolk sac. 03:06 The green is amniotic fluid, and you see a lining of ectoderm around that and mesoderm as well. 03:12 It will now go through a variety of folds that allow us to finally get the developed embryo with now an abdominal peritoneal cavity that has in the case of gastroschisis, a lateral wall defect. 03:32 Here we're seeing a lateral view from the side, showing the similar kinds of folding, and it can be very complex. 03:38 So we're gonna show them side by side with a transverse and a lateral view, seeing the various folds that occur. 03:46 And you'll see looking at the transverse image, we're going to have a defect that is going to be our gastroschisis, and on the right you will also see where the bowel is herniating through the abdominal wall. 03:59 So with regard to the pathophysiology, and why this defect typically occurs on the right-hand side. 04:06 Let's get into some of the vascular development that happens during differentiation. 04:11 The umbilical veins in the developing placenta and fetus are originally bilateral. 04:16 They drain into the sinus venosus which will eventually become the right atrium. 04:21 In the second month of gestation, there is complete regression of the right umbilical vein. 04:26 However, the left umbilical vein persists, connecting to the ductus venosus within the developing liver. 04:33 The ductus allows the shunting of oxygenated blood past the liver, and into the nascent inferior vena cava. 04:41 While it is patent however, the right umbilical vein is really important for supplying the nutritional building blocks that allow the normal right sided abdominal wall development. 04:52 If however, the right umbilical vein decides it's going to close prematurely, the abdominal wall will be incompletely formed. 04:59 That will obviously then lead to the gastroschisis that is seen at birth. 05:04 And now you understand why there's a right sided predominance of these lesions. 05:10 Let's come to the clinical presentation. 05:13 So it's not subtle in most cases, there is a paraumbilical abdominal wall defect, usually to the right side of the umbilical cord insertion site, and there's no membrane covering that. 05:25 The abdominal wall defect is usually something less than 4 cm. 05:30 There are complications associated with this, as you might expect. 05:33 So with this part of the bowel being outside of the abdominal wall, during development, there's reduced bowel motility. 05:41 And there's also reduced bowel absorption due to the unprotected intestine being exposed to irritating amniotic fluid and we tend to lose fluid into that developing GI tract because of irritation. 05:56 There's also related vascular compromise caused by the bowel's herniated, so we will may not get normal bowel development. 06:05 And as a result of that intestinal atresia, so loss of part of the GI tract is seen in about 5% to 25% of newborns with gastroschisis. 06:15 So the complications overall involve intestinal stenosis, that means that we have obliterated the lumen of the intestine, you may have short bowel because it's just not developing normally, you may lose portions of the bowel, intestinal atresia, you may have perforation, or you may have necrosis or volvulus volvulus, literally meaning tying the bow into a knot. 06:38 As a result of this exposed bow, you also have an increased risk for gastrointestinal infections. 06:43 And there's a very high risk for in-hospital mortality and complications, which means we really need to mobilize the clinical teams when we identify this at birth. 06:53 Diagnosis and monitoring. 06:56 So ultrasonography is going to be our best friend in diagnosing this. 06:59 And most of the time, we make a prenatal diagnosis often as early as 14 weeks, but usually around 20 weeks or mid gestation. 07:08 The findings include oligohydramnios, which means a reduced amount of amniotic fluid. 07:14 And then we will also occasionally see other organs that have herniated such as the liver. 07:19 If there are more organs that are herniated that obviously increases the overall risk. 07:24 This is just an ultrasound, and you can see the head to the left, and we have a green arrow pointing to a very obvious defect in the abdominal wall with loops of bowel sticking out. 07:35 When this is identified, we will also in most cases do fetal genetic studies because there is an underlying genetic basis for a number of these cases of gastroschisis. 07:47 And especially if we want to identify potentially other complications that will affect long-term management. 07:56 In terms of that management and the overall prognosis, so the message is this is going to be okay in most cases. 08:03 It does require that we get together with the maternal fetal medicine specialists, neonatologist and the pediatric surgeon and we would normally having identified this in advance recommend delivery in a center that has terrific neonatal care resources. 08:19 For uncomplicated gastroschisis, that means nothing else is herniated besides a few loops of bowel that is not a contraindication to vaginal delivery. 08:28 But if we have liver herniation as well. 08:31 Babies should be delivered by cesarean. 08:34 They need to go into neonatal intensive care. 08:37 And we want to reduce intestinal injury and reduce fluid loss because of the loops of bowel that are exposed. 08:44 We protect that exposed bowel by wrapping it with sterile saline dressings covered with a plastic wrap to limit the loss of fluid. 08:51 And in some centers, you may even lower the entire lower half of the neonate into a plastic bag that will protect all of the lower bowel perfusion. 09:02 In our neonatal care centers we will reduce that intestinal injury. 09:06 We will do fluid and electrolyte resuscitation and we will give prophylactic broad-spectrum antibiotics to limit the possibility of infection. 09:15 And finally, to treat this, initially we will decompress the bowel. 09:20 So we don't want anything going through those loops about until we can surgically correct it. 09:26 We'll maintain airway, we will give respiratory support as necessary. 09:30 And then ideally surgery is performed within hours of birth. 09:35 And that's to minimize intestinal injury and during that surgery, we will usually extend the defect a little bit so that we are not poking the bowel through a little tiny hole. 09:47 We'll make the hole a little bit bigger. 09:49 In general, surgical closure, once we have reduced the bowel, pushed it back inside will be successful in greater than three quarters of cases.
About the Lecture
The lecture Gastroschisis by Richard Mitchell, MD, PhD is from the course Congenital Gastrointestinal Tract Disorders.
Included Quiz Questions
What is one difference between gastroschisis and omphalocele?
- No membrane or sac covers the intestine in gastroschisis.
- No skin covers the intestine in gastroschisis.
- A layer of pericardium covers the intestine in gastroschisis.
- A layer of peritoneal fluid covers the intestine in gastroschisis.
- Ascites covers the intestine in gastroschisis.
What is the usual location of gastroschisis?
- Directly to the right of the umbilical insertion site
- Directly superior to the umbilical insertion site
- Directly inferior to the umbilical insertion site
- Directly to the left of the umbilical insertion site
- Directly at the umbilical insertion site
What step of embryological development fails in patients with gastroschisis?
- Failure of lateral wall closure
- Failure to form the amniotic cavity
- Failure to form the yolk sac
- Failure to form the abdominal wall
- Failure to form the peritoneum
What is a risk factor for gastroschisis?
- Intake of decongestants
- Older maternal age
- High body mass index
- Deli meat consumption
- Nulliparity
What is a complication of gastroschisis?
- Volvulus
- Increased bowel length
- Tracheoesophageal fistula
- Marfan syndrome
- Irritable bowel syndrome
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |