Playlist
Show Playlist
Hide Playlist
Tuberculosis (TB) in Children: Pathology & Diagnosis
-
Slides TB Alverson.pdf
-
Download Lecture Overview
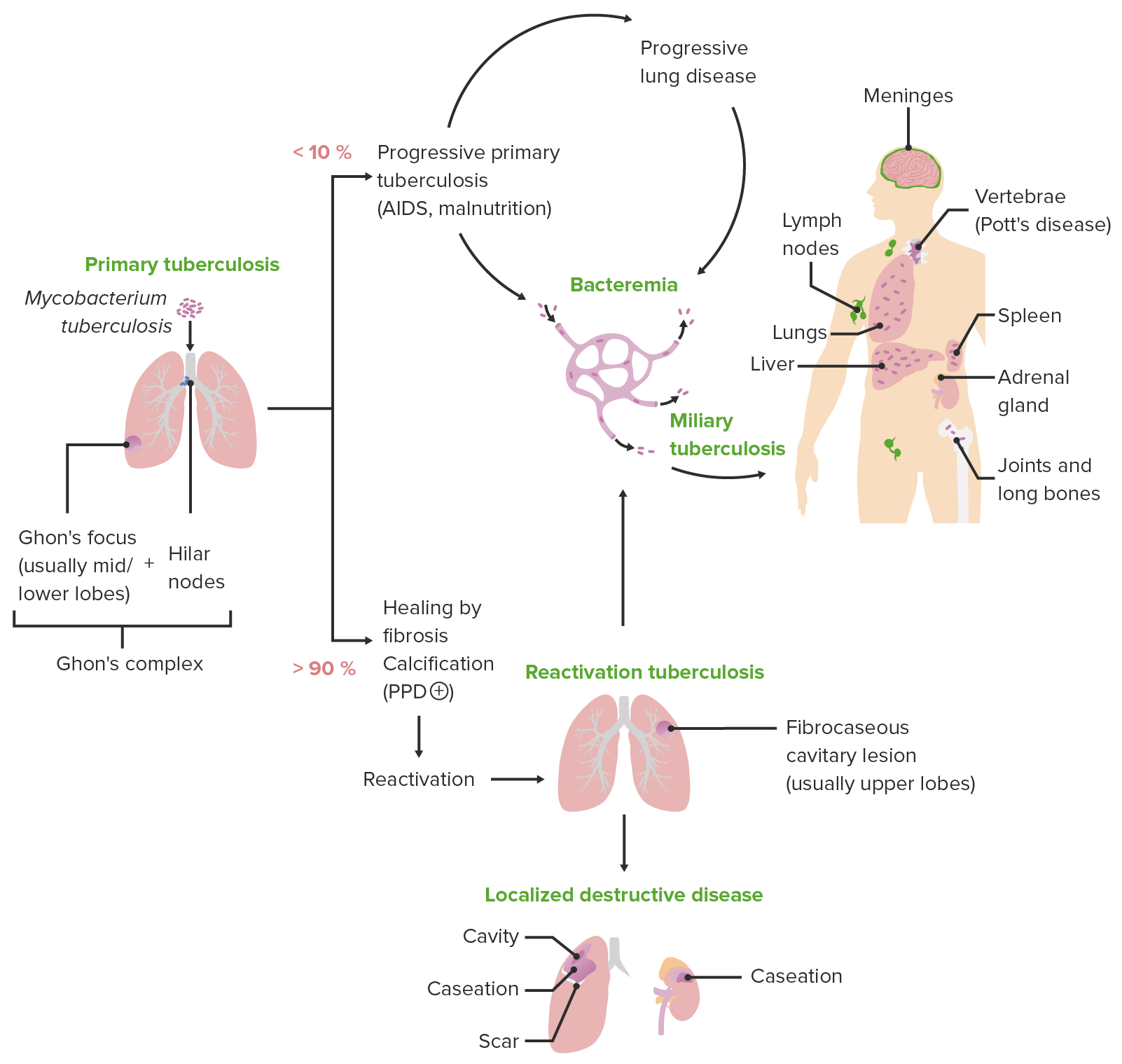
00:00 In this lecture, we’re going to discuss Tuberculosis. So, tuberculosis is caused by a bacteria that grows very very slowly and develops resistance easily and is hard to kill with antibiotics. 00:15 This is a tough condition internationally and a lot of effort is going in to treating it better. 00:21 <i>Mycobacterium tuberculosis</i> is the offending agent. This is an anaerobe and it’s very slow growing It only divides maybe once in 7 days. It’s an acid-fast stained organism. So we need an acid-fast stain in order to really be able to see it particularly well such as you can see on this slide. So, there are many typical presentations of tuberculosis and I want to run through them. Patients may develop pneumonia and there’s a classic picture to that, they may develop meningitis, they can develop osteomyelitis which we sometimes call Pott’s disease especially if it’s of the spine, they can develop an arthritis or a lymphadenitis which we will call scrofula, rarely they can develop genitourinary disease or peritonitis. TB can present in so many different ways. Spread of TB is mostly through person to person transmission through droplets, although there are some animals that can get it too such as lions and wildebeest and even some apes. Young children are less infectious with this disease. So it’s interesting if a child is infected it’s probably their parent that’s spreading it not the child. Children are usually not the source of TB from other people because they have less effective coughing. In the United States, fortunately, the risk is very low compared to many other countries who are suffering from tuberculosis. A few risk factors therefore are usually key to making the diagnosis of tuberculosis in children in the United States. The immigrants or people who’ve travel recently to endemic areas are at increased risk for tuberculosis. TB is more likely in immunocompromised patients especially those with HIV or inherent T-cell defects such as severe combined immune deficiency. Also, children who have been exposed to prisoners or IV drug users or even healthcare workers are at increased risk for getting this disease. So how does it present? Well, the respiratory illness presents with prolonged cough, respiratory symptoms and fever usually for more than 14 days. Patients may present with meningitis and usually also have risk factors for tuberculosis. If they have involvement of their brain and encephalitis, they may present with CNS symptoms such as seizure. 02:56 Patients with lymphadenitis will typically present as patients who have gone through multiple rounds of antibiotics for a presumed bacterial lymphadenitis and nothing is working. Patients late can present with bony abnormalities or joint effusions consistent with tuberculosis and that’s usually in the context of a long history of respiratory symptoms. So the way we test for is called the PPD. This is also called alternatively the TST or the Mantoux test. We usually call this the PPD in the United States. So this is an injection of purified protein derivative or PPD into the skin very very finely into the subcutaneous layer. It’s then injected and we wait for a 72-hour period and we bring them back and we check to see if the skin is elevated. You’ll notice on this picture that there’s a pen mark. What this person was doing is they were drawing lightly on the skin and they waited for the pen to get stuck on an elevated piece of skin. They're not just looking for where the redness occurs, they are looking for where the edema or swelling occurs. So if they’re measuring this correctly, you can see how the pen line on the left side of the picture doesn't make it all the way to the red spot, it stops early. That’s the correct way to check the size of the PPD. It’s not the redness, it’s where the swelling is and a ballpoint pen is a great way to do this. So this person had a measured 24 mm PPD test. Well that’s great but what’s normal? So what’s normal depends on the clinical constituency of the patient you’re taking care of. In other words, certain patients have certain numbers that are considered normal or abnormal. So in some patients, anything more than 5 mm is considered abnormal and evidence for exposure to tuberculosis. This is true in patients with HIV, patients who have a recent known contact with tuberculosis, patients who have a chest x-ray that’s consistent with active tuberculosis, or patients with immunosuppression say for example someone on chronic steroids. For most of us, 10 mm is the cut off. This is true for patients who are recent immigrants from prevalent areas, for IV drug users, for residents from dense populations such as cities, for patients with any risky condition where we worry this could be tuberculosis, for children who are less than 4 and for anyone who’s exposed to high risk adults such as prisoners, healthcare workers who specialize in TB, etc. Then, there are some people for whom more than 15 is considered abnormal. We allow a little bit more space. That’s basically everyone else. So you look at your risk factor and you decide in advance how big will I let this PPD be then you implant the PPD, wait for a 48-hour to 72-hour window and then check it again. Measure it with a ballpoint pen and this is how big it should be. There is another test that is a little more expensive but is a reasonably good test to know about and that’s called the Interferon gamma release assay. 06:18 Alternatively, some places called this the QuantiFERON Gold test because that’s the company name. Whatever the case may be, the advantage of this is there is only 1 visit rather than going in and getting the PPD and then coming back to have it read, it’s just 1 visit but it is more expensive. It tends to have false negatives in children under 5 years of age so we don’t like to use it in that age group but it is the best test for someone who got a BCG vaccine. 06:47 Remember, patients who got BCG vaccines we interpret their PPDs generally the same as those who didn’t but this may be a good test because if this test is negative we may say “You know what, this is probably their vaccine and this is not a positive response to the PPD test.” Lastly, we can certainly culture for their organism. If the patient is symptomatic, we’re going to try to get cultures. That’s incredibly important because with cultures we can now determine what the sensitivity of the organism is and choose the best medical regimen for that patient to get better. The problem with cultures is, like I stated earlier, this bacteria grow very slowly so this takes time. Gastric aspirates are better than sputums in young children. In adults, you’re told to get sputums. Kids can’t make sputums very effectively so we really rely on gastric aspirates. 07:45 So what we’ll do is in the morning when they’re waking up we’ll insert an NG tube and suck out some stomach contents. That’s going to better yield than sputum in these young kids but the yield isn’t great, it’s only around 40% but we will try often for days in a row because the value of getting the organism itself and knowing what it’s treatable. We additionally can make the diagnosis through chest x-ray, a few key findings which you might note. One is the Ghon complex. 08:15 This is mediastinal node associated with pulmonary disease where there is a calcified lesion within the context of that lymph node. This is classic for the disease and remember the name Ghon complex, you may see that on exam. Alternatively, patients may present with infiltrates in the lung and there are a few things that you need to understand about that. Remember that the bacteria, <i>Mycobacterium tuberculosis</i>, is an obligate aerobe. It prefers to grow in the upper areas of the lung that have a higher amount of oxygen concentration. So as a result, the primary infection is lower down because that’s the direct route in the lungs where you have your primary infection but reactivated infections, those that have been dormant for a long time and come back are usually upper lobe. In children, more common than that is the miliary pattern. This is much more common in children than it is in adults and here’s an example of that. Also, patients with a large heart may have TB pericarditis which is something you should look for. If a patient has a positive PPD and a negative chest x-ray, this is called a latent TB infection. These patients have been exposed, their immune system has seen and fought tuberculosis but right now nothing is going on.
About the Lecture
The lecture Tuberculosis (TB) in Children: Pathology & Diagnosis by Brian Alverson, MD is from the course Pediatric Infectious Diseases. It contains the following chapters:
- Pathology of Tuberculosis
- Diagnosis of Tuberculosis
Included Quiz Questions
For what patient population is a PPD induration of 7 mm considered abnormal?
- Patients with HIV.
- Patients living in densely populated areas.
- Patients living in contact with high-risk individuals.
- Patients 3 years old or younger.
- Patients who are IV drug users.
Which of the following is the test of choice to confirm a true tuberculosis infection in a patient who has had a BCG vaccine and results positive on PPD?
- Interferon-gamma release assay
- Chest X-ray
- Repeat PPD
- Blood culture
- Sputum Gram stain
Which of the following is considered an abnormal PPD result for a nurse working in a tuberculosis endemic area?
- 11 mm induration
- 9 mm erythema
- 8 mm induration
- 5 mm erythema
- 7 mm induration
To diagnose a 3-year-old child with tuberculosis, what sample should be obtained and sent for culture?
- Gastric aspirate
- Sputum
- CSF
- Urine
- Blood
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I particularly liked the remarks regarding the interpretation of the PPD test.