Playlist
Show Playlist
Hide Playlist
Meningitis in Children: Pathology and Diagnosis
-
Slides Meningitis.pdf
-
Download Lecture Overview
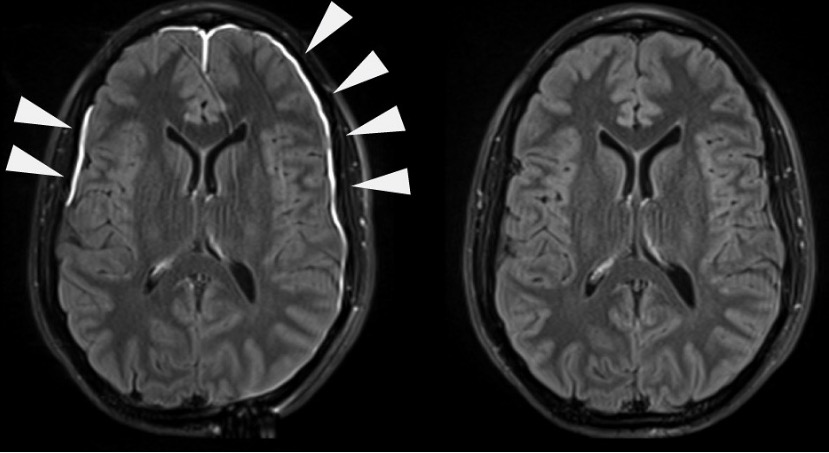
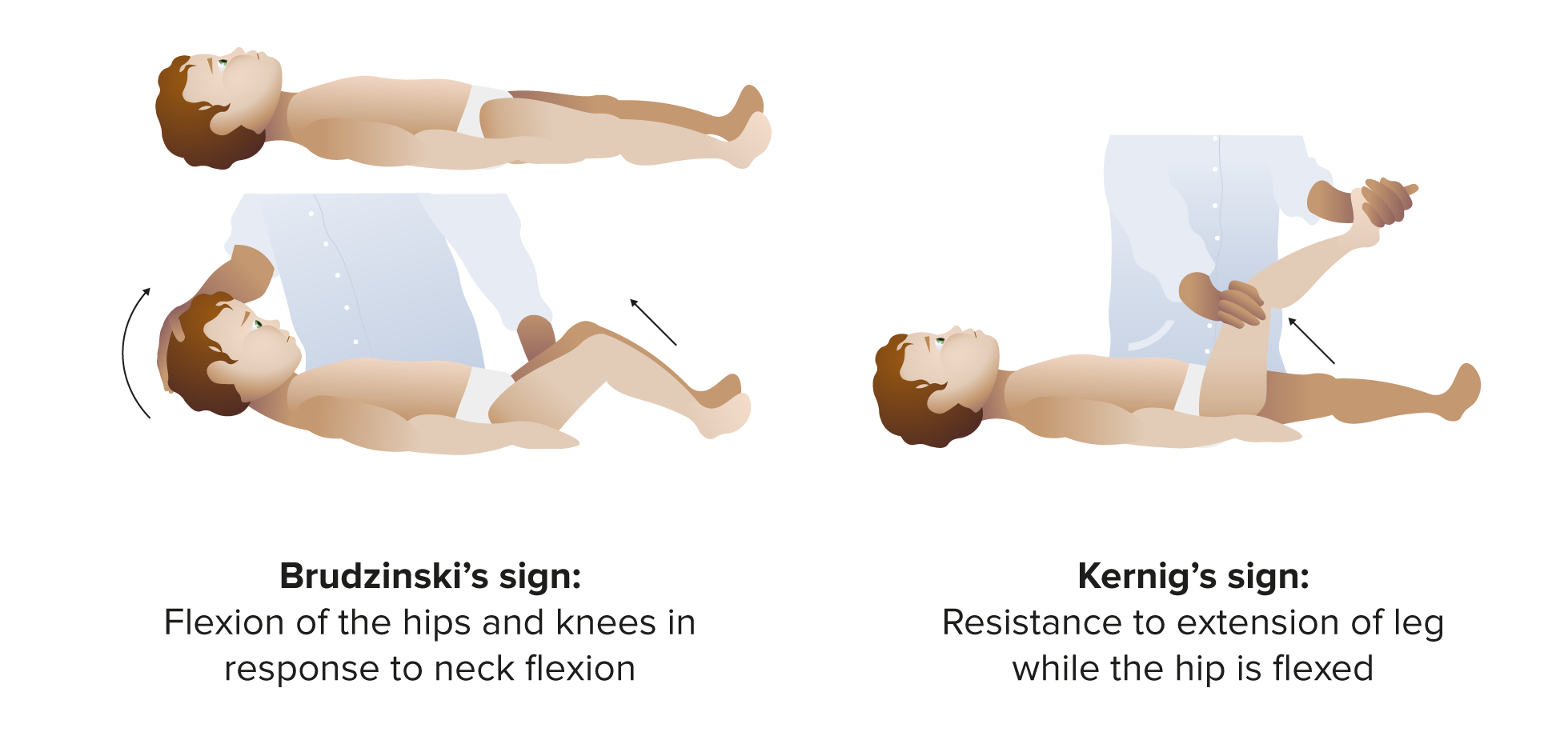
00:00 In this lecture, we're going to discuss Pediatric Meningitis. Vaccines have been a valuable tool in reducing rates of meningitis in children. Specifically, the <i>H. flu</i> type B vaccine has virtually eliminated <i>H. flu</i> B meningitis from the United States. The anti-streptococcal vaccines have been very beneficial at reducing substantially but not eliminating rates of streptococcal meningitis. 00:31 The <i>Neisseria meningitidis</i> vaccine which is primarily given to children before they go to college has been very effective at reducing college outbreaks of <i>Neisseria meningitidis</i> meningitis which is highly infectious and highly dangerous. Additionally, both the varicella and the influenza vaccines reduce rates of viral encephalitis and viral meningitis. So, how does meningitis happen? Well, we have to recognize that bacteria are constantly colonizing our nasopharynx. During some freakish event, the bacteria invades with the mucosa and get in to the bloodstream and then they generally get up to the brain and they may penetrate the blood-brain barrier. This is how this infection happens. It will present in infants differently than it will in older children. Infants or newborns will present with fever, irritability and lethargy, excessive crying and either hypo- or hyperthermia so a low temperature or a high temperature. What's key is the irritability. We usually see that as predominant and we worry about this in pretty much all young infants with fever as our rule out sepsis protocol. In terms of older children, they will present with fever but these children will more often have vomiting, headache, photophobia, confusion and what's key is a stiff neck. If you have a patient like that with a stiff neck and unwillingness to touch their chin to their chest, you definitely should be worried about meningitis. Nuchal rigidity is the physical exam hallmark of this diagnosis and they usually have difficulty pushing their head forward on to their chest. You may further make the diagnosis by looking for the Kernig and Brudzinski signs. You recall what those are. Those are basically where the patient has difficulty raising the neck or the patient has pain while the doctor raises the hip. Patients may have petechiae and purpura that would be consistent with <i>Neisseria meningitidis</i>. Here is the Kernig and Brudzinski sign that I described. You can see Kernig sign where the hip is raised up and the Brudzinski sign where the head goes up and then the knees flex reflexibly. If you have a hard time remembering which is which, remember Kernig's is knee, k and k. In meningitis, we'll get some labs to try and make this diagnosis. Let's start with some non-specific labs. The CBC may be elevated in meningitis but it might not. So this is not a definitive test. We will often get a blood culture in meningitis and occasionally it will reveal what the causative organism is but the best culture is of the spinal fluid. In infants, we're also checking urine. We're checking it because we don't know whether this is a urinary tract infection, a blood infection, or meningitis. 03:42 What's key to understand is an unusual phenomenon in adults but is common in children which is that children with a urinary tract infection will get a low level sterile pleocytosis in the CSF. 03:56 What that means is a child with a urinary tract infection and lots of white cells in the urine may have a low number of white blood cells in their spinal fluid but not have meningitis. This highlights the need for getting the tap before giving antibiotics because if you get the tap after giving antibiotics, you sterilize the CSF and it will be impossible to distinguish a patient who has both the UTI and meningitis from a child who has a UTI and a sterile pleocytosis. So the test of choice for any child where you're concerned about meningitis is obviously a lumbar puncture and we're going to get that fluid and we're going to send it off to the lab. What are we going to send it for? Well, first we're going to send it for a gram stain. The CSF gram stain has a high false negative rate but a low false positive rate. What that means is if you see bacteria, you should be worried but if you don't you're about where you started. Let's also send that CSF for protein. 04:59 In bacterial disease, this is usually very high. We should also send that CSF for glucose. Usually, the bacterial disease, the glucose is low, less than 2/3 of whatever the serum value is. Likewise, we're going to send that CSF for a cell count and specifically ask about the number of white blood cells. Patients with meningitis will have a higher than 21 white count if they're under 4 weeks of age, 4-8 weeks it should be less than 11. In other words kids with meningitis will have more than 11 cells. After about 8 weeks we expect a normal patient to have less than 8 cells. 05:40 So more than 8, that's concerning.
About the Lecture
The lecture Meningitis in Children: Pathology and Diagnosis by Brian Alverson, MD is from the course Pediatric Infectious Diseases. It contains the following chapters:
- Pathology of Meningitis
- Diagnosis of Meningitis
Included Quiz Questions
Which of the following organism is most likely to cause meningitis presenting with purpura and petechiae?
- Neisseria meningitidis
- Streptococcus pneumoniae
- Influenza virus
- Borrelia burgdorferi
- Herpes simplex virus
Which of the following is NOT a common finding in infants with meningitis?
- Stiff neck
- Lethargy
- Irritability
- Hypothermia
- Hyperthermia
Which of the following accurately describes Brudzinski's sign?
- Patient's hips and knees flex reflexively when the neck is flexed towards the chin.
- Patient has pain when the doctor raises the hip.
- Patient has nuchal rigidity.
- Patient has photophobia.
- Patient has petechia and purpura.
What precaution should be taken to prevent sterilization of CSF and help differentiate urinary tract infections and meningitis?
- Perform spinal tap and then provide antibiotics.
- Provide antibiotics and then perform spinal tap.
- Perform urinalysis and then provide antibiotics.
- Provide antibiotics and then perform urinalysis.
- Provide antibiotics and then send for blood culture.
In an infant younger than 4 weeks, how many white blood cells must be seen in the CSF sample to indicate meningitis?
- > 21 cells
- > 5 cells
- >8 cells
- > 11 cells
- > 16 cells
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I particularly liked the differences regarding the age with the key features highlighted and the comments regarding the CSF values.
well explained quick summary, has all the important information, maybe adding lumbar puncture contradictions would be helpful, thank you for all the amazing lectures Dr. Alverson, they are very helpful in reviewing pediatrics