Playlist
Show Playlist
Hide Playlist
Bronchiolitis: Clinical Presentation & Management
-
Slides Bronchiolitis.pdf
-
Download Lecture Overview
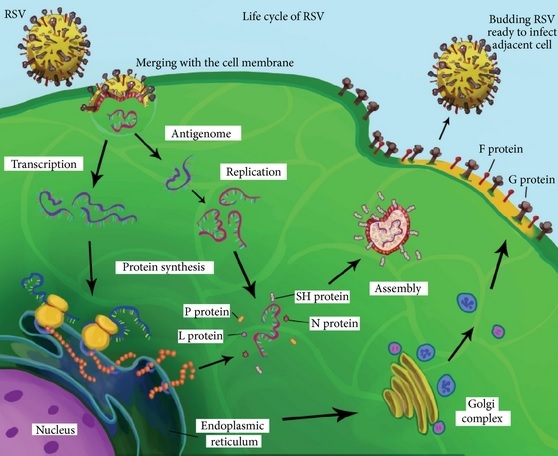
00:01 So what puts children at risk for bronchiolitis? Well, we talked about premature infants. 00:07 Children with congenital heart disease are more likely to have severe disease and more likely to be hospitalized. 00:14 Children with chronic lung disease of prematurity are more likely to be hospitalized. 00:19 Kids with cystic fibrosis are at increased risk for severe bronchiolitis. 00:23 Children with immunodeficiency and particularly severe immunodeficiencies, such as severe combined immunodeficiency or SCID, are at increased risk for hospitalization. 00:33 And as we stated, children who have been exposed to smoking are at increased risk for hospitalization for bronchiolitis. 00:40 So you’ve got the patient, you’ve diagnosed bronchiolitis based on your clinical exam and history. 00:47 What are you going to do in terms of treating them? Well, first as you can see on this slide, you are not going to give this child albuterol. 00:54 As tempting as it may be, if this is bronchiolitis, albuterol does not shorten hospitalization, does not decrease the likelihood of being hospitalized in the first place, and it does make children jittery. 01:08 So it’s generally ineffective. 01:11 Some people are concerned that there may be a small percent of children who would respond to albuterol and who like to then give a trial of albuterol. 01:20 The latest American Academy of Pediatrics guideline says not to do that because we’re going to end up overusing the drug and causing so many people to become jittery and not helping anyone in terms of their length of stay in the hospital. 01:35 Steroids have no role in bronchiolitis. 01:38 If you suspect the patient has bronchiolitis, you should not administer steroids. 01:43 They do not shorten length of stay in the hospital, they do not reduce rates of readmission to the hospital. 01:49 They really have no benefit. 01:53 So what does work? The most important thing to do in a child with bronchiolitis is superficial suctioning with saline drops. 02:03 Before feeding or before initiation of any treatments, if they are warranted and as needed, you’re going to give saline into the nasal passage and you’re going to teach the parents how to suck it out. 02:16 Notice I said this is a great opportunity to teach and empower the parents. 02:22 We are shifting our paradigm in the last ten years away from drugs in the management of this condition and we still need to empower parents to help their children get better, and teaching them to adequately suction their child is a mainstay of therapy. 02:39 It is extremely effective at reducing symptoms. 02:42 In one study in Cincinnati, children who are superficially suctioned every four hours also had a shorter length of stay. 02:51 You want to avoid deep nasopharyngeal suctioning with a catheter because it’s irritating, extremely painful, can cause bleeding, and if repeated frequently can cause trauma. 03:01 However, in the acute setting of a severe respiratory distress, it’s absolutely indicated because it can help in the emergent setting. 03:12 So superficial suctioning, we used to use those little blue bulbs and this new device is taking the world by storm. 03:20 There are self-administered suction devices for parents to use on their children. 03:27 One end is applied to the nose and the other end the parent sucks in vigorously to apply that suction force into the nose area. 03:37 So first they give the saline drops, then, they suck it out. 03:40 It’s common for having to -- You have to teach the families how to do this. 03:45 What’s key here is that the mucus that’s being sucked out will not get into the parent’s mouth and it’s important to tell them that. 03:52 My experience is almost all parents who try this once will never go back to the blue suction bulb, which is largely ineffective. 04:02 So one thing that we worry about in children with bronchiolitis is their pulse oximetry. 04:07 We worry about, are they getting enough oxygen. 04:10 And I want to rethink this paradigm because there are a lot of people who worry about oxygen and that fear of oxygen is driving actually unnecessary care and unnecessary hospitalization. 04:22 So keep in mind a baby in utero is around 60% to 65% saturated hemoglobin, so below 65 is definitely dangerous. 04:32 I would not recommend that. 04:34 At 18,000 feet, if you were to climb right now up a mountain, your normal pulse oximetry would be around 75%. 04:43 You wouldn’t be dead, but you’d certainly be a little hurting for oxygen. 04:47 So certainly, 75 is not a zone where I feel comfortable with a baby hanging out. 04:53 But nobody really knows what is safe for an infant and infants routinely and normally desaturate all the time. 05:02 The average desaturation for an infant who is well, who is less than four months, who has a pulse ox probe left on their finger for 27 hours is well into the mid-80s, so normal babies will desaturate. 05:17 And we need to be careful about measuring too much oxygen and worrying too much about it. 05:21 This may be a child who is not actually having a problem. 05:25 So keep in mind if we were to take the oxygen-hemoglobin dissociation curve, and if you recall, this is a curve which has on one axis the pressure of oxygen that’s available in the room and on the other axis what percentage of hemoglobin molecules are actually saturated, and we start in a situation where all of the hemoglobin molecules and we start reducing the amount of oxygen, it’s like this car is going along for a while and then suddenly takes a dive down the hill. 05:56 Once a pulse ox machine gets down to around 90%, further reduction in available oxygen is going to cause a much more rapid deceleration, and that’s why most hospitals use 90% as a safe level. 06:11 So how else should we manage these children? Well, it’s key in the hospital setting that we should engage in handwashing and we should gown, glove, and mask to prevent spread of the illness. 06:21 In the United States, 30% to 40% of children hospitalized during the RSV season for another reason get RSV while they’re in the hospital. 06:32 The risk of infection is related to their length of stay, and high-risk children are more likely to be in the hospital anyway. 06:39 So in the hospital setting when you’re seeing these patients, we need to wash our hands, gown, glove, and mask. 06:46 When do we decide it’s safe for them to go home? Well, we generally decide when their respiratory rate is safe keeping in mind that, especially with RSV, they can have a sort of happy tachypnea, where they’re not in distress and breathing a little bit faster in the 50 to 60 range. 07:03 Those children may be okay to go home. 07:05 They should have no increased work of breathing, no accessory muscle use, no retractions, flaring, or grunting. 07:13 They should be feeding well, they should not need IV fluids or NG fluids to stay hydrated, and the parents should know how to suction effectively. 07:22 And when they have met these criteria, they’re probably safe to go home. 07:26 Preventing bronchiolitis is key. 07:29 And so we encourage families to breastfeed because that will improve the likelihood that the child has a minimal sickness when they’re exposed to the virus that their mother is also exposed to. 07:41 We would love for children to not be exposed to secondhand smoke And in the home, alcohol-based hand sanitizer can help prevent spread of illness to children and infants who are prone to more severe bronchiolitis. 07:58 There is some emphasis on medical prevention of bronchiolitis and this is because it is the number one cause of hospitalization in children. 08:07 This isn’t a death prevention situation such as the influenza vaccine or the measles vaccine. 08:16 This is really more to prevent use of hospital resources. 08:22 So one drug that’s been made available and is being used currently in the United States is palivizumab, which is an antibody designed against the RSV. 08:31 This drug is incredibly expensive. 08:33 It costs roughly $10,000 for a child to go through the winter season and get it. 08:38 It is very safe, but it’s not cost-effective. 08:43 In other words, we have to spend about $300,000 to prevent one hospitalization, which costs on average $10,000, and because it doesn’t prevent mortality from RSV, this drug is likely to go away in the next several years. 09:03 Right now, it’s restricted for use in severely premature infants and infants with congenital heart disease. 09:10 However, even in these populations, this drug is not cost-effective. 09:14 It’s effective, it’s not cost-effective. 09:18 So there are some new medications that are coming out and I don’t know which ones of these are likely to be promulgated and accepted in the United States. 09:27 There is an oral anti-RSV agent that is being worked on currently. 09:32 There is nasally administered immunoglobulin that’s currently being studied. 09:38 And also, there is a maternal vaccine where they would then also give a booster vaccine to the baby. 09:45 One new therapy that is come up about in the last several years for infants with bronchiolitis is high flow nasal canulla This is a device, that blows air into the babys nose at relatively high rates. 10:00 Most centers use a rate of 2 liters per minute per kilogramm usually with a maximum of around 20 or 30 liters per minute. 10:08 The idea here is, that we can assist with breathing through several purposed mechanisms. 10:15 The most commonly purposed mechanisma are number 1: That the high flow nasal canulla is providing positive pressure, which releaves airway out the lactal system; We see so commonly in bronchiolitis. 10:29 And the second purposed method is that the baby is not re-inhaling their exhaled carbondioxid Remember that high levels of carbondioxid put you into respiratory distress, because that carbondioxid is turned into acid - carbon acid. 10:46 Well, when babys are breathing with bronchiolitis, they often have very shallow breaths, that are very rapid. 10:52 And so what can happen is, they can actually end up inhaling the CO2 that they just exhaled, because it's still sitting in the airway deadspace. 11:00 The high flow nasal canulla may act a little bit like blowing a leavblower into a barreld leaves. It'll pump out the CO2 in that airway deadspace and prevent a re-inhalation of that carbondioxid. Thereby reducing the amount of acid in the blood; Thereby reducing the respiratory distress. 11:18 So this method came about and is now almost ubiquitous at least in the united states in the management of these infants. And i've actually seen it used in developing countries as well. 11:30 The challenge is that in 3 perspective randomized control trials, it hasn't helped at all. 11:36 So it does not seem to change liked of stay, it doesn't seem to change rates of readmission, it doesn't change the likelihood that a baby gets inturbated. 11:45 It really has no impact on the child, but all of us clinically feel like we've seen some kids who respond. 11:53 So, the only thing i can say about this is, that there are a lot of people who feel like it helps some babys. 11:58 We certainly shouldn't use it as a way of prolonging liked of stay unnecessary. In other words: don't spend a lot of time weaning it or making sure they're ok of high flow nasal canulla. 12:10 One controversy is that, because in many centers in the united states high flow nasal canulla is only available in the ICU Over the last 10 years, we have doubled our rate of admitting children to the ICU, without much benefit which is resulted in a dramatic increasing cost of care, without much benefit. 12:30 So this fairly controversal therapy is ubiquitous. You'll see it most centers that are managing bronchiolitis. 12:37 And yet we don't really have a real handle on how to identify which infants will benifit, or to what degree they are benefitting from this therapy. 12:46 All of these therapies are geared towards reducing the rate at which children are hospitalized in the United States. 12:54 The goal is to reduce cost, but not necessarily to save lives. 12:59 We’ll see where this goes. 13:01 This is an active area of research right now. 13:04 Thanks for your attention.
About the Lecture
The lecture Bronchiolitis: Clinical Presentation & Management by Brian Alverson, MD is from the course Pediatric Pulmonology. It contains the following chapters:
- Risks and Treatment
- Pulse Ox
- Medications
Included Quiz Questions
Nobody knows what is a truly “safe” level of hypoxia for an infant when checking an O2 saturation, but what number do most hospitals use?
- 90%
- 88%
- 92%
- 94%
- 96%
An infant is at high risk of bronchiolitis if he has any of the following, EXCEPT?
- Hydrocephalus
- Congenital Heart Disease
- Cystic Fibrosis
- Chronic Lung Disease of Prematurity
- Immunodeficiency disorder
Which of the following must be avoided unless we have a patient with severe Bronchiolitis?
- Deep nasopharyngeal suctioning
- Superficial suctioning with saline drops every four hours
- Periodic pulse oximetry
- Parent education on how to use the suction device
- Handwashing and use of gloves by all the contacts
Which of the following is NOT a criterion for the discharge of a patient with Bronchilitis after hospitalization?
- Absence of fever
- 'Safe' respiratory rate
- Not needing any IV or NG fluid
- Parents know how to use suction device effectively
- Absence of labored breathing
Bronchiolitis is a common respiratory problem, especially during the winter season. All of the following are effective preventive measures for Bronchiolitis, EXCEPT?
- Antiviral medication prophylaxis
- Breastfeeding
- Avoidance of second-hand smoking
- Routine use of alcohol-based hand sanitizers at home
- Avoidance of contact with a patient with bronchiolitis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Another great lecture, where all the following are covered: - Myths: oxygen, etc. - Asthma vs Bronchiolitis - Pavalizumab - Current literature on brochiolitis - Experience from an advanced practitioner I work in a Swiss hospital and even though we follow as much as possible the AAP recommendation, we are not all the time up-to-date.