Playlist
Show Playlist
Hide Playlist
Colon Cancer: Diagnosis and Management
-
Slides Colon cancer General Surgery.pdf
-
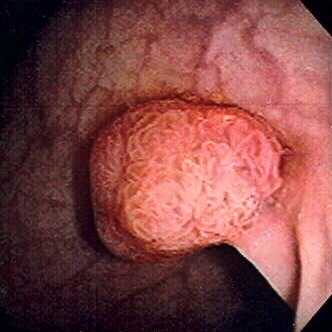
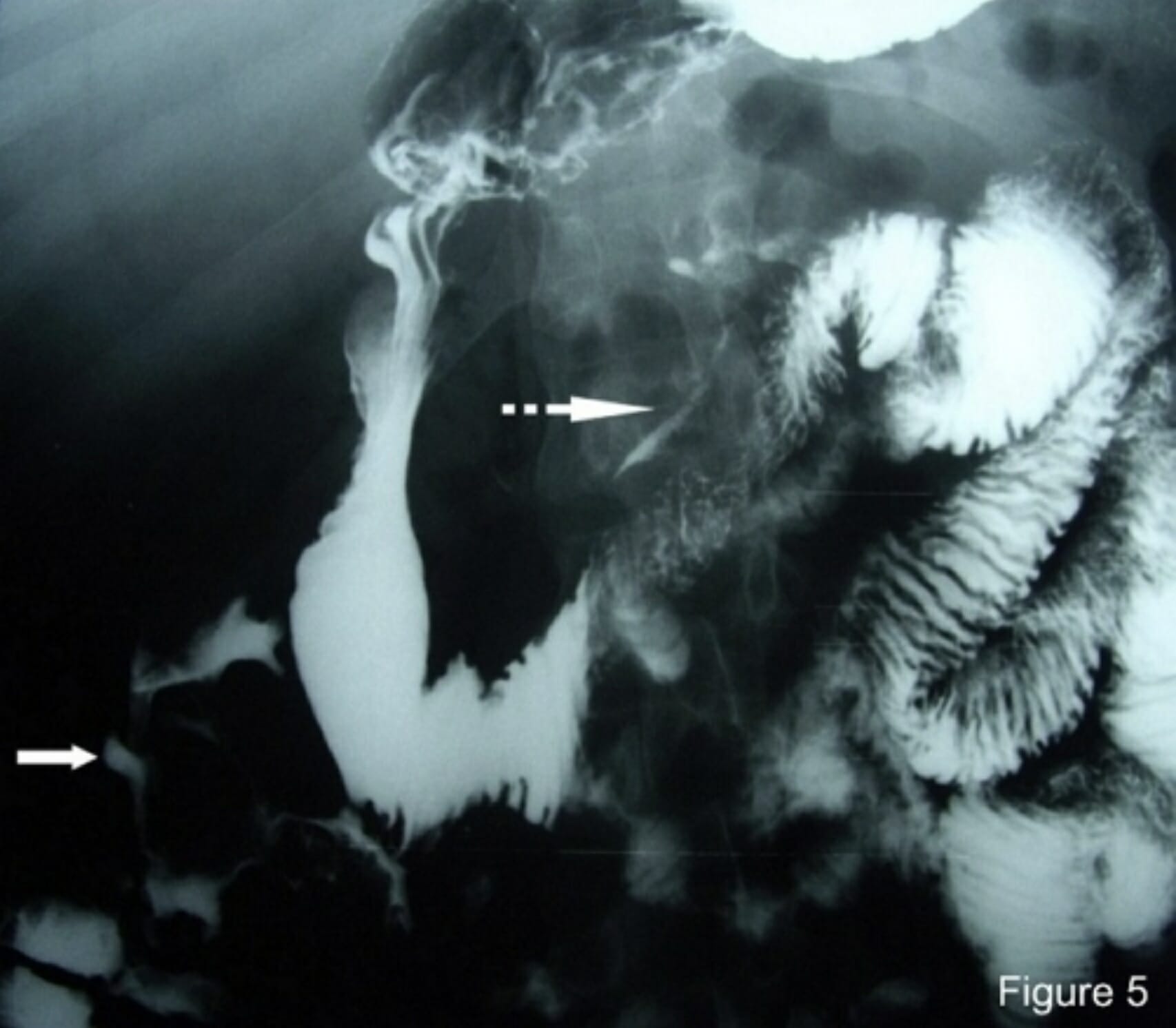
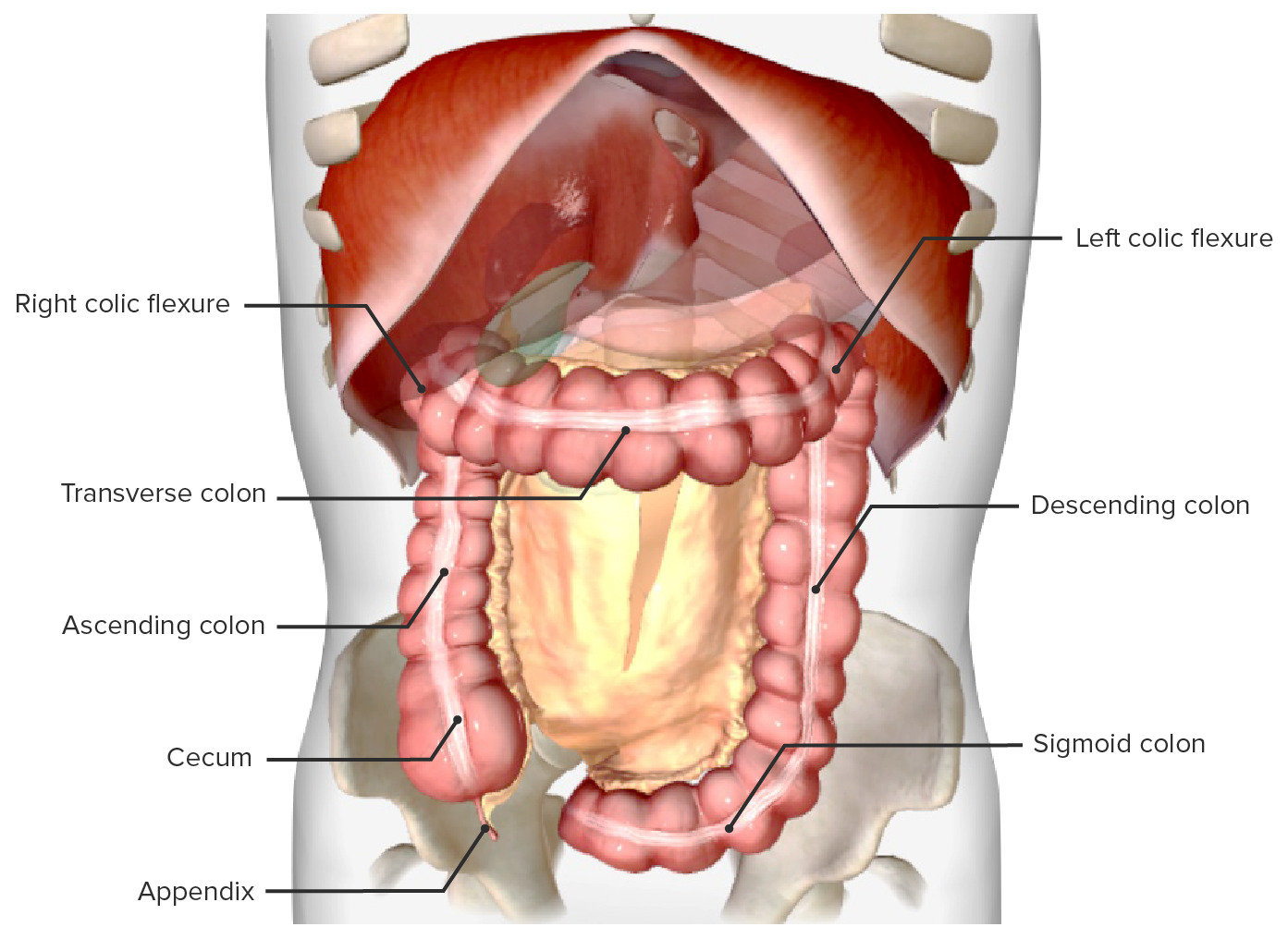
Download Lecture Overview
00:01 I can’t overstress the importance of colonoscopy and screening colonoscopies. We typically do this in an outpatient setting after a bowel prep. A bowel prep includes drinking some sort of an agent that will do a volume cleansing of the colon as well as allow an easier manipulation and visualization of the colon. 00:23 Patients are placed on their side under visualization. Oftentimes, believe it or not, patients are awake for this procedure so they can actually look at the entire colonoscopy as it is being performed. 00:34 Now, not every patient requires a colonoscopy. There are centers that will either do a barium enema or fecal occult blood testing. Only if the fecal occult blood testing is positive will they pursue either a flexible sigmoidoscopy or a colonoscopy. Nevertheless, colonoscopy is quite standard. With a normal colonoscopy with averaged-risk patients, you don’t require another one for another 10 years. 01:01 In cases of incomplete colonoscopy results, the PILLICAM can be used, which is a small camera in the shape of a pill that the patient swallows. 01:10 It takes pictures that can be used for diagnosis. 01:14 Now that you've diagnosed colon cancer, what’s the next step? Well, before offering surgery, we have to make sure that the patient has not metastasized to other organs. Liver function testing is very important because it is a common area of metastases particularly alkaline phosphatase. Additional metastatic workup can include chest X-rays, cross-sectional images. On this set of abdominal CTs, you’ll notice that multiple liver lesions are showing. The volume of lesions is suggestive of metastases as opposed to a solitary liver lesion. Here’s a description of what happens in surgery. We do what’s called an oncologic surgical resection which means we want to take the segment of the colon that contains the tumor obviously but we also want to take its draining blood supply as well as very importantly its lymph node basin. Now as you progress from the left of the slide to the right of the slide, you’ll notice that we’re going from the right side of the colon to the left side of the colon. Some patients may require 5-FU based chemotherapy depending on the depth or penetration or stage of the cancer. Recall that colon and rectal cancer are treated very similarly except for radiation. We can’t radiate colon without irradiating the small intestines and therefore, it has had limited utility. However, the rectum can be irradiated and therefore, rectal cancer is often treated with radiation. 5-FU, leucovorin are both common chemotherapy bases. Tumor depth is very important. This is also an important review of the different layers of the colon. T1 disease invades submucosa. T2 invades the muscularis propria commonly called the MP. T3, into pericolonic fat. And T4 is a full-thickness penetration of the surface of the visceral peritoneum or frank, direct invasion to surrounding organs whether that’d be a bladder or prostate. Stages of the colon go by the AJCC TNM staging process. You can look that up on the internet. 03:36 Based on the stage of the colon cancer, whether it’s a stage 1 or 4, has significant five-year survival prognosis. You can see that patients with stage 1 or early disease have far better five-year survivals than a patient who has stage 4 or metastatic colon cancer. We talked about the importance of colonoscopy. 04:01 It should be conducted every 10 years beginning at the age of 50. If it’s normal, then one can forego another one for 10 years. There’s an interesting subset of patients where we talk about colonoscopy before a surgery. This is the classic patient who presents with potential right lower quadrant abdominal pain. You get cross-sectional images, concerned for either diverticulitis or appendicitis and yet on the cross-sectional image, you see what’s called a phlegmon. A phlegmon is a collection of inflammation that hasn’t completely progressed to an abscess. These patients may eventually develop a disease that requires surgery. However, before offering surgery to those patients, you must offer them a colonoscopy to search for colon cancer. This is the classic scenario of a right lower quadrant phlegmon if presented to you on the examination as a clinical scenario that patients require screening for colon cancer before definitive operation whether it’s diverticulitis or appendicitis. 05:03 Let’s review some very high-yield information. Again, Lynch syndrome and the multiple Amsterdam criteria as well as the Bethesda criteria. Remember the very predictable pattern of gene mutation from polyp to cancer sequence. Recall that patients with FAP and multiple colon polyposes have near 100% risk of colon cancer and therefore, we offer surgery to them. Thank you again for joining me on this discussion of colon cancer.
About the Lecture
The lecture Colon Cancer: Diagnosis and Management by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which statement is TRUE?
- A colonoscopy is typically an outpatient procedure where the patient will discharge home after the procedure the same day.
- A colonoscopy should be done only after a positive fecal occult blood test.
- Screening colonoscopies should be repeated every 5 years if results are normal.
- Colonoscopy procedures require the patient to be under general anesthesia.
- Colonoscopy and barium enema have similar sensitivity and specificity for the diagnosis of colon cancer.
All of the following are used to diagnose metastatic colon cancer EXCEPT?
- Colonoscopy
- Liver function tests
- Chest X-ray
- CT scan of the abdomen
- Serum alkaline phosphatase level
All of the following modalities of treatment can be used for BOTH colon and rectal cancers EXCEPT?
- Radiotherapy
- Oncologic surgical resection
- 5-FU chemotherapy
- Leucovorin chemotherapy
- Trametinib chemotherapy
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
very well explained but what about dukes astler classification for tumor penetration and linfatic afectation.