Playlist
Show Playlist
Hide Playlist
Hypercoagulability as a Paraneoplastic Syndrome
-
Slides CP Paraneoplastic Syndromes.pdf
-
Download Lecture Overview
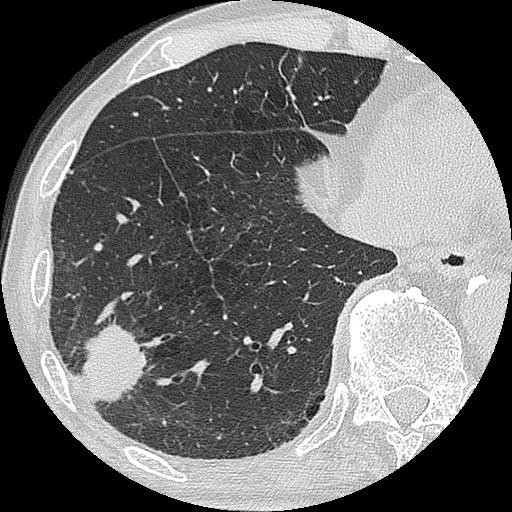
00:01 Next up, hypercoagulability. 00:05 So this is basically an increased risk of thrombosis because we have activated one aspect of Virchow's triad. 00:13 We have made the host hypercoagulable, and there are a variety of ways that we can do this, but when it happens, you may get deep venous thrombosis, then with pulmonary embolization, or you can get nonbacterial thrombotic endocarditis, the formation of thrombi on valves that can then embolize and cause injury someplace else. 00:40 So there's an increased risk of both of those in the setting of a hypercoagulable state driven by malignancy. 00:47 The mechanisms include the tumor, causing extrinsic vascular compression, and/or even invasion into a vessel. 00:55 And when that occurs, you're more prone to forming a thrombus in that location. 01:01 Tumors and endothelial cells that are driven by tumors through the vascular endothelial growth factor, basic fibroblasts derived growth factor etc, will produce more tissue factor. 01:15 Remember, tissue factor is going to be an important component of the extrinsic coagulation cascade. 01:22 Because of the factors being made, and the inflammation that results from malignancy, you will see increased platelet activation and there will be increased levels of platelets because we will increase thrombopoietin synthesis within the liver. 01:40 The tumor has on its surface a variety of molecules, of which phosphatidyl serine, one of the phospholipid components of the membrane will be expressed at higher levels in tumors and in tumor vasculature. 01:54 And that will support the activation of the coagulation cascade, as we've talked about in previous talks. 02:03 Again, the inflammation, that same inflammation such as Interleukin-6 that's driving the production in the liver of hepcidin, it's also driving in the liver the production of coagulation factors VIII, fibrinogen and von Willebrand factor and so that's going to increase the coagulability of blood. 02:23 And finally, because the tumor and tumor vasculature expressing higher levels of plasminogen activator inhibitor, we will see a tendency to a more prothrombotic state. 02:36 So the endogenous fibrinolysis that normally occurs will be inhibited by that plasminogen activator inhibitor-1 expression. 02:44 So there are a lot of different ways to that we're getting hypercoagulability. 02:47 How does this play out? So I mentioned nonbacterial thrombotic endocarditis. 02:52 What you're seeing on the left hand side is a mitral valve and there's a big goober otherwise known as a thrombus. 03:00 Nonbacterial endocarditis thrombus on the surface of that. 03:05 This actually happens because we are hypercoagulable,and if you think about it, the normal valve leaflets are clapping up against each other 60, 70, 80 times a minute. 03:17 And so normal valves are expressing or being exposed to two of Virchow's triad all the time. 03:25 One is the trauma of the valve leaflets closing against each other, and the second is the relative areas of stasis. 03:31 Each time a valve closes, there's a little area of stasis. 03:35 Now if we superimpose on top of that, a hypercoagulable state, we form this thrombus on the surface of the valve. 03:43 There is no infection in here. 03:45 In fact, the term non-bacterial thrombotic endocarditis is bad because there's no inflammation either, but we're stuck with that. 03:54 It's also called marantic endocarditis. 03:58 Either term is referring to these vegetations that are on the lines of closure of the valve and they are not causing any destruction, but they're not firmly attached. 04:11 And as the valves clap open and close 60, 70, 80 times a minute, pieces of this vegetation can flip off and go systemically, so can cause embolic disease on the left side of the body of the systemic vasculature. 04:28 What's been shown on the right hand side is just this vegetation, and it's a blend, platelets, fibrin and red cell vegetation with lines of Zhan that you can see there and it's just kind of lightly stuck on the surface of the valve. 04:44 So that's one of the complications of a hypercoagulable state. 04:47 Here's another major consequence of a hypercoagulable state. 04:53 The very left hand side panel is showing a deep leg vein so this would probably be the femoral vein in this patient who has now completely thrombosed that. 05:05 If that thrombus in the deep leg vein embolizes, breaks free and goes up towards the heart, the next capillary bed, the next vascular bed it's going to impact on is going to be in the lungs. 05:17 And what's shown in the middle panel is a very significant saddle embolus going into the right and left main pulmonary arteries. 05:30 What's being shown on the right hand side is just what that deep venous thrombosis would look like if we cut through it and you can see that there are laminations in it, so this is forming these lines of Zahn. 05:41 This is a patient who is hypercoagulable because of all the things that we talked about, and died as a result not per se directly of the cancer but of the paraneoplastic state associated with the cancer.
About the Lecture
The lecture Hypercoagulability as a Paraneoplastic Syndrome by Richard Mitchell, MD, PhD is from the course Cancer Morbidity and Mortality.
Included Quiz Questions
Which inflammatory-mediated molecules cause hypercoagulability in patients with cancer?
- Factor VIII and fibrinogen
- Hepcidin and fibrinogen
- Ceruloplasmin and hepcidin
- CRP and ferritin
- Transferrin and haptoglobin
Which statement is correct relative to cancer and hypercoagulability?
- Extrinsic vascular compression by a tumor increases the risk of thrombosis.
- Decreased tissue factor production by tumor and endothelial cells.
- Decreased platelet activation and accumulation
- Decreased expression of phosphatidylserine by tumor cells
- Elevated levels of protein C and S in serum
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |