Playlist
Show Playlist
Hide Playlist
Case: 56-year-old Woman with Left Extremity Weakness
-
Slides Diseases of the Motor Neurons.pdf
-
Download Lecture Overview
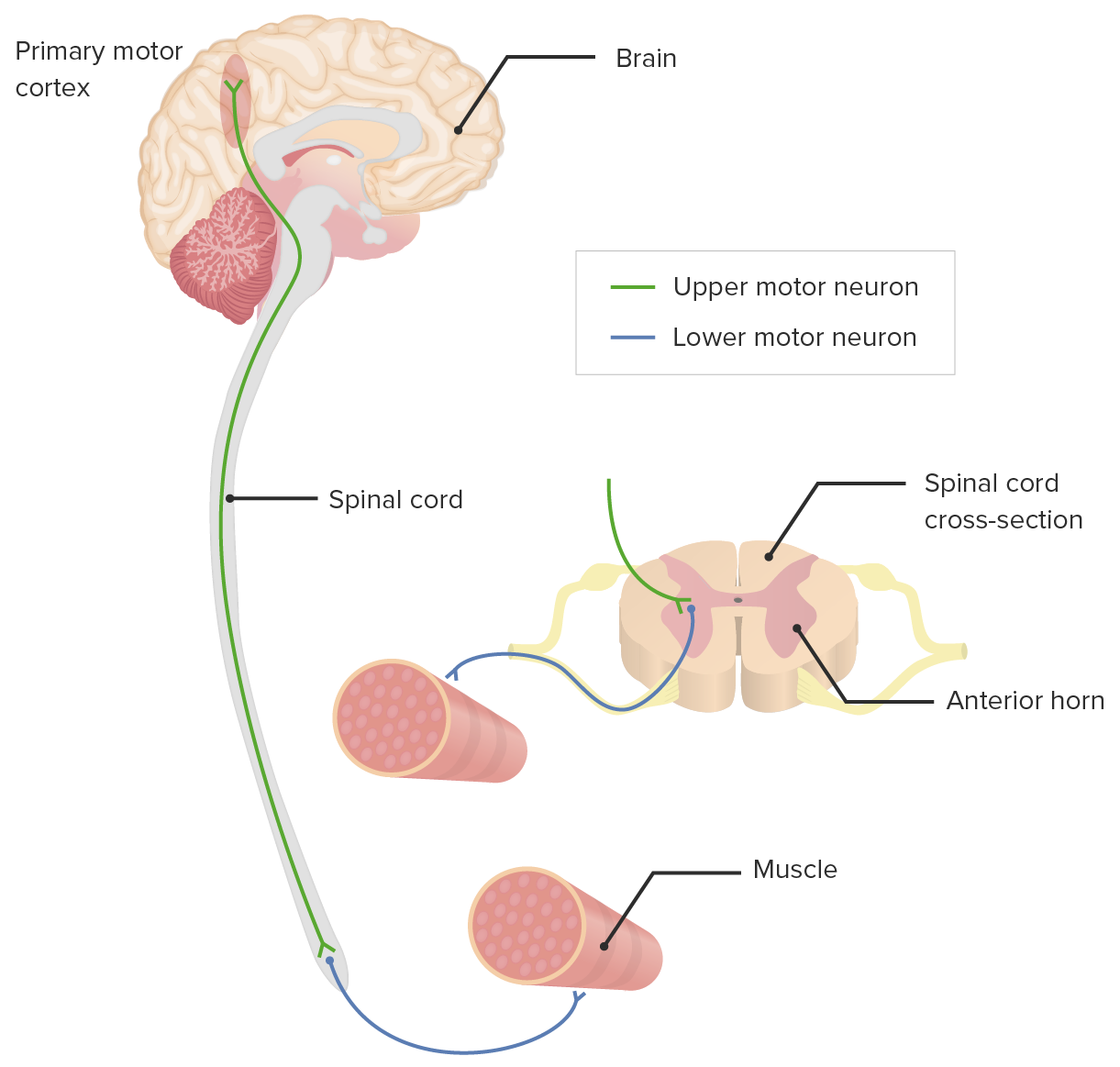
00:02 In this talk, we're going to review motor neuron diseases. 00:09 And let's start with a case. 00:10 It's a case of a 56 year old, presenting with left extremity weakness. 00:15 A 56-year old woman with past medical history of hypertension and hyperlipidemia presents with left extremity weakness. 00:22 This initially began in January with weakness in her left foot and ankle. 00:26 This remained stable until a motor vehicle accident in April. 00:30 The patient was evaluated for a whiplash injury at that time. 00:34 2 to 3 weeks following the accident, the patient noticed weakness progressing up the leg. 00:40 As of July, the patient had developed weakness in the left hand. 00:44 By October, the patient has started to use a walker and then a wheelchair to ambulate. 00:49 And in December, the patient presented with inability to grasp in the left arm, and atrophy of the hand muscles. 00:56 So we're seeing in this case, a steadily and relentlessly progressive illness that initially was thought to be due to this motor vehicle accident, but clearly is due to other underlying pathology.p So let's look at some of the key features. 01:11 First of all, the distribution. 01:13 This is left hemibody symptoms which could localize to a number of areas of the nervous system, central and peripheral nervous system. 01:22 We don't know the reflex exam, and that will be important to focus on in our examination, as well as sensory findings in this patient to figure out exactly where we localize these symptoms to. 01:32 And an important wildcard here is this gradual progression of symptoms which support a degenerative etiology, perhaps some rare inflammatory or infectious conditions, but really raise suspicion for a degenerative or inherited or congenital etiology that may be going on for this patient. 01:50 And then potentially a neoplasm, which could present with slow insidious onset of symptoms, particularly for from a benign lesion. 02:00 In this case there were no bulbar symptoms, no sensory loss, no neck pain, no bowel-bladder dysfunction and some chronic lower back pain that is likely unrelated to the symptoms that are leading to their presentation. 02:14 And importantly, bulbar symptoms would point us to the brainstem. 02:17 Sensory loss would suggest the presence of sensory peripheral nerve involvement or sensory fiber involvement in the central nervous system. 02:26 No neck pain suggests no degenerative changes in the spine that may be clearly offending in this case, and the lack of bowel bladder dysfunction is something we could see with a central cord syndrome. 02:37 So where do we localize these symptoms to? Well, like any neurologic presentation, we walk through those areas of the nervous system, it could be in the cortex or subcortex. 02:49 But importantly, motor and sensory fibers often run together in the cortex or sub cortex. 02:54 And this is really a motor predominant presentation. 02:57 There's no sensory symptoms. 03:00 Could be the brainstem, that's the next level down in layer. 03:03 But again, motor and sensory fibers travel in close proximity, and so it has to be very localized to a specific part of the brainstem and a degenerative or neoplastic or inherited syndrome in the brainstem would be quite atypical to present with that focal and localized symptoms. 03:20 What about the spinal cord? It could be a spinal cord problem, there are no bulbar symptoms, no cortical symptoms, the spinal cord is a consideration but again, we don't see sensory changes and sensory changes would be common in various spinal cord disorders. 03:34 Peripheral nerve, could it be peripheral nerve? It had to be a lot of peripheral nerves, the peripheral nerves to the leg, and to the arm and and throughout the entire hemibody, which is quite atypical, but we are hearing some symptoms that could suggest a peripheral nerve pathology. 03:49 We're not hearing things that suggest neuromuscular junction, or muscle but important considerations and patients presenting with motor predominant symptoms. 03:58 So let's take a closer look at this patient's physical exam. 04:01 Her mental status was intact and cranial nerves were also intact, really putting brain subcortex and brainstem lower on our differential diagnosis or localization for this patient. 04:12 What about motor function? Strength exam showed left upper extremity weakness - 3 out of 5, Strength is at two out of five in the dorsal interosseous muscles in the hand. 04:22 The left lower extremity showed 3+ out of 5, Strength also weak to all muscle groups throughout the left lower extremity. 04:30 And right upper and right lower extremity were full 5 out of 5 strength. 04:33 We're seeing that clear asymmetry in this patient's presentation. 04:38 Bulk showed significant atrophy in the left hand telling us that this weakness, this problem had been going on for some period of time and likely is involving the peripheral nervous system. 04:50 Reflexes were 3+ throughout, upper and lower extremities bilaterally which is telling us there's also some central nervous system component to this. 04:59 And sensation was intact throughout, which is quite surprising. 05:03 With this this degree of weakness and these changes with reflexes, the presence of no sensory findings really point towards a motor-predominant disorder or a motor neuronopathy, the motor neurons appear to be affected Fasciculations are present within the left arm in multiple muscle groups and less frequently in the right arm. 05:22 Fasciculations are a peripheral nervous system or lower motor neuron finding and really point towards lower motor neuron pathology. 05:30 So we're seeing both upper and lower motor neuron findings. 05:35 So how would you characterize this condition? Is this an upper motor neuron disorder, a lower motor neuron disorder, a combined upper and lower motor neuron disorder or an extrapyramidal disorder? Well, this is really important to pick out of this case. 05:49 This is not just an upper motor neuron disorder, there's the presence of fasciculations which is indicative of lower motor neuron findings. 05:57 It's not just a lower motor neuron disorder, there's hyperreflexia throughout, which is indicative of upper motor neuron findings. 06:03 It's not extrapyramidal. 06:05 The classic extrapyramidal disorder is Parkinsonism, which presents with bradykinesia, postural instability, rigidity with or without tremor, and we have none of those findings in this case This is a pyramidal problem, the pyramidal system is affected. 06:19 And it's really a classic presentation of combined upper and lower motor neuron findings. 06:24 And in this case, we have upper motor neuron findings in the same location, same level, spinal level as our lower motor neuron findings which is highly suggestive of a motor neuron disorder. 06:36 So let's look at the workup for this patient which was quite extensive to look into all the potential causes of this presentation. 06:44 First, we see an MRI of the cervical spine. 06:46 This is a T2 sagittal image which shows some very mild degenerative changes in the cervical spine which do not explain this presentation. 06:54 And essentially, the MRIs of the C spine is unremarkable for an etiology of this disorder. 07:01 The patient underwent MRI of the brain to look for any central nervous system pathology that could be contributing. 07:06 And as this as expected, the MRI of the brain was unremarkable and again did not show any explanation for this patients combined upper and lower motor neuron disorder. 07:16 There was also an extensive laboratory investigation that was undergone. 07:20 CK was normal at 53 though sometimes can be mildly elevated in this condition. 07:25 ESR and CRP were performed to look for any systemic inflammatory processes that could be contributing to a secondary CNS inflammatory disorder which were norma ANA was negative, Thyroid Stimulating Hormone - negative, Serum protein electrophoresis was without an M spike, there was no paraproteinemia, free light chains were within normal limits and RPR was negative. 07:49 In addition, the patient underwent B12 testing. 07:51 B12 can present as a myeloneuropathy central nervous system or spinal cord pathology and peripheral neuropathy. 07:58 So combined upper and lower motor neuron symptoms but was normal at 533 (pg/mL). 08:03 Copper level was also performed and within normal limits and both B 12 deficiency and copper deficiency can present as a myeloneuropathy. 08:11 Lyme disease testing was negative, Vitamin E was within normal limits and that can present with again a myeloneuropathy with ataxia, which was a consideration in this case in this patient but was normal, and then HIV testing was negative. 08:25 So the patient underwent EMG nerve conduction study to further evaluate the potential cause for this condition and it was consistent with motor neuron disease. 08:35 The left median motor and ulnar motor responses revealed low amplitude so something's going on to reduce the number of nerves, the number of peripheral nerves to the left median and ulnar nerves. 08:47 All sensory studies were intact with normal values, and that's really important. 08:51 There's no diagnostic test for motor neuron disease. 08:54 It's a diagnosis of exclusion, and excluding the presence of sensory abnormalities is critical. 09:00 Motor neuron diseases, disease of the motor neurons, not the sensory neurons and we see that here. 09:06 And needle EMG showed abnormal spontaneous activity with obvious neurogenic pattern with activation on all four extremities that we're seeing denervation changes, loss of innervation of the muscles as a result of some motor neuron pathology on needle EMG exam. 09:24 And so ultimately, this patient's presentation was consistent with a diagnosis of motor neuron disease, or ALS, amyotrophic lateral sclerosis. 09:32 And so let's walk through some of the key features of motor neuron disease, how we define it, localize it, evaluate and treat this disorder. 09:41 First, let's talk about how we define motor neuron disease, both the upper and lower motor neurons.
About the Lecture
The lecture Case: 56-year-old Woman with Left Extremity Weakness by Roy Strowd, MD is from the course Diseases of the Motor Neurons.
Included Quiz Questions
Which of these would be an expected finding in a patient with a pure motor neuron disorder?
- Nerve conduction sensory responses with normal latency and amplitude
- A lesion in the occipital region of the cerebrum on MRI
- A C6 disk protrusion affecting the dorsal root ganglia
- High serum vitamin B12 levels
- Nerve conduction motor responses with increased amplitude
Which symptom is most consistent with lower motor neuron findings?
- Fasciculations
- Hyperreflexia
- Bradykinesia
- Postural instability
- Allodynia
Hyperreflexia is most common in which of the following?
- Upper motor neuron pathology
- Lower motor neuron pathology
- Polyneuropathies
- Guillain-Barré syndrome
- Hypothyroidism
A patient with a lower motor neuron disorder is most likely to present with which of the following?
- Focal muscular atrophy
- Paresthesias
- Bilateral foot numbness
- Hyperalgesia
- Muscular fatigue that improves with use
Which finding may be seen in a patient with a suspected pure motor neuron disorder?
- Normal serum laboratories
- Cortical atrophy on MRI
- Cervical disc protrusions
- M-spike on SPEP
- Sensory abnormalities
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |