Playlist
Show Playlist
Hide Playlist
Osteoporosis: Diagnosis and Management
-
Slides Osteoporosis Chronic Care.pdf
-
Download Lecture Overview
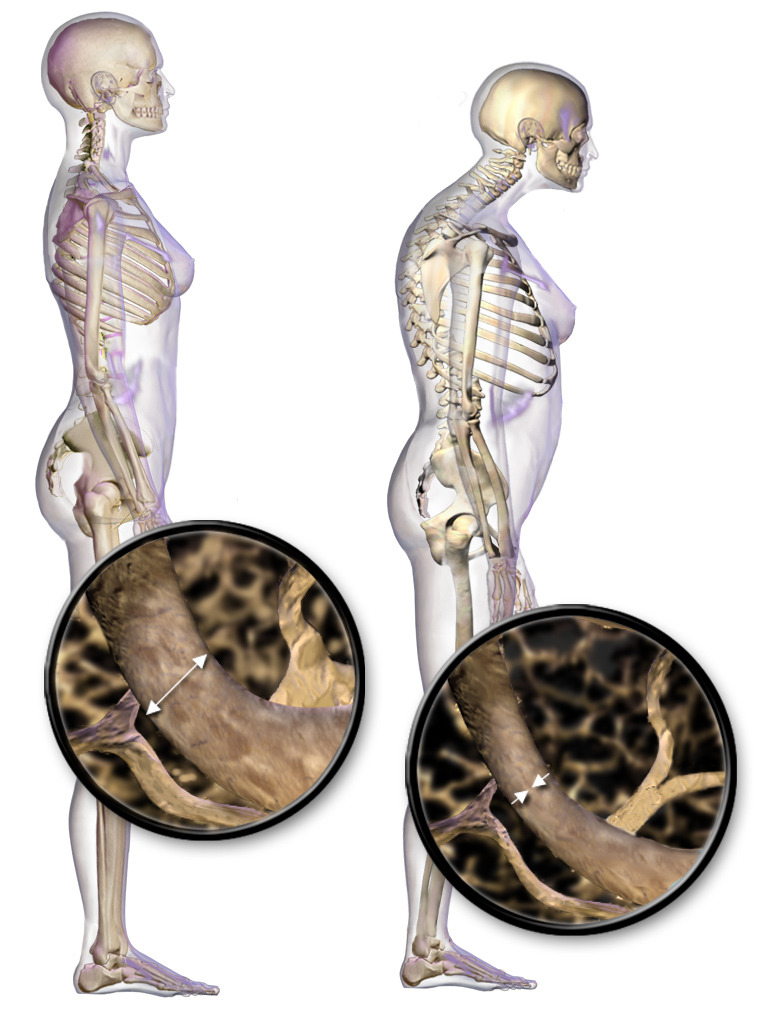
00:01 Now, let's talk about osteoporosis. 00:03 And to me, this is often a forgotten diagnosis, particularly among our older patients. 00:09 But I bet that if you had a grandmother or your mother who suffered a fracture of her spine or of her hip, you’re not going to forget about it. 00:19 It is a serious diagnosis that carries potentially devastating consequences for patients and, therefore, it's worth a minute to talk about it. 00:26 So, let's go. 00:27 We’re going to be discussing the risk of fracture overall, how to screen for it. 00:33 And I thought we’d start with a case. 00:35 This is a 66-year-old white woman presenting for a wellness visit. 00:39 She has no past medical history and no complaints. 00:41 That's a rare event. 00:43 She has no family history of osteoporosis or fracture in particular. 00:49 Now, what should you offer her to screen for her risk of fracture. 00:54 A, nothing, she has no risk factors; or B, nothing, only African-American women should be screened for osteoporosis; C, screening with an ultrasound of the calcaneus; or D, screening with DEXA of the hip and spine. 01:07 DEXA is dual absorption x-ray absorptiometry. 01:14 The answer is D, DEXA. 01:15 So, DEXA scanning is the preferred method for screening for osteoporosis. 01:21 She is over 65 and, therefore, meets screening recommendations for screening - for a screening exam. 01:29 The reason we think about screening patients is that osteoporosis is very common, affects more than 10 million Americans. 01:37 Overall, here's a graph that shows the lifetime risk of osteoporotic fracture among white adults in particular and we’ll talk about some of the racial differences associated with osteoporosis. 01:48 You can see it’s much higher for women among men. 01:50 That's why women are recommended for screening, but men are not. 01:54 So, what are some of the risk factors for osteoporosis? Obviously, age. As we get older, our bones become higher risk for fracture. 02:03 White or Asian race, so those are the two racial groups that are associated with greater rates of osteoporosis and fracture. 02:11 History of smoking, family history of osteoporosis or fracture, having a low body weight - not a high bodyweight, but a low one - and the biggest risk factor for an osteoporotic fracture in particular is a previous osteoporotic fracture. 02:26 So, it's amazing to me that patients come in and they already have a history of compression fracture of the spine or a fracture of the hip and/or some other fragility-based fracture, and yet they haven't been tested with a DEXA nor are they on treatment. 02:41 Really, once you have an osteoporotic fracture, it's a good idea to just initiate bisphosphonate treatment and then do a DEXA scan as - just to get a baseline level of where the patient is. 02:53 But that is a tremendous risk factor for another fracture, is a previous fracture. 03:00 So, as I mentioned, the Dual Energy X-Ray Absorptiometry study is preferred and that starts at age 65 for average risk patients. 03:08 For higher risk patients, those who have a family history of osteoporosis and fracture, those have been on corticosteroids for a long time, there are some tools that can help to judge when the patient should be screened and if they deserve early screening for fracture risk. 03:27 Men, there's really not a clear benefit to screening for men, even those at higher risk. 03:33 So, therefore, there is no strong recommendation to screen broadly for osteoporosis among men. 03:40 And then, it is important for clinical practice as well as your exam, osteoporosis defined by that T score of at least 2.5 standard deviations below the mean. 03:49 The T score is the comparison to the period in life in the early 20s when you have your greatest bone mass. 03:57 So, what did her DEXA test show? She has a T score minus of 2.7. 04:03 So, now, which of the following routine laboratory tests is indicated for this patient based on that DEXA score alone? Is it HIV, TSH, parathyroid hormone (or PTH), or a complete blood count (CBC). 04:17 TSH. 04:18 This patient, because her score is minus 2.7, it's less than minus 2.5, therefore, she fits the criteria for osteoporosis. 04:29 All patients with osteoporosis should be checked with a TSH and they should also get a calcium level and routine electrolytes. 04:36 Now, what's the best treatment option for this patient? Yet another question. 04:40 How about calcium only, calcium with vitamin D, a bisphosphonate or calcitonin? Bisphosphonate. 04:48 If you really want to prevent fracture in this patient, which is the ultimate goal, we’re not looking to necessarily increase bone density. 04:55 We want to maintain bone density, but that's not even - that's not an outcome the patient can feel, right? That's something that we can measure. 05:04 But what we really want to prevent is fracture. 05:07 That's an important patient-oriented outcome. 05:10 And bisphosphonates have the strongest track record for preventing fracture. 05:15 And they’re more effective overall for preventing spinal versus hip fracture. 05:20 Number needed to treat is fairly low at 25, but it can range up to 95 for some studies looking at hip fracture. 05:27 But, again, preventing a spine or hip fracture can be absolutely critical. 05:33 It can prevent the patient from suffering complications due to immobility, being placed in a nursing home. 05:39 So, there’s a lot of benefits to preventing these fractures that go beyond just the fracture itself. 05:44 However, current recommendations state that after about five years of treatment among - in a low risk woman, it may be okay to consider stopping treatment with bisphosphonates. 05:57 Second line agents for patients who can't take or can't tolerate bisphosphonates say they have a history of severe esophagitis. 06:03 I have a patient in that situation. 06:05 And therefore, bisphosphonates aren’t a great option for her because of their associated risk of esophageal disease. 06:13 Raloxifene can be a good second line agent. 06:16 It's a selective estrogen receptor modulator. 06:21 Side effects can include vasomotor symptoms. 06:23 So, particularly for patients with more severe menopausal symptoms, it’s not a great option. 06:28 And there is some small increased risk of venous thromboembolism. 06:34 Whereas other drugs, newer drugs for the application against osteoporosis are really only used for severe cases that don't respond to normal therapy, that's teriparatide or denosumab and those are given in an endocrinology office. 06:51 Now, calcium and vitamin D do have a role. 06:56 And, of course, patients with osteoporosis should continue on calcium and vitamin D. 07:00 But using them alone among patients with osteoporosis is insufficient in terms of preventing fracture, and so they need to be augmented with one of these other agents. 07:09 Again, bisphosphonates preferable. 07:12 So, that's really what I wanted to discuss with bisphosphonates. 07:16 Who should be screened, some of the risk factors, and then particularly the treatment is really important. 07:22 So, when you identify it, even if it's just a patient who has a previous osteoporotic fracture, initiate treatment with a bisphosphonate with good warnings about taking in the morning before eating a meal and making sure that they’re upright to prevent those esophageal complications. 07:38 They should do great and prevent fracture down the road. 07:42 Thanks.
About the Lecture
The lecture Osteoporosis: Diagnosis and Management by Charles Vega, MD is from the course Chronic Care. It contains the following chapters:
- Osteoporosis
- Screening for Osteoporosis
- DEXA Testing
Included Quiz Questions
Which of the following is NOT a risk factor for osteoporotic fracture?
- Obesity
- Chronic glucocorticoid use
- Excess alcohol intake
- History of smoking
- Advancing age
Which of the following is the most widely used method for measuring bone marrow density?
- Dual-energy x-ray absorptiometry
- Quantitative computed tomography
- Serum calcium and vitamin D levels
- Quantitative heel ultrasound
- Spine X-ray
What is a contraindication to bisphosphonate treatment?
- History of Barrett's esophagus
- History of smoking
- History of chronic corticosteroid use
- History of hip fracture
- Family history of breast cancer
Which of the following statements about Raloxifene treatment is NOT true?
- It is a first line treatment for osteoporosis.
- It increases the risk of venous thromboembolism.
- It reduces the risk of breast cancer.
- It is a selective estrogen receptor modulator.
- It may cause hot flushes.
Which of the following patients should be started on bisphosphonate treatment?
- A woman with a T-score of -2.7
- A woman with a T-score of 2.7
- A woman with a T-score of -1.5
- A woman with a T-score of 1.5
- None of the options are an indication for therapy with bisphosphonates.
Customer reviews
4,5 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
The lecturer is very eloquent and pleasant. He also points to facts which may be confusing and harder to memorize, making it easier in remembering. He gives great examples to stress the importance of the information in his lectures.
This lecture is concise, patient-oriented, and well-sequenced with appropriate graphics.