Playlist
Show Playlist
Hide Playlist
Gastroesophageal Reflux Disease (GERD): Diagnosis & Management
-
Slides Structural GI Diseases.pdf
-
Download Lecture Overview
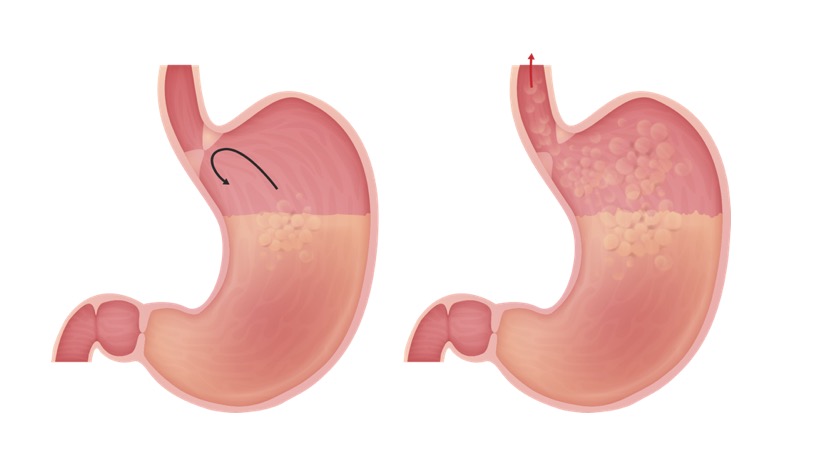
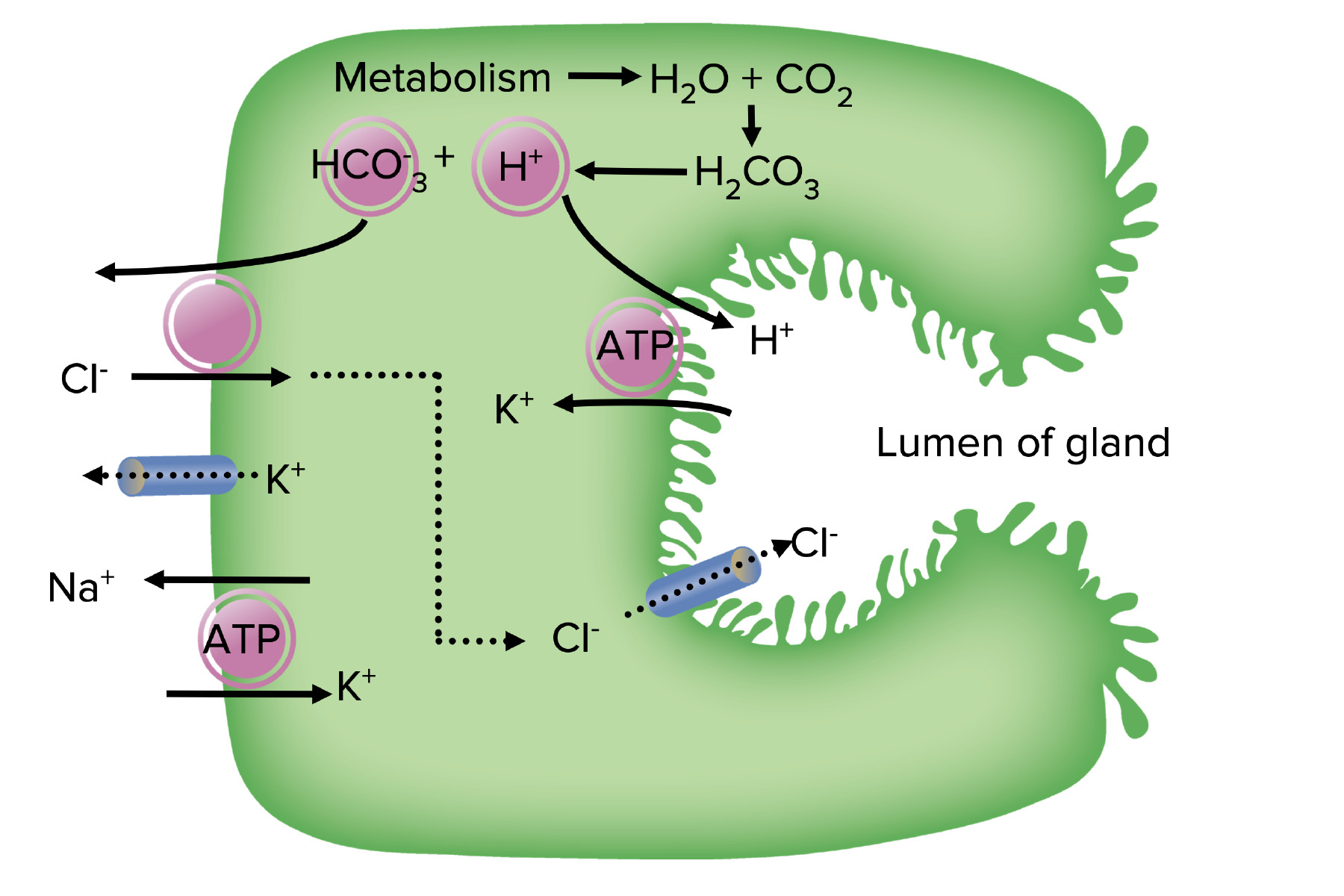
00:02 Imaging for reflux is almost always a bad idea, and the reason I say that is because it’s almost always present. 00:09 Remember, 60% of totally normal newborns regurgitate at least once a day. 00:16 When we do a swallow study, which is what you can see on this slide, we make children NPO for a period of time and then send them to the radiology suite. 00:25 They greedily eat down their contrast because they’re very hungry, and then a lot of the time, reflux is seen. 00:32 That doesn’t mean the child has reflux disease. 00:37 The false positive rate is high because reflux is physiologic. 00:41 So, diagnosis of this condition is actually somewhat clinical. 00:46 If we suspect reflux disease, we don’t often test for it but rather we’ll treat it empirically and see how the child responds. 00:55 Imaging is really only for suspected swallowing problems in children with neurologic deficit, for example, where we suspect a problem, or in children where there might be something structurally preventing the esophagus from working such as a vascular ring. 01:13 Upper GI series will rule out anatomical abnormalities, but again, there’s a very high false positive rate for reflux. 01:22 We could do nuclear scintigraphy. 01:24 This is a radio-labeled food, and then we see whether it goes to the stomach or the lungs. 01:30 This is useful really for things like delayed gastric emptying. 01:34 We don’t use this test very often. 01:38 So, the test of choice, if you must do one, is the esophageal impedance probe. 01:43 What this does is it’s a tube, as in this child, where it goes into the nose and down into the esophagus. 01:50 There are lots of little measuring devices that are looking for measuring electrical impedance between these little measuring things all the way down the probe. 02:02 So, when the patient refluxes and electrical conducting fluid now goes over these, you can tell exactly what level that fluid has gone to, and therefore determine the distance that the esophagus is having reflux climb up it. 02:19 This has replaced the pH probe, which could only detect acid. 02:23 This detects all types of fluid. 02:26 So, for infants who were already being treated with omeprazole, for example, you will still detect an abnormal impedance probe but you would not necessarily have an abnormal pH probe. 02:41 This correlates non-specific symptoms with GER events. 02:46 So for example, if a child has apnea, stridor, and irritability while the pH probe was going up, that implies that there’s a connection here. 02:55 So the mother or the parent can have a button to press while the child is sitting there on this study and they can correlate the button with the event of reflux and see if there’s a correlation, and that can help them determine if the reflux is the problem or if that’s just what the parent is concerned about, and this baby is actually doing normally. 03:19 To truly diagnose it, we can also do endoscopy and biopsy, which is a reliable diagnostic method but is invasive. 03:26 We have to put the child to sleep, put a camera down there and look for erosions. 03:31 It’s usually unnecessary, unless there’s a suspicion for another problem and then we happen to find an evidence of reflux. 03:40 So there are some nonsurgical therapies that we can do for reflux. 03:45 First off, we can educate about feeding large volumes. 03:49 If infants eat smaller volumes more frequently, they’re less likely to reflux. 03:54 Large volumes are likely to fill up the stomach and are more likely to reflux. 03:59 Positioning upright after feeds may well be on your exam but actually has been shown not to be effective. 04:08 Positioning after feeds really is of no benefit, and in fact, some people recommend sitting in a car-seat after feeds, but that’s actually been shown to increase aspiration risk. 04:19 So that is not warranted. 04:22 If we decide to treat in a medical fashion, there are two ways we can go about it. 04:28 One is to suppress acid production in the stomach, and this will reduce pain and fussiness with refluxing events. 04:39 However, it does not prevent the reflux itself. 04:42 It’s not acting as a barrier, it’s just reducing the amount of acid. 04:47 And the problem is it turns out that refluxing is good for you. 04:52 Yeah, I said that. 04:53 Refluxing is good for you. 04:55 In infants and in adults, the refluxing of acid up into the upper area of the throat causes a reduction in the amount of bacteria that are there and reduces the risk of pneumonia. 05:10 Children and adults on acid suppression therapy have an approximately six-fold increase risk for pneumonia. 05:18 They also are at risk for gastroenteritis. 05:21 And in adults, C. diff enteritis. 05:24 So, it’s not totally benign to start acid suppression. 05:28 An alternative in infants is to thicken their feeds. 05:32 Viscous feeds are less likely to reflux simply because it’s harder to get them back up the tube. 05:38 This is more effective than acid suppression in most cases. 05:43 It does actually prevent the refluxate. 05:47 However, it can cause obesity. 05:51 So, infants were fed thickened feeds will gain weight much faster because the thickener is caloric addition. 05:59 And as we have learned, rapid weight gain in the first year of life puts children at risk quite remarkably for adult type 2 diabetes much later in life. 06:11 So it is not a benign thing to cause a baby to gain rapid weight during their first year of life. 06:18 There is a surgical alternative that is in existence for children with severe reflux, and often, this is limited to children who are either getting a G tube because they’re incapable of eating, and especially we see this done in children with severe cerebral palsy or other neurologic problems. 06:36 This is called the Nissen fundoplication, and basically, it’s a surgical wrap of the gastric antrum around the distal esophagus. 06:45 This is reserved for chronic gastroesophageal reflux disease, which is not responsive to other therapies. 06:54 The problem is that when we finally studied in the one largest and best study we did, it turns out that children who had this procedure done did not actually have improved outcomes in terms of recurrent hospitalizations for reflux-like events. 07:11 So, it’s not totally clear that this operation, while it’s commonly done, is particularly effective. 07:18 But sometimes, there’s not much else you can do. 07:23 That’s all I have for you today about gastroesophageal reflux disease and the other problems that are structural involving the enteric system. 07:31 Thanks very much.
About the Lecture
The lecture Gastroesophageal Reflux Disease (GERD): Diagnosis & Management by Brian Alverson, MD is from the course Pediatric Gastroenterology. It contains the following chapters:
- GERD: Diagnosis
- GERD: Management
Included Quiz Questions
How is gastroesophageal reflux disease generally diagnosed in infants?
- History and physical examination
- Esophageal pH probe
- Esophageal manometry
- Esophageal impedance probe
- Upper GI series
Thickened feeds for a child with GERD is appropriate, but it can lead to which of the following complications when used long-term?
- Obesity
- Chronic diarrhea
- Gastroenteritis
- Pneumonia
- There are no long-term complications
Approximately what percent of normal infants have symptoms of gastroesophageal reflux around 4 months of age?
- 60%
- 20%
- 2%
- 5%
- 25%
Which of the following findings on esophagogastroscopy is characteristic of GERD?
- Erosion
- Excessive mucus
- Pigmented ulcer
- White patch
- Polyp
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |