Playlist
Show Playlist
Hide Playlist
Stroke Imaging Findings
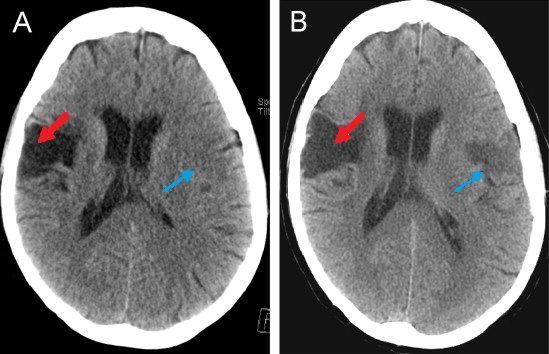
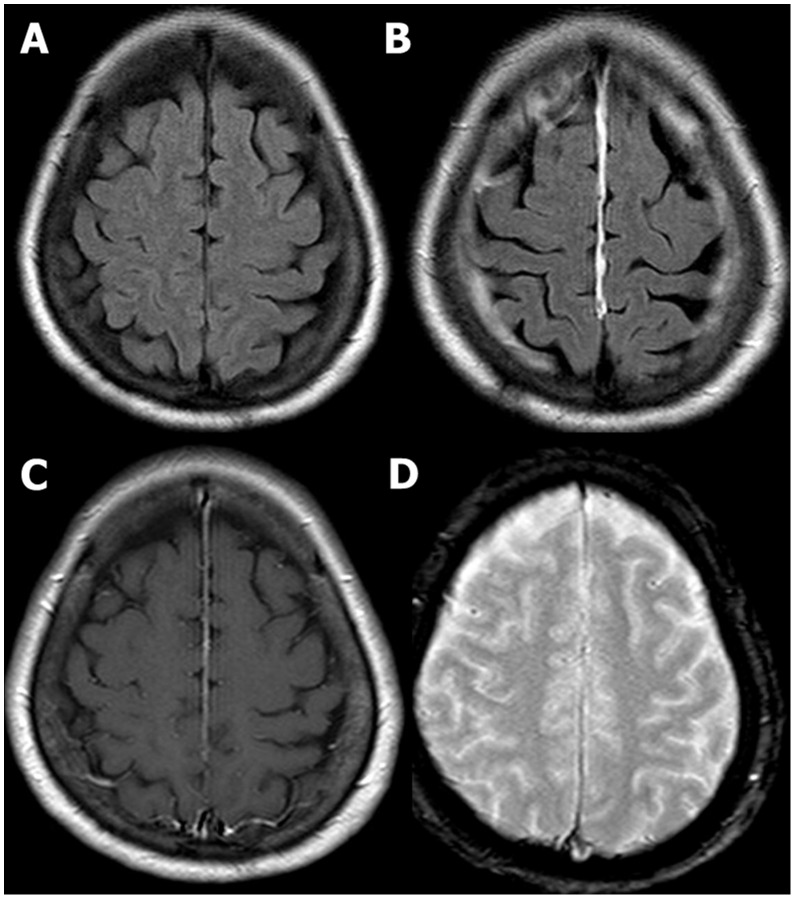
00:01 So one of the most important things that we can look for on brain imaging are the findings of an acute stroke. 00:06 Let's start off by taking a look at this case. 00:09 Take a look at the findings and keep this in mind as we go through the lecture and then we'll go back to this at the end. 00:16 Stroke is the compromise of the blood supply to a portion of the brain parenchyma which results in loss of neurologic function. 00:24 Strokes may be caused by an embolic or a thrombotic event and diagnosis is often based on clinical symptoms. 00:31 In the setting of an acute ischemic stroke, t-PA or Tissue Plasminogen Activator can provide the most benefit if it's administered within 3 hours of the onset of stroke. 00:41 There's only a moderate benefit if it's administered between 3 and 4 ' hours of the onset of stroke. Anything after that, then t-PA is not very useful. 00:50 So what is the role of imaging when it comes to acute stroke? It's really to exclude hemorrhage because t-PA is contraindicated in a patient that has hemorrhage. You also want to exclude other causes of symptoms such as mass. 01:02 There are 2 major types of stroke. 01:06 There's an ischemic stroke and then there's a hemorrhagic stroke. 01:09 The area of the brain parenchyma at the junction of the two vascular territories is called the watershed territory and that is actually the most susceptible to ischemia. 01:19 Common watershed areas are between the ACA and the MCA and also between the MCA and the PCA. 01:26 So you wanna begin with the CT scan of the head because of its quick access and the ability to exclude hemorrhage. 01:32 Ischemic strokes, however, may not be visible on CT for several hours. 01:36 MRI's actually the most sensitive examination for early ischemic stroke and diffusion weighted images are the ones that are the most useful. 01:45 They demonstrate changes of an acute stroke within 20 to 30 minutes of onset. 01:49 However, MRI can be hard to obtain and can be time consuming. 01:52 You don't wanna waste those precious few minutes looking for an MRI and with this is why stroke imaging is usually held off only for patients looking for secondary signs of stroke. 02:03 So within 24 hours, CT Findings can actually be negative. 02:08 Early findings can include decreased density in the basal ganglia, loss of gray-white differentiation, or what's called the hyperdense MCA sign. 02:17 So the MCA, are the middle cerebral artery, can appear dense because of thrombosis within it. 02:22 Within 12 to 24 hours, you may see a vague low density area within the brain parenchyma and after 24 hours you have a better defined low density area. 02:31 You also have loss of gray-white differentiation and you could have adjacent edema and mass effect. 02:37 These changes can last for up to 4 weeks after the initial event. 02:42 So let's take a look at these findings. 02:44 On the left, we have a CT scan of the head. 02:47 And on the right, we have a diffusion weighted image on MRI. 02:50 Let's take a closer look at the CT scan. 03:01 So the CT image on the left is actually negative. 03:05 The patient presented with symptoms for about 2 hours, however, you can see that on the diffusion weighted image or the DWI image there's a bright area in the right frontoparietal region and this indicates acute stroke. 03:17 So let's take a look at these images and we wanna see how stroke can evolve over time. 03:22 This image depicts the findings of a stroke at about 24 hours, so there is loss of gray-white differentiation and there's compression of the ventricles and shift of the midline or subfalcine herniation. 03:33 So here we have the findings of the hypodensity, we no longer have gray-white differentiation here and if you take a look at the midline it's shifted to the right so this is subfalcine herniation. 03:44 This image was performed several weeks after the initial event. 03:49 So you can see now that the low density area is more sharply marginated and there is no longer any mass effect. 03:55 So the midline is now back to midline and you can see that the ventricle is actually enlarged and this is called ex-vacuo dilatation of the ventricle. 04:05 Because you have loss of blood brain parenchyma here, the ventricle on that side fills that space and dilates. 04:11 So hemorrhagic strokes can occur into the brain parenchyma or into the subarachnoid space. 04:17 If a patient has hypertension, this significantly increases the risk of hemorrhagic conversion of a stroke. 04:22 So let's take a look at this case. 04:25 This is a 65-year-old male that presents with right sided weakness which began about 2 hours ago. 04:30 The patient had a CT scan of the head, so let's take a look at the scan. 04:35 Do you see any findings here? So the CT is actually normal. 04:48 How would you treat this patient? So if you remember, stroke is a clinical diagnosis. 04:54 The CT scan is done to see if there are any other signs that could be causing these symptoms and to see if there is any hemorrhage. 05:01 So as hemorrhage is excluded, the patient was clinically diagnosed with an ischemic stroke and was treated with t-PA and admitted to the ICU. 05:08 However, he lost consciousness the next day. 05:12 So what would be your next step? So this patient ended up having a CT scan. 05:24 If you recall, this is the image that we saw at the beginning of the lecture. 05:28 So let's take a look at these 2 non-contrast axial CT scan through the head. 05:33 What are the different findings that you see here? So this CT demonstrates intracerebral, subarachnoid, and subdural hemorrhage. 05:49 So let's take a look, here's an example of an intracerebral hemorrhage. 05:53 The patient also has subarachnoid blood which we can see here, here, and then on this scan we can see some subarachnoid blood here as well. 06:02 There's a subdural hematoma along the left convexity here, as well as here. 06:08 This patient also has shift of the midline structures to the right indicating that there is subfalcine herniation. 06:17 So the stroke has now become hemorrhagic, so what would be your next step? So in this case you would wanna call neurosurgery for urgent surgical decompression to relieve mass effect. As you recall, subfalcine herniation can lead to death so this increase intracranial pressure needs to be relieved quickly. 06:35 So in this lecture we've covered some of the findings of acute stoke, ischemic, and hemorrhagic and as you recall MRI is really the most sensitive way to evaluate for stroke, however, because you have a limited amount of time in which you need to treat the patient, a clinical diagnosis is really the way to go with the CT performed just to make sure that there's no hemorrhage before you treat the patient.
About the Lecture
The lecture Stroke Imaging Findings by Hetal Verma, MD is from the course Neuroradiology.
Included Quiz Questions
A patient presents with stroke symptoms and acute onset slurred speech that started 2 hours ago. What is the imaging study of choice and why?
- Non-contrast head CT to exclude hemorrhage before administration of tPA.
- Brain MRI because it is more sensitive to evaluate for acute stroke.
- Head CT with contrast for better evaluation of the vasculature.
- Non-contrast head CT because it is most sensitive to evaluate for acute stroke.
- Brain MRI to assess for mass lesions.
Which statement is FALSE regarding stroke and its management?
- The administration of tPA has the most benefit when administered within the first 12 hours of onset.
- Stroke is ischemia and infarct of a portion of the brain parenchyma.
- Stroke may be thrombotic or embolic.
- Ischemic strokes may not be visible on CT images for several hours after the onset.
- The watershed territory is most susceptible to ischemia.
What is the “hyperdense MCA” sign seen on CT imaging after a middle cerebral artery stroke?
- The MCA can appear dense due to thrombosis within it.
- It is not seen until after 24 hours post-stroke.
- It is an enlarged left ventricle.
- It is a vague low-density area.
- It is a loss of gray/white differentiation.
Which of the following situations require urgent surgical intervention?
- Subfalcine herniation after a hemorrhagic stroke
- Glioma in the left occipital lobe
- Pituitary adenoma reaching up to the optic chiasm with no visual defects
- Normal-pressure hydrocephalus in a 78-year-old patient
- An ischemic stroke in a 54-year-old hypertensive patient
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |