Playlist
Show Playlist
Hide Playlist
Hypercalcemia: Types & Causes
-
Slides Hypercalcemia.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
00:02
Hypercalcemia, we talked about the different
types.
00:04
If there’s primary hypoparathyroidism, which
is a malignancy of your parathyroid glands,
and on your boards and on your wards, you
usually will not have other issues per se
and what I mean by that is the kidney function
should be relatively normal.
00:24
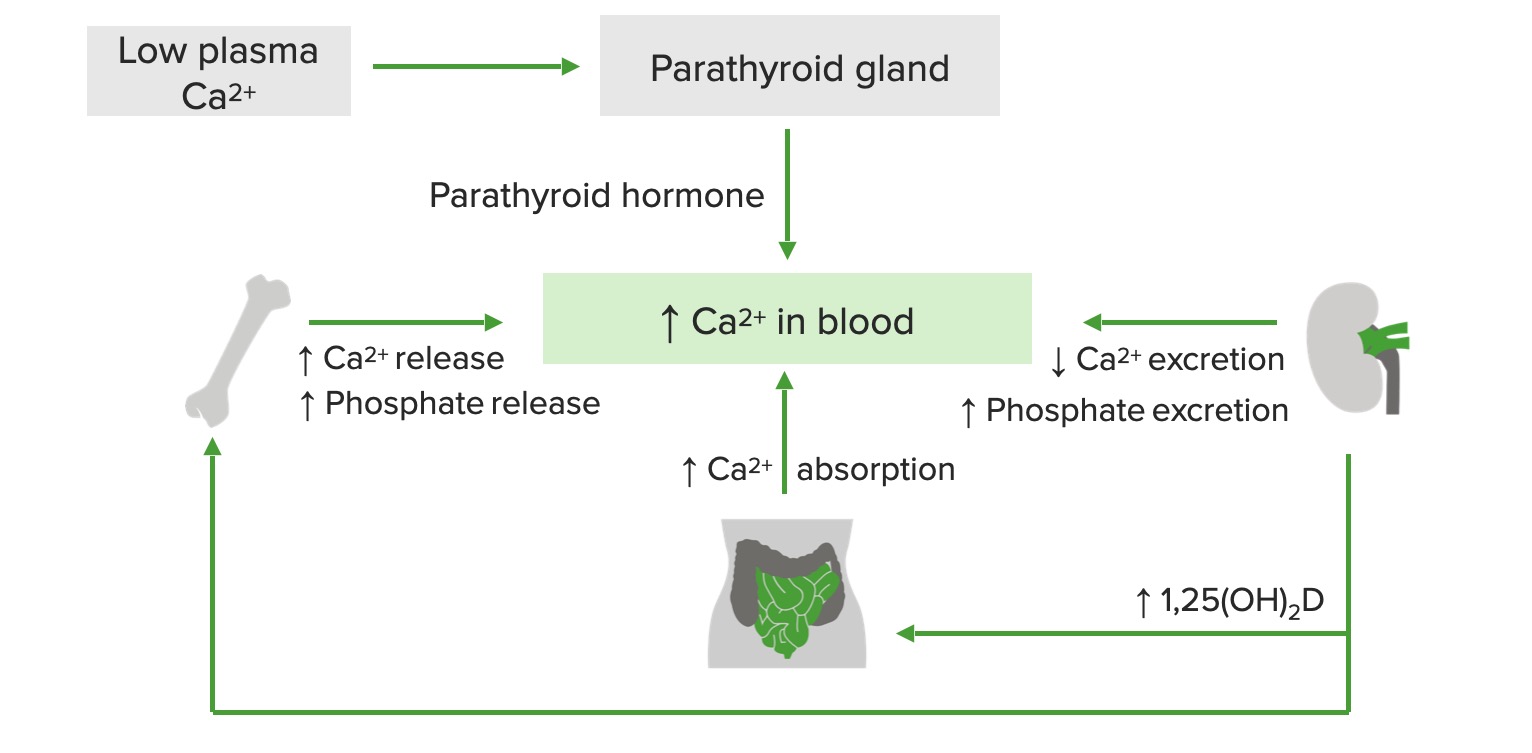
With that primary hypoparathyroidism, which
could be part of MEN type-1, could be part
of 2a, right, MEN, multiple endocrine neoplasia,
you are then going to result in hypercalcemia
because PTH will resorb your calcium from
the kidney and resorb the calcium from the
bone.
00:43
The mechanisms of malignancy-related hypercalcemia…
bone metastases, resorption; breast, multiple
myeloma, prostate, lymphoma, thyroid, lung,
so on and so forth.
00:52
So, metastases from different organs, meaning
to say primary cancer existed in breast, metastasized
to the bone resulting in resorption of it
resulting in hypercalcemia.
01:03
Multiple myeloma, you’ve-you’ve heard
of that punched-out lytic lesions in the bone.
01:09
Prostate cancer, it might then spread from
the prostate out then through the batson-batson
paravertebral plexus into the vertebrae therefore
bring about hypercalcemia, lymphoma thyroid.
01:23
Humoral hypercalcemia, PTH-related peptide
and what that basically means is that you
have paraneoplastic.
01:31
Two major paraneoplastic conditions that you
want to know of where you may then release
PTH-related peptide, number one, will be squamous
cell cancer of the lung and the other big
one will be renal cell carcinoma.
01:43
Do not forget these two for sure.
01:46
Because of all that PTH-rp then working upon
your PTH receptor, you are then going to reabsorb
your calcium resulting in hypercalcemia in
with your actual PTH level.
01:55
“Dr. Raj, aren’t they the same thing?”
No, the PTH-related peptide is different from
PTH.
02:02
The PTH is being released from your parathyroid
glands and when you have all this hypercalcemia,
your parathyroid glands will be shut down.
02:11
Clear?
So, your actual PTH levels are decreased,
but PTH-rp is increased.
02:18
Same concept as Graves’ disease where you
have thyroid stimulating immunoglobulin binding
to the TSH receptor.
02:26
All that T3,T4 is going to shut down your
anterior pituitary from releasing TSH.
02:30
What’s your TSH level in Graves’?
Dramatically decreased.
02:36
What’s your PTH level in this patient?
Dramatically decreased.
02:40
Please do some parallels.
02:43
Conversion of 25 type of Vitamin D to 1,25
example such as lymphoma.
02:50
Others, well, if you’re thinking about hypovitamin
D-osis, we’re thinking about sarcoidosis.
02:57
These are all the different causes of hypercalcemia,
the first one being primary hyperparathyroidism
where the 90 percent of hypercalcemia being
caused by a type of adenoma.
03:09
Make sure that you know about malignancy-related
hypercalcaemia as well, this is a very good
[Inaudible 00:03:14] list that you want to
be extremely familiar with.
03:20
As mentioned before, sarcoidosis which then
increases your activity of 1,25 dihydroxycholecalciferol
or calcitriol; hypervitaminosis D may result
in hypercalcemia.
03:31
In pulmonology, we talked about proper management
of sarcoidosis; may respond to glucocorticoid…
hypercalcemia.
03:41
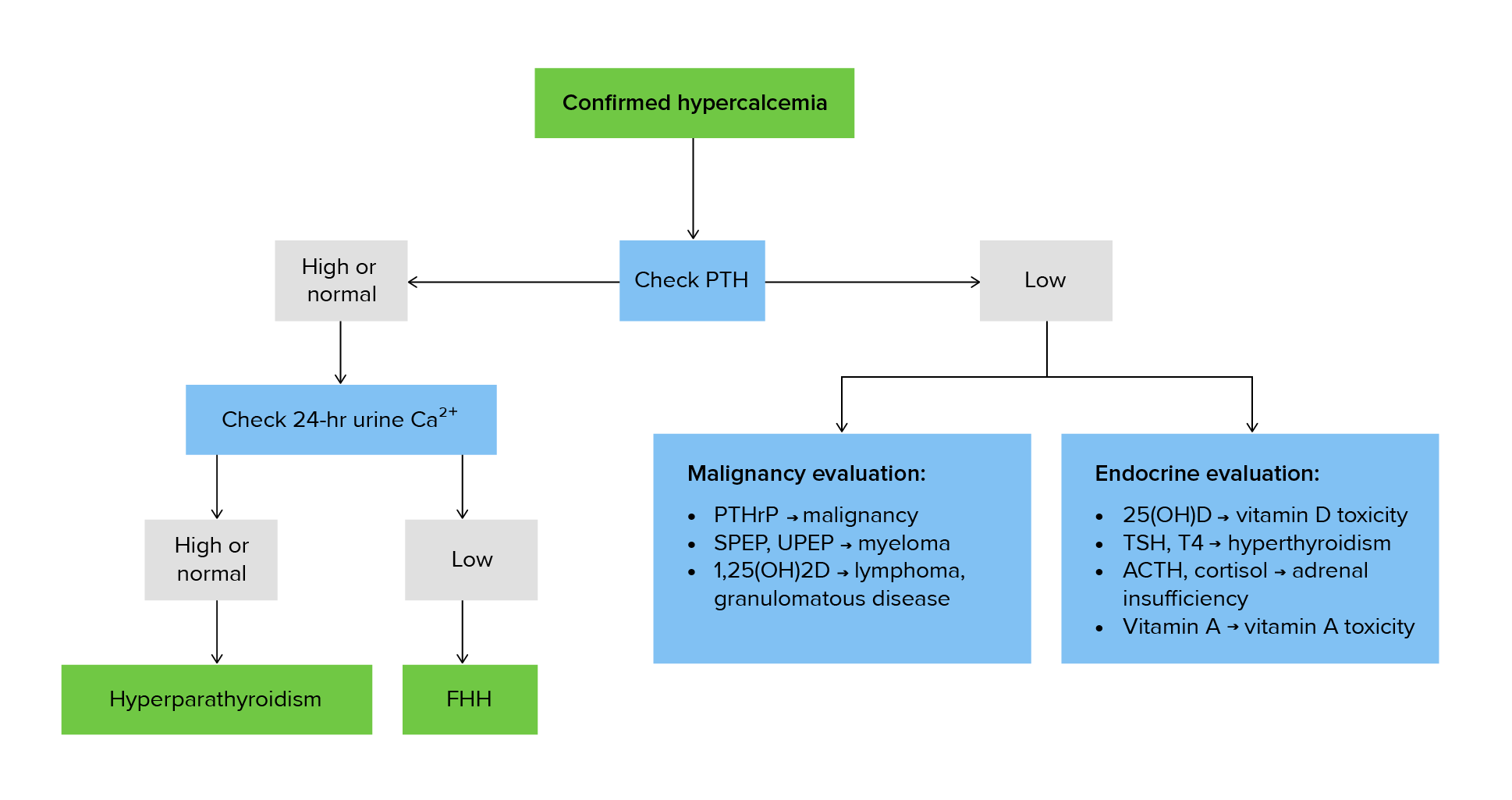
Continue discussion of hypercalcaemias, take
a look at familiar cause.
03:45
Another cause at the bottom of this section
will be drugs, keep them separate.
03:49
But, the familiar cause here is hypocalciuric
hypercalcemia… allow the name to speak to
you.
03:56
There is something going on in the kidney
in which the receptors for PTH are responding
extremely well, too well to the point where
there is increased reabsorption of calcium
from the urine, hypocalciuric, and putting
it into where?
Emia… welcome to familial hypocalciuric
hypercalcemia.
04:17
With this, look for family history, not necessarily
required, but nonetheless, the question might
have family history of par-parathyroidectomy.
04:30
Benign clinical manifestation, however, and
then drugs such as thiazide diuretics.
04:36
Because of increased reabsorption of calcium
from the DCT may result rare, just keep this
in mind, maybe hypercalcemia.
04:46
Vitamin D intoxication, hypercalcemia; immobilization,
especially in Paget’s disease patients.
04:52
Remember Paget’s disease of the bone, obviously
is what our… what we… what I am referring
to.
04:59
And with Paget’s disease of the bone, it
takes a triphasic type of pathogenesis.
05:06
So, you begin with that osteolytic phase and
then you end up with the mosaic pattern.
05:13
The osteoclast will completely burn out, in
which you then go into osteosclerotic phase.
05:18
Do you remember?
Paget’s disease of the bone.
05:21
Others, thyrotoxicosis, adrenal insufficiency,
pheochromocytoma and parenteral nutrition
may all result in hypercalcemia.
About the Lecture
The lecture Hypercalcemia: Types & Causes by Carlo Raj, MD is from the course Parathyroid Gland Disorders.
Included Quiz Questions
A patient presents with hypercalcemia and low PTH. There are no other symptoms that point to an electrolyte disorder, but the patient does complain of cough and pleuritic chest pain. Which diagnosis ranks high on your differential?
- Squamous cell lung cancer
- Myocardial infarction
- Pneumonia
- Small cell lung cancer
- Congestive heart failure
Which substance is increased in sarcoidosis and causes hypercalcemia?
- Vitamin D
- Calcium
- Phosphate
- PTH
- Potassium
What is the adequate management of hypercalcemia caused by a granulomatous disease?
- Glucocorticoids
- Medications that decrease the absorption of Vitamin D in the gut
- Radiation therapy
- Antibiotics (penicillins or cephalosporins)
- Lifestyle changes
What is NOT a characteristic of familial hypocalciuric hypercalcemia (FHH)?
- Low PTH
- Autosomal dominant inheritance pattern
- Low urinary calcium
- Family history of parathyroidectomy
- Mutations in calcium-sensing receptors
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |