Playlist
Show Playlist
Hide Playlist
Vaginitis in Adolescent Girls
-
Slides Vaginitis Pediatrics.pdf
-
Download Lecture Overview
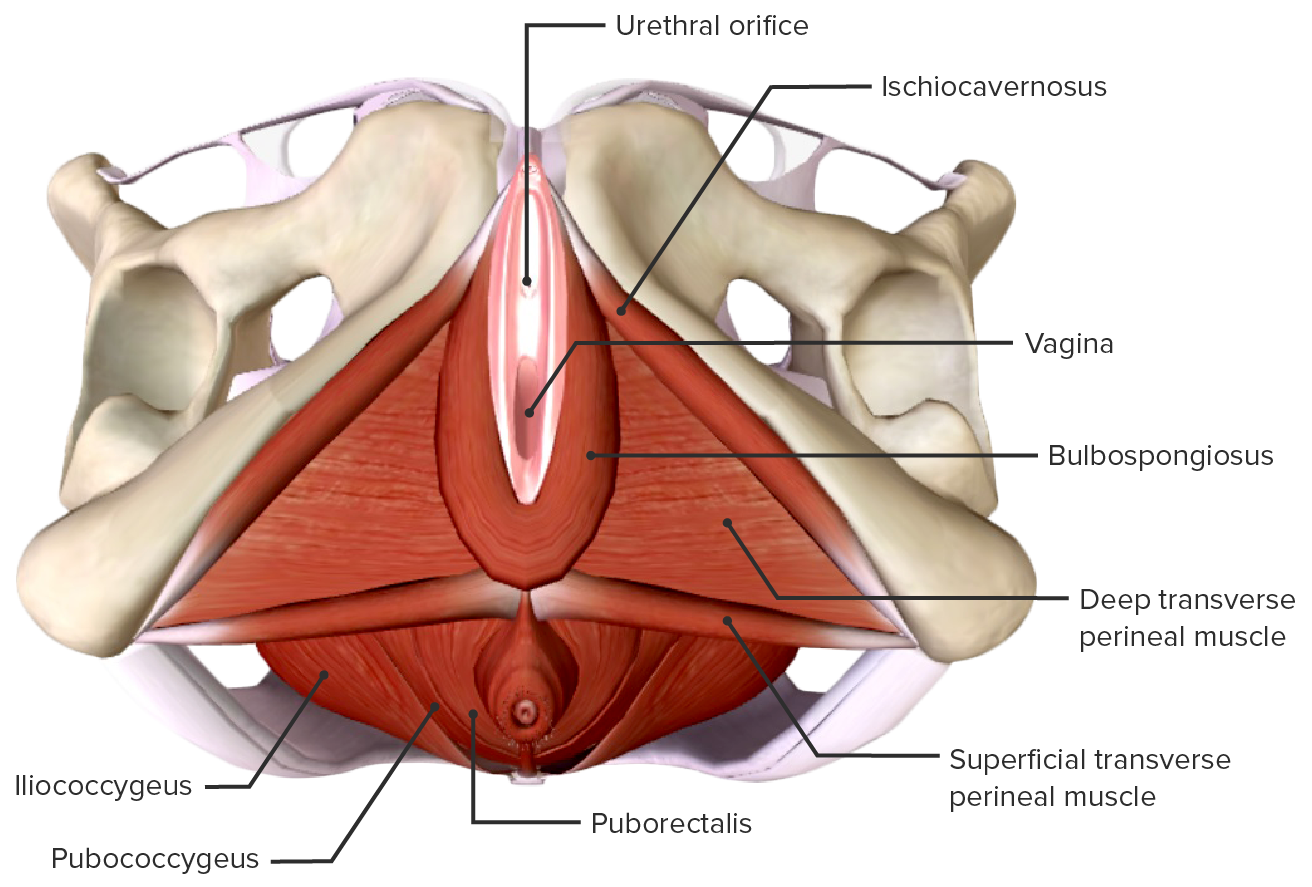
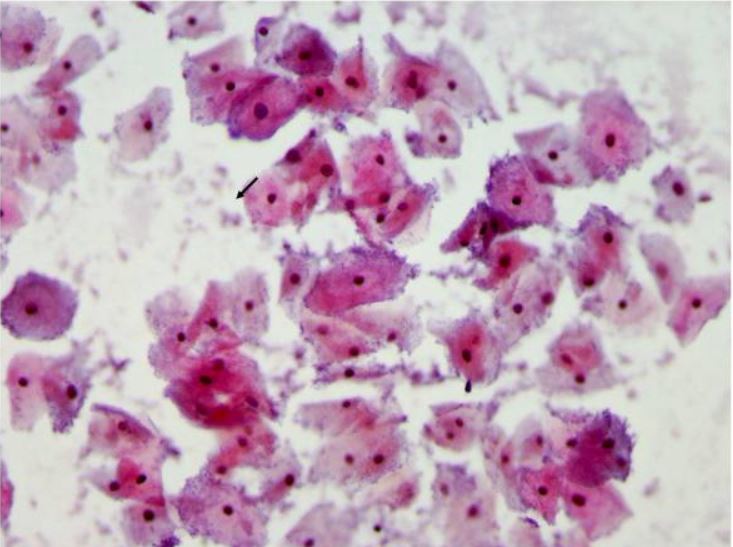
00:01 In this lecture, we will discuss vaginitis. Vaginitis is an inflammation of the squamous epithelial cells lining the vagina. It commonly leads to vaginal discharge. More than 90% of cases in adolescents are caused by either bacterial or yeast infections. So, what are the causes? About 20% to 25% of the time, it’s vulvovaginal candidiasis. A substantial amount of time, it’s bacterial vaginosis. 00:29 It can be trichomoniasis or it might be some other problems such as mycoplasma genitalium or ureaplasma. So, what are the risk factors for vaginitis? One is unprotected sexual intercourse, having multiple partners, having a new sexual partner, having a history of sexually transmitted infections. 00:50 Frequent douching increases risk of vaginitis and having recent antibiotic use can increase your risk of yeast infections. So, let’s talk about BV and candidiasis. Lactobacillus is predominant in normal flora in the vagina. The normal post-pubertal pH is about 3.8-4.2. When you disrupt the normal vaginal flora or alter the pH, this can lead to overgrowth of other flora such as candida which causes vulvovaginal candidiasis or Gardnerella which causes bacterial vaginosis. There is also a sexual transmitted vaginitis which is caused by Trichomonas. Trichomonas is an anaerobic parasitic protozoan. 01:38 It has a flagella which aids in its motility. It can adhere to the vaginal epithelial cells which can lead to cellular damage and mucosal inflammation. In males, it’s usually asymptomatic or only mildly symptomatic. 01:53 So, important questions to ask a patient with vaginitis is about the vaginal discharge. When did this start? How long has it been going? What’s the color or the odor or the consistency or the quantity? Get a sense of that. Then, also ask about sexual activity. It’s important to ask about hygiene habits because douching is part of this problem. Also, ask about recent antibiotic use. It might be your patient has a yeast infection. When you examine the patient, look at the external genitalia. 02:25 Look for vulvar erythema or edema. Look for any genital lesions that might be going on. 02:30 Assess for inguinal lymph nodes. Those will be more common in infections. Also, it’s reasonable to do a speculum exam in patients who are compliant to look and visualize the discharge. Assess the color or the consistency and see if there’s drainage from the cervical os. If that’s the case, think about cervicitis. 02:49 So, let’s go through our differential. One thing this could be is just a non-specific vaginitis. 02:56 This can happen from poor hygiene, from improper wiping, from having tight clothes, or perhaps from chemical irritation like bubble baths. Possibly this is physiologic leukorrhea. 03:07 Perhaps, this is just a result of rise in estrogens during puberty. It precedes menarche by generally 3-6 months. 03:15 Also, this could be vaginal discharge from a cervicitis such as chlamydia. That can be mistaken for a vaginitis. Remember, increasingly we’re recognizing mycoplasma genitalium and ureaplasma but most centers don’t have a way to test for that yet. So, how should you assess a patient with vaginitis? Typically, we do a vaginal microscopy or a wet mount. We can look at a saline wet mount and visualize epithelial cells, see clue cells, look for white cells, or look for Trichomonas. 03:47 They’re obvious on exam. We can do a KOH prep. In this case, we can visualize hyphae consistent with the yeast infection. Additionally, it’s reasonable to check the pH and make sure that the pH is within the normal range. But a culture is generally not needed for a diagnosis of vaginitis. 04:05 Usually, you can pick it up from one of these tests. Additionally, more and more, some centers are moving towards just molecular testing alone without the microscopy. This can be done on a self-administered swab by the patient. So, how do we treat these patients? For vulvovaginal candidiasis, we typically do fluconazole, 150 mg by mouth, just one dose and almost always, they’ll get better. For bacterial vaginosis, we may do metronidazole, 500 mg by mouth, twice a day for seven days or alternatively with fewer side effects, we can do a vaginal suppository of metronidazole. For trichomoniasis, we would give Flagyl and we would give a 2 g single dose. That usually does the trick. There are some potential complications to vaginitis. One of them is preterm labor. So, we want to avoid vaginitis in pregnant women. 05:03 Additionally, it can cause a premature rupture of membranes or low birth weight in newborns, generally bad with pregnancy. Vaginitis also increases risk of sexually transmitted infections for complicated reasons. It could be something to do with the vaginal flora or it could be the fact that these two things have the same risk of multiple partners. So, how can we prevent vaginitis? Well, we should promote condom use. Certainly, we should discourage douching or intravaginal hygiene products as they change the pH and increase risk for infections. Likewise, it’s important to remember that eating yogurt as a way of providing lactobacillus does not prevent infections. 05:47 There’s not that much lactobacillus in yogurt and it’s not getting into the right place. 05:51 Lastly, we should certainly address hygiene issues, general hygiene issues as well as the douching issue. 05:58 So, that’s my review of vaginitis in adolescent girls. Thanks for your time.
About the Lecture
The lecture Vaginitis in Adolescent Girls by Brian Alverson, MD is from the course Adolescent Medicine. It contains the following chapters:
- Vaginitis
- Treatment Options
Included Quiz Questions
Which of the following is least likely to cause vaginitis?
- Bacillus cereus
- Mycoplasma genitalium
- Ureaplasma species
- Trichomonas vaginalis
- Gardnerella species
Bacteria are the cause of vaginitis in approximately what proportion of patients?
- 50%
- 25%
- 10%
- 75%
- 90%
Which of the following is not a risk factor for vaginitis?
- Protected sexual intercourse
- Previous history of sexually transmitted disease
- New sexual partner
- Frequent douching
- Multiple sex partners
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This lecture gives clear ideas about the etiology, diagnosis, risk factors and the treatment. Thank you!