Playlist
Show Playlist
Hide Playlist
Varicose Veins: Pathogenesis
-
Slides 09 VascularMedicine advanced.pdf
-
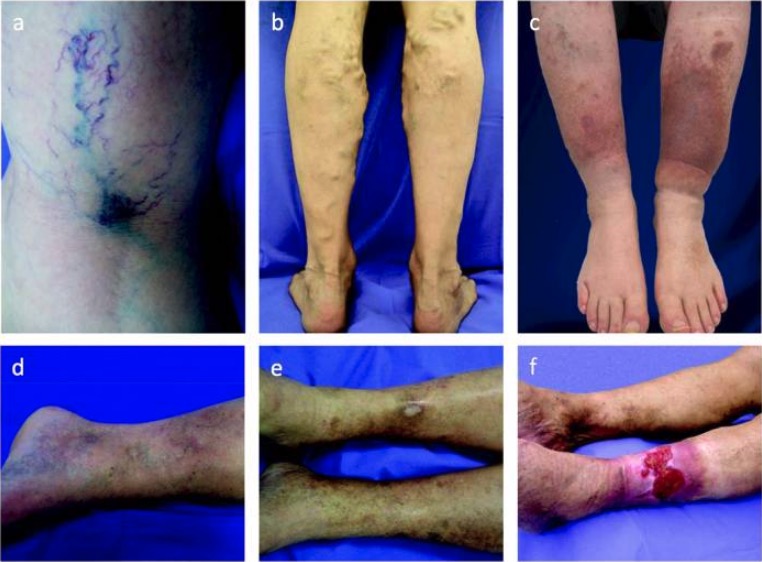
Download Lecture Overview
00:02 Varicose veins can result in superficial phlebitis. That is the veins are sitting on the surface, they can be easily traumatized with a small bruise or traumatic injury. This leads to inflammation and can lead to thrombosis. 00:21 But superficial phlebitis in a varicose vein usually doesn’t result in pulmonary embolism. 00:27 Treatment is local heat, for example with a heating pad; elevation of the extremities so you help the vein to drain; and then drugs: aspirin or ibuprofen can reduce the inflammation and reduce the tendency towards clot forming. 00:44 The combination of varicose veins and deep inside venous insufficiency – that is the valves not working well or internal varicose veins if you will – that increases the risk for DVT – deep venous thrombosis – and pulmonary embolism because the blood tends to stagnate there. And also the walls of these veins are not normal in terms of their ability to prevent blood clots from forming. And so the deep system can become thrombosed and that can lead to pulmonary embolism. And we’ve talked about how dangerous pulmonary embolism can be. 01:24 With the patients who have this situation chronically – that is they have deep vein insufficiency, the veins are dilated internally, the valves don’t work well – it is very common that there is congestion of the tissue with the blood that doesn’t drain adequately out of the legs. Edema – or swelling – occurs. Lots of fluid in the tissues. Again, as I mentioned before, as the swelling goes up in the tissues, tissue nutrition – getting blood, oxygen and nutrients to the cells – becomes impaired. And you can actually have necrosis, or death, of tissue, particularly the subcutaneous – that is the fat deposits under the skin. 02:08 These skin areas develop brown pigmentation. What happens here is that red blood cells escape from the capillaries because of the high pressure. They degenerate there and they deposit hemoglobin which is metabolized locally into a compound called hemosiderin which is an iron compound derived from hemoglobin and is brown. And so the skin, as you can see in the picture there, is quite brown in the lower extremity from chronic venous disease. 02:41 Again, so much fluid develops that the lymphatics are unable to drain it. And you may actually, because of inadequate nutrition, get scarring or sclerosis of the lymph channels and this even further increases the amount of swelling in interstitial fluid. And you may even get a form of dermatitis – or skin inflammation – and venous ulcers, as I’ve already talked about. And in very severe cases it might even lead to amputation.
About the Lecture
The lecture Varicose Veins: Pathogenesis by Joseph Alpert, MD is from the course Venous Diseases.
Included Quiz Questions
Chronic venous insufficiency can cause all of the following conditions except ?
- Auto-immune hemolytic anemia.
- Chronic foot and/or ankle ulcers.
- Chronic lower extremity edema.
- Recurrent deep venous thrombosis.
The skin appears brown in chronic venous insufficiency due to..?
- Hemosiderin.
- Hemoglobin.
- RBCs.
- Ferritin.
- Hepcidin.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |