Playlist
Show Playlist
Hide Playlist
Vascular Remodeling: Glagov Phenomenon
-
Slides Plaque Morphology and Complications.pdf
-
Download Lecture Overview
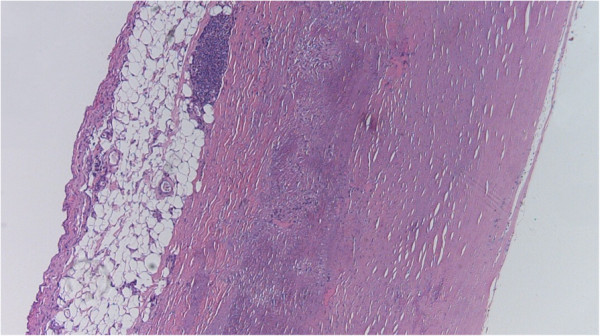
00:00 All right then, this session we'll look at plaque morphology and the complications that occur, as a difference between different kinds of plaque. 00:11 Not all plaque is created equal. 00:14 Here's where we are on our roadmap. 00:17 We've already talked about risk factors and how we build a plaque. 00:20 Now we're going to talk about differences in the way the plaques look, and they behave. 00:27 In interesting phenomena, that was identified in the 60s and 70s by Dr. Glagov is this phenomena where as we build atherosclerotic plaque going from left to right. 00:41 As we get more and more plaque accumulation, the vessels can accommodate this by undergoing remodeling. 00:49 And so for the first four circles, even as we get more and more atherosclerotic plaque that compromises the lumen more and more. 00:58 The lumen size as the vessel has expanded hasn't changed. 01:02 It's the same lumen size. 01:05 However, we do reach a point where the vessel can't remodel anymore. 01:09 And as we accumulate more and more plaque, the last two circles on the right, we do get a smaller and smaller lumen with less and less flow going down that. 01:20 But up to a certain point, we can't see any significant atherosclerosis. 01:24 This has implications when we do angiography because angiography, putting in radio contrast material into a vessel only looks at the luminal diameter, and can't really assess the accumulation of atherosclerotic plaque, because of this outward remodeling of the vessel, the Glagov phenomenon. 01:44 So that's one important point. 01:46 We do reach a point, also where we have clinical significance, and this, this Rubicon is typically identified as about 70% stenosis. 01:56 At this point, we don't have any more ability of the vessel wall to remodel and that 70% luminal stenosis is starting to limit blood supply. 02:07 Let's look at that. 02:09 So on this graph, we're looking at coronary flow reserve on the Y axis, we're looking at the degree of stenosis or diameter narrowing on the X axis, and about that critical stenosis that 70% Rubicon resting flow is not compromised, so we will have no symptomatology at rest. 02:30 But if we increase activity, if we increase demand on the heart, if we increase heart rate, or blood pressure, then that 70% percent stenosis starts to significantly impact the amount of blood that can get in. 02:46 And we will start to have symptomatology, we will have supply demand mismatch, and patients will start presenting with anginal symptoms. 02:56 Usually, when angina occurs, patients don't continue to exercise through that or to continue their activity through that, and they get back to resting conditions. 03:05 And so we avoid a heart attack. 03:07 So angina is a warning signal, and that 70% stenosis starts occurring then. 03:14 Let's look at the progression of atherosclerosis. 03:16 A normal vessel is shown here on this trichrome stain, and the arrow is pointing to a little bit of an intimal proliferative process. 03:24 So what's now highlighted in green is a very small, early intimal lesion. 03:30 This is not going to be in any way shape or form, impeding vascular flow. 03:35 And even as this is developing, we're starting to get outward remodeling, so we would see no diminution of flow. 03:42 Further on, once we reach that 70% stenosis, again, on a trichrome stain here, we will develop so called stable angina, certain levels of activity, certain demands on the heart will exceed the capacity of the vessel to perfuse that heart, and we'll get symptomatology. 04:01 We may get chest pain or angina, we may get symptoms of congestive heart failure with shortness of breath. 04:08 And now highlighted in green, you can see the degree of atherosclerotic plaque development. 04:15 It looks like it may be even more than 70%. 04:18 But that's because in this vessels, we've taken it out of the body without pressure in the lumen. 04:23 The lumen has been collapsed by all of that surrounding smooth muscle and extracellular matrix. 04:30 And then, importantly, atherosclerosis doesn't just progress by the accumulation of atherosclerotic plaque. 04:41 There can be acute events where the plaque ruptures. 04:46 And now we expose to the following blood underlying matrix including Von Willebrand factor and tissue factor and other things that will cause an acute thrombosis. 04:59 So in this vessel that's shown here in the final panel. 05:02 Now in green, that's the degree of atherosclerosis, there really wasn't that much atherosclerosis, maybe 30 or 40% overall. 05:12 But this plaque wasn't stable, it ruptured. 05:16 And now we have a superimposed thrombus that's in the middle, that was completely occlusive. 05:21 And we went from maybe a 30, or 40%, chronic stenosis to now 100%, acute occlusion. 05:29 And this patient suffered a myocardial infarct as a result of that. 05:33 So let's talk about those changes now that occur, acutely. 05:39 Atherosclerosis is a disease that has a long horizon. 05:45 There is a very long preclinical phase, it takes decades fortunately, in most of us, to develop any significant atherosclerotic plaque. 05:54 And we go from a normal artery, first to a fatty streak. 05:58 Fatty streak is where we're getting the accumulation of lipid underlying dysfunctional endothelium with or without some macrophages that are also taking up that liquid to become foam cells. 06:11 That is actually reversible process. 06:12 That's why you see that double headed arrow, and we can actually go back to a completely normal artery. 06:19 That fatty streak, however, can progress, we can accumulate more inflammatory cells, which will recruit and activate more smooth muscle cells, which will lay down more matrix and eventually we get a combination fibrofatty plaque or atherosclerotic plaque. 06:34 From that point, there are a couple different ways that we can diverge. 06:38 So we can have progressive accumulation of material. 06:42 We have a stable plaque and it just keeps getting more and more and more driven by the usual processes. 06:50 That will happen over decades. 06:52 And eventually at some point, we get that critical stenosis, we exceed the capacity of the vessel to remodel, we get beyond 70% chronic stenosis, and then we get symptomatology that is the kind of the critical stenosis. 07:08 The other way that this can go from a fibrofatty plaque is so something so called a vulnerable plaque. 07:14 This plaque is unstable for reasons that we'll talk about in the subsequent slides. 07:19 But from a vulnerable plaque, we can actually have a vessel wall that completely ruptures or formation of an aneurysm that ruptures and we can have a catastrophic event that way. 07:32 Or we can have that plaque as we saw on the previous slide, break. 07:37 And now we're exposing underlying, very thrombogenic matrix elements and necrotic debris and other things that will now take us from whatever degree of stenosis we had to a complete occlusion by thrombus. 07:51 So it takes a long time to get to a point where then something happens. 07:56 Okay? Preclinical phase clinical phase.
About the Lecture
The lecture Vascular Remodeling: Glagov Phenomenon by Richard Mitchell, MD, PhD is from the course Atherosclerosis.
Included Quiz Questions
What is an example of the clinical application of the Glagov phenomenon?
- Angiography
- Ultrasonography
- MRI scan
- CT scan
- PET scan
What phase of atherosclerosis manifests in middle age?
- Clinical
- Stable
- Vulnerable
- Preclinical
- Stenotic
What type of plaque is associated with aneurysm and rupture?
- Vulnerable
- Stable
- Fibrofatty
- Fatty streak
- Mature
Angina is a warning symptom of an impending...
- ...myocardial infarction.
- ...cerebral infarction.
- ...septic shock.
- ...myoclonic seizure.
- ...pulmonary embolism.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |