Playlist
Show Playlist
Hide Playlist
Urgent Gynecologic Disease
-
Slides GynUrgentDiagnoses AcuteCare.pdf
-
Download Lecture Overview
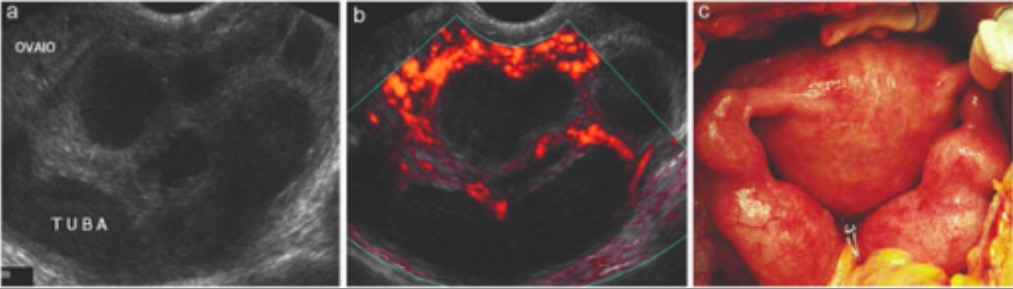
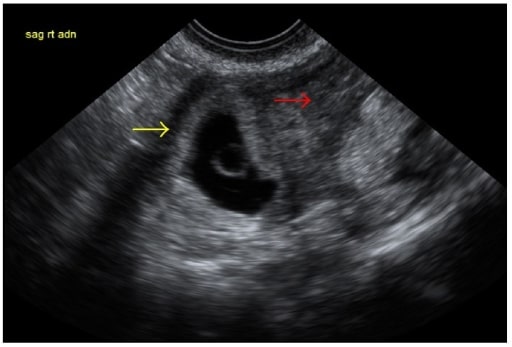
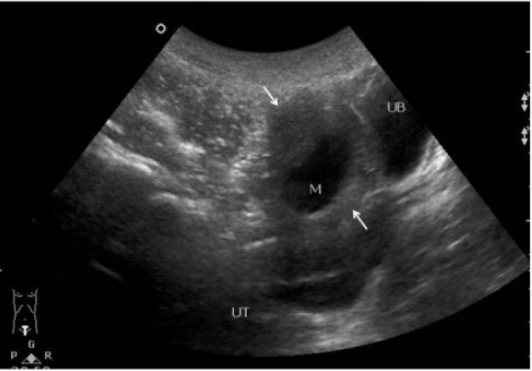
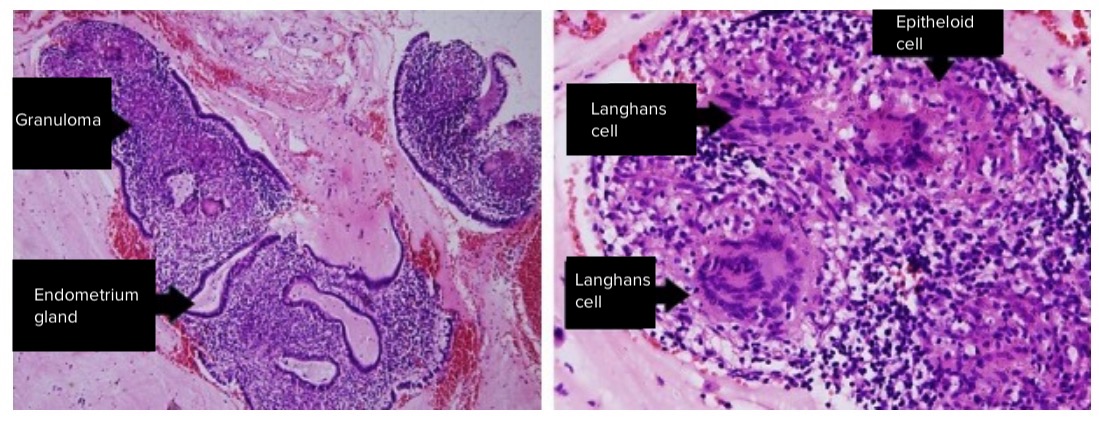
00:01 So, now we’re going to discuss urgent gynecologic issues. 00:04 And I think that we’re going to highlight a few disorders that are absolutely critical to know if you're taking care of women in your practice. 00:12 So, the ones that I am going to focus on today, I’m going to start with pelvic inflammatory disease. 00:17 Then we’ll move on to ectopic pregnancy and ovarian cysts. 00:21 So, let’s talk about pelvic inflammatory disease (or PID). 00:25 Now, classically, and still to this day, we think of sexually transmitted infections – Neisseria gonorrhoeae, Chlamydia trachomatis – as causing most cases of PID, but it should be noted that up to 40% of cases are polymicrobial, involving even gram-negative organisms. 00:44 And that percentage is increasing over time. 00:48 And so, the classic signs you look for are cervical motion tenderness and mucopurulent cervical discharge on your speculum examination, but you can't hang your head and say all cervical motion tenderness is therefore PID. 01:02 Just remember CMT is present in about a quarter of cases of appendicitis, in about half of cases of ectopic pregnancy. 01:10 So, just because a patient has cervical motion tenderness doesn't mean -- equal they have PID. 01:14 Still can be one of these other diagnoses which can very much mimic pelvic inflammatory disease. 01:20 However – and I think for a very great way to help rule out PID while you’re waiting for your cultures is do a wet mount. 01:30 If there is no white cells present, the chance the case is actually pelvic inflammatory disease and not one of those other conditions is a lot lower. 01:42 So, obviously, with PID, it mandates immediate treatment with antibiotics, including parenteral antibiotics. 01:48 For patients who are more sick, and I'm talking about folks who have a blood pressure that’s declining, pulse that's high, evidence of systemic infection and/or they are pregnant where we’re going to be more aggressive with the treatment of PID, they are going to get IV therapy. 02:07 Cefotetan or cefoxitin plus doxycycline and clindamycin plus gentamicin can also be used. 02:15 Again, those are options that are helpful in pregnancy instead – and avoiding the doxycycline option. 02:21 That said, most patients receive intramuscular or along with oral treatment with ceftriaxone plus oral doxycycline. 02:29 And that can include oral metronidazole. 02:32 For patients who receive either treatment, it’s important that they get follow-up to make sure that they're doing better because pelvic inflammatory disease is associated with a risk of infertility and also associated with a risk of broader infection, such as tubal ovarian abscess or even systemic sepsis. 02:50 And so, therefore, it's important to make sure that patients are doing better. 02:55 Let’s move on to ectopic pregnancy now. 02:59 So, it's not uncommon. 03:01 As you can see in the picture, that is an ectopic pregnancy. 03:05 You can see that – a tubal pregnancy there on the left side of your picture. 03:09 Ectopic complicates 1 to 2% of all pregnancies. 03:13 And a classic symptom, which could be on your exam, abdominal pain along with first trimester bleeding. 03:20 And again, it’s always important to think about things like ectopic pregnancy in cases of abdominal pain among women of childbearing age. 03:29 So, always consider pregnancy and its complications when dealing with pain issues. 03:35 Diagnostic workup includes a transvaginal ultrasound to start with. 03:39 If that is non-diagnostic because it’s early in the pregnancy, a quantitative beta-hCG is really helpful. 03:47 Among most women early in pregnancy, when they have a healthy pregnancy, you can expect the beta-hCG level to double about every 2 to 3 days. 03:56 A quantitative mark that falls off that table can be suggestive of an ectopic pregnancy and, therefore, treatment may need to be initiated. 04:05 If the level is falling because this can also be associated with a missed abortion, for example, you want to follow those levels to – until they’re undetectable because of the possibility of something like a hydatidiform mole or a molar pregnancy. 04:25 Ectopic pregnancy is often treated surgically, but methotrexate can be just as effective as surgery. 04:32 Just remember that it does have contraindications. 04:35 It is a powerful drug, even though it’s used in a limited setting in ectopic pregnancy. 04:40 Patients with lung, kidney or liver disease or severe hematologic illness should not be receiving methotrexate. 04:46 It’s usually a single dose given intramuscularly. 04:50 And even among patients with declining beta-hCG levels who are minimally symptomatic, watchful waiting may be okay for those patients, but you have to ensure that they have very good follow-up because, obviously, a rupture or an infection could be complicated and very devastating for these patients if left untreated. 05:13 Methotrexate can be less effective in certain cases. 05:18 When there’s evidence of fetal cardiac activity, methotrexate is not going to be as effective as surgery when there's a larger gestational sac, when there’s higher serum progesterone levels. 05:28 So, all signs of a more advanced pregnancy, including higher levels of a beta hCG. 05:33 Once the beta hCG level hits 2000, methotrexate is only about 40% effective and those patients should be considered for surgical option for a treatment of their tubal pregnancy. 05:46 All right. Let’s talk about another issue, are ovarian cysts. 05:50 Ovarian cysts, really common. 05:51 About one in five women develop ovarian cysts over a lifetime. 05:56 Ruptured ovarian cysts, another common condition, can be very painful, but it’s usually just a question of supportive pain management until the symptoms reside because usually the symptoms do resolve over the course of days. 06:09 And screening women for ovarian cysts, most of these cysts are benign. 06:15 Benign cysts are more likely to have thin walls, be unilocular and be less than 10 cm in diameter. 06:21 Those are all characteristics of benign ovarian cysts. 06:24 Once encountered, it's important to consider a serial ultrasound follow-up for these patients. 06:30 It doesn't mean the patient needs surgery, but serial ultrasound can ensure that it's not growing. 06:36 And in fact, many simple cysts resolve spontaneously. 06:40 The majority do. 06:41 And so, that's what the serial ultrasound is designed to do. 06:43 It’s to really ensure that the cyst involutes and resolves on its own because giving oral contraceptive pills or birth control pills, aspirating the cyst doesn't really help in resolving them unfortunately. 06:57 And for persistent cysts, cysts that are changing in character, particularly among women who are close to menopause or menopausal, that's the time to start to worry about the potential for a malignancy, getting a tumor marker such as CA 125 and also referring to gynecology for further evaluation is in order for those cases. 07:22 All right. So, we talked through some of the main emergencies and urgent issues associated in gynecology and we’re going to be talking about some more routine ones as well. 07:33 Thank you.
About the Lecture
The lecture Urgent Gynecologic Disease by Charles Vega, MD is from the course Acute Care. It contains the following chapters:
- Urgent Gynecologic Disease
- Ectopic Pregnancy
- Ruptured Ovarian Cyst
Included Quiz Questions
A 26-year-old woman presents to the clinic with 2 days of lower abdominal pain and vaginal bleeding. She has mild nausea. Her last menstrual bleeding was expected 15 days ago. Her vital signs are within normal limits. Her abdomen is soft with mild tenderness in the hypogastric area without guarding or rebound. Which of the following is the most appropriate next step in diagnosis?
- Beta hCG
- Abdominopelvic computed tomography scan
- Response to antibiotic treatment
- Laparoscopy
- Abdominal ultrasound
Which of the following is a major long-term complication of pelvic inflammatory disease?
- Infertility
- Uterine rupture
- Pyelonephritis
- Ovarian torsion
- Pericolic abscess
Which of the following clinical findings in patients with an ectopic pregnancy is best treated with methotrexate?
- Adnexal mass measuring 1.8 cm
- Beta hCG measuring 6,000 IU/L
- Presence of fetal cardiac activity
- Hemodynamic instability
- Unable to attend post-treatment appointments
Which of the following is the most appropriate management of a 4-cm left ovarian cyst in a premenopausal woman?
- Repeat ultrasound in 1–2 months
- Referral for surgery
- CA-125
- Oral contraceptive pills
- Oral antibiotics
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |