Playlist
Show Playlist
Hide Playlist
Upper and Lower Motor Neuron Diseases: Clinical Manifestations
-
Slides Diseases of the Motor Neurons.pdf
-
Download Lecture Overview
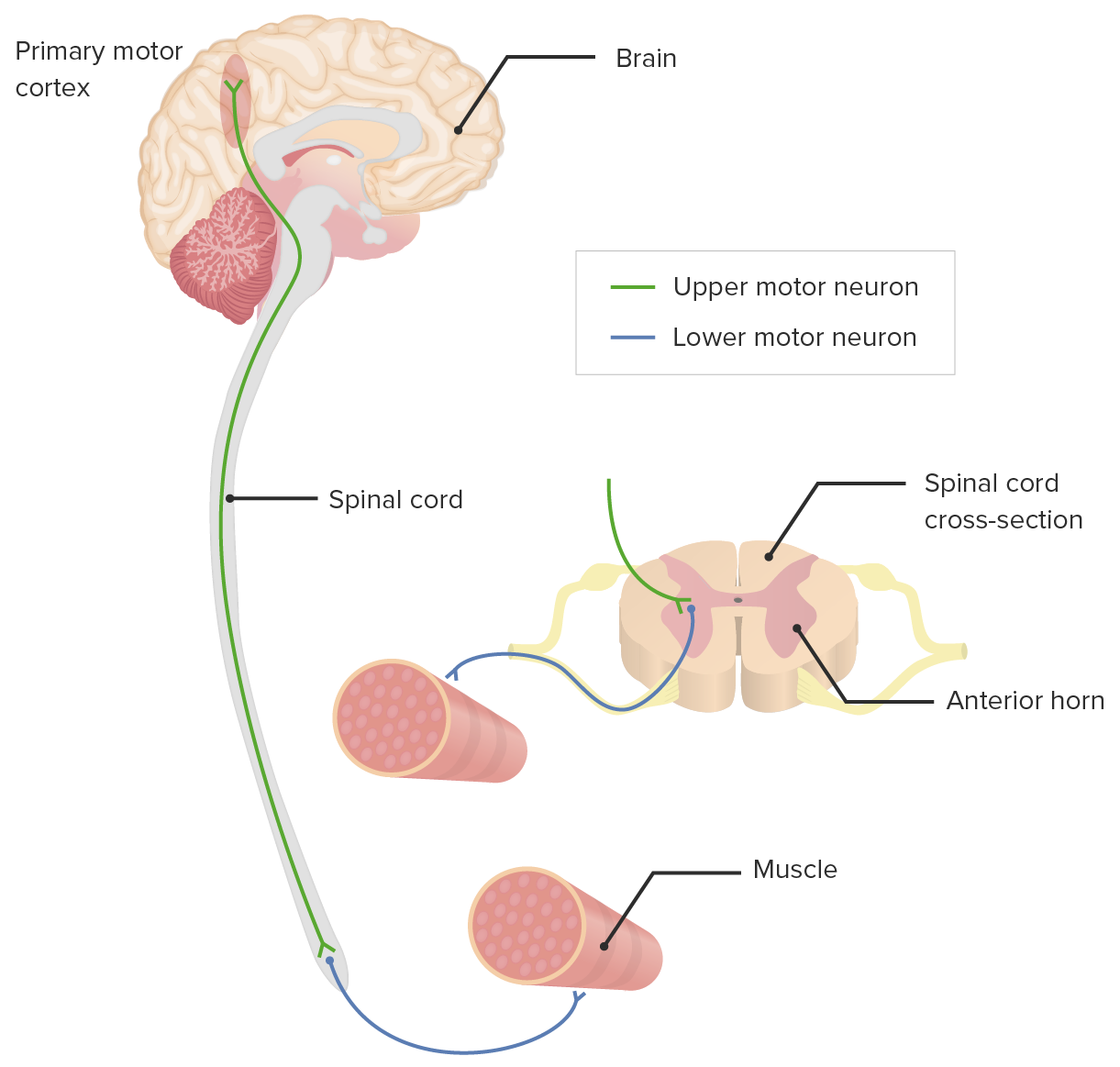
00:02 Now let's talk about the clinical manifestation of motor neuron diseases. 00:05 How do patients present? What are their signs and what are some of the symptoms? Well, we can see upper motor neuron signs and the typical clinical manifestations of upper motor neuron pathology, are demonstrated here. 00:18 We can see weakness, weakness can come from a problem of any of the motor nerves - primary motor neuron, the upper motor neuron, or the secondary motor neuron, the peripheral lower motor neuron. 00:29 We can see increased tone, and spastic tone is a classic sign of upper motor neuron pathology. 00:36 Sspasticity is what we see in evaluating tone when we look at passive range of motion of the muscles. 00:42 Hyperreflexia is a classic sign of upper motor neuron pathology. 00:47 We don't see fasciculations. 00:49 Fasciculations suggest lower motor neuron pathology, so we don't see that from upper motor neuron disorders. 00:55 And we can see rigidity, it's often a clasp, knife rigidity, which is really spastic tone that we're seeing. 01:02 Spasticity is both velocity and angle dependence. 01:05 And so the faster you move the limb with passive movement, the more tone there is, and so when you're moving really quickly, there's a lot of tone. 01:12 When you're moving slowly, there's relatively less tone. 01:16 It's also angle dependent. 01:17 We see that that increase in tone is more severe out of extension, and less severe in at flexion. 01:23 And so those are features of clasp-knife rigidity, and suggestive of spasticity are a problem with the upper motor neurons, the pyramidal system, they're pyramidal findings. 01:35 Clonus is a significant hyperreflexia, 4+ hyperreflexia where there's sustained beating of a deep tendon reflex, and the Babinski sign or an extensor plantar response is indicated, is an indicator of upper motor neuron pathology. 01:53 What about upper motor neuron bulbar symptoms? This has been coined pseudobulbar palsy, which is those same upper motor neuron dysfunction and disorders affecting the corticobulbar fibers. 02:06 We can see slurred speech, dysphasia, a spastic dysarthria where there's really stiffening of the vocal cords and oral pharyngeal muscles, tongue spasticity, reduced mobility of the tongue, both with protrusion or lateral side to side movements. 02:22 pseudobulbar affect is emotional lability. 02:24 It's a spastic emotion where patients have really high highs and really low lows. 02:30 They cry when they're not sad, they laugh when they're not happy. 02:33 And that emotional lability is that same spasticity that we see in the motor nerves, but here we're seeing him in emotional control. 02:40 And that's likely due to motor control of the face, unprovoked crying, laughing and anger. 02:47 We can see a hyperactive gag reflex and a jaw jerk. 02:50 And typically, with a patient modestly or minimally opening their mouth and we tap on the jaw with a reflex hammer, we don't see much in the way of a jerk of the jaw. 03:01 And in upper motor neuron disorders tapping on the jaw results in an intense biting jaw jerk which is indicative of upper motor neuron signs or upper motor neuron pathology of the corticobulbar fibers. 03:15 We can also see lower motor neuron dysfunction in motor neuron disorders. 03:19 And here are some of the clinical manifestations we can see from lower motor neuron dysfunction. 03:23 Again, weakness we can see from problems with any of the motor nerves, upper or lower. 03:28 Atrophy is very common with lower motor neuron pathology. 03:32 Fasciculations are really important. 03:35 They are pathognomonic for lower motor neuron dysfunction. 03:38 These are visible involuntary contractions of a single motor unit. 03:44 That's a motor nerve and all of the muscles that innervates and it looks like the patient is moving their muscle but with it relaxed. 03:52 It's very important when evaluating for fasciculations. 03:55 The patient is relaxed, all the muscles are still and and you're looking for involuntary contraction of a muscle group, which is a fasciculation and typically it looks like an undulation of the muscle. 04:09 We can see decreased tone from lower motor neuron pathology and hyporeflexia. 04:15 In addition, we can see lower motor neuron signs affecting the corticobulbar fibers. 04:19 We can see dysfunction in any area of the brainstem but frequently we can see and look for pathology affecting the medullary region of the brainstem. 04:29 Cranial nerves IX, X, XI and XII - we can see impairment in chewing, swallowing and tongue movements Tongue fasciculations and atrophy are one of the pathognomonic signs for motor neuron disease. 04:42 It's important that we look for tongue fasciculations and atrophy in patients suspected of motor neuron disorders and this is done by having the patient open their mouth and looking at the tongue in the relaxed and passive condition. 04:57 Protruding the mouth can cause the tongue to move and fasiculate, so we're really looking at passive a still position of the tongue to look for tongue fasciculations. 05:08 Diminished gag reflex and a jaw jerk that's normal or absent is also suggestive of lower motor neuron dysfunction of those corticobulbar fibers. 05:19 So let's compare some of the clinical findings with upper motor neuron and lower motor neuron lesions. 05:24 Knowing that with motor neuron diseases sometimes we see a combination of upper and lower motor neuron pathology. 05:30 First, we look for muscle tone. 05:32 With upper motor neuron lesions, we see spastic tone, increased tone, clasp-knife rigidity, and with lower motor neuron lesions, patients become hypotonic. 05:42 In terms of muscle mass, with classic upper motor neuron lesions, there's often no change though with long term upper motor neuron lesions, we can see a little bit of atrophy. 05:51 But with lower motor neuron lesions, we see prominent muscle wasting and atrophy that is particularly prominent on exam. 05:58 We need to look for fasciculations, we don't see fasciculations in pure upper motor neuron lesions, but we do when there's lower motor neuron pathology. 06:07 Deep tendon reflexes, we see hyperreflexia with upper motor neuron lesions, hypo/areflexia with lower motor neuron lesions, and this is important Areflexia, should point us squarely towards a peripheral nerve dysfunction and particularly the lower motor neuron. 06:23 And then on EMG, we typically see normal nerve conduction testing with pure upper motor neuron lesions and abnormal conduction , reduced amplitude of the compound motor action potential, the motor potential with lower motor neuron lesions. 06:39 Importantly, there is not a diagnostic test that says that this is a motor neuron disorder and we're using our clinical exam, the symptoms, the signs and in some cases EMG nerve conduction to support that diagnosis in these patients.
About the Lecture
The lecture Upper and Lower Motor Neuron Diseases: Clinical Manifestations by Roy Strowd, MD is from the course Diseases of the Motor Neurons.
Included Quiz Questions
Fasciculations are pathognomonic for which condition?
- A lower motor neuron lesion
- An upper motor neuron lesion
- A lesion in the primary motor cortex
- A cerebellar lesion
- A lesion in the internal capsule
Which statement concerning clasp-knife rigidity is correct?
- It increases with faster passive movement.
- It worsens as the joint angle becomes more acute (with flexion).
- It is a sign of lower motor neuron lesions.
- It is an extrapyramidal finding.
- It indicates a loss of muscle tone.
Which sign is most likely to be found in an upper motor neuron disease?
- Spasticity
- Fasciculations
- Atrophy
- Areflexia
- Abnormal nerve conduction studies
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |