Playlist
Show Playlist
Hide Playlist
Ulcerative Colitis
-
Slides GIP Ulcerative Colitis.pdf
-
Download Lecture Overview
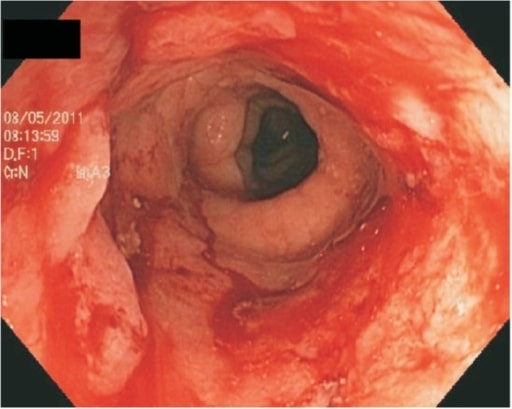
00:01 Welcome. We're going to be talking about the other variety of inflammatory bowel disease, Ulcerative Colitis. 00:09 Ulcerative Colitis, abbreviated UC, is an inflammatory bowel disease that begins in the rectum but may ultimately advance retrograde to involve the entire colon. 00:22 And it is associated with mucosal inflammation and ulcers. So it's a pretty good name, Ulcerative Colitis. 00:29 The epidemiology of this. There's going to be a slight bimodal distribution. 00:33 So, late teens and young adult. And it's a little bit older than the typical Crohn's patient. 00:41 There's a second peak that occurs between the ages of 50 and 70. 00:46 In general, men are more likely to be affected than women. 00:49 So, this is also different than Crohn's where there is an equal gender representation. 00:53 The known genetic risk factors include association with HLA-B27. There are others kind of dietary and other associations that are seen. 01:05 The actual mechanisms of their association are not completely understood. 01:10 So, if you have a high fat intake, there's a higher risk of ulcerative colitis. 01:15 If there's a lot of non-steroidal anti-inflammatory drug, it's the same thing. 01:19 If there is stress, the same thing. 01:23 This is likely to be increased incidence in a patient who is otherwise prone to it on the basis of their genetic makeup. 01:32 Intestinal infections likewise can cause a dysregulation of immune response that can ultimately be kind of set in stone and turn into an Ulcerative Colitis. 01:46 The pathophysiology here is similar but different than what we saw in Crohn's Disease or the other form of inflammatory bowel disease. 01:54 We're looking at epithelium here. 01:56 Epithelium will have a normal tight junction, will have a normal mucous production and we form a barrier between whatever is in the colonic lumen and what is in the submucosa. 02:10 There is constant surveillance of the luminal contents, whatever bacteria are there. 02:15 And those are being presented by antigen presenting cells, macrophage and dendritic cells to the T-cells, regulatory T-cells that also live in a submucosa. 02:27 Under the setting of normal epithelial barriers. In normal epithelial immune regulation, all we do is make a lot of regulatory T-cells which fundamentally say, "Okay, the bacteria that we have recognized are good guys. We're not going to deal - do anything with them. Just ignore them." That's the normal setting. On the other hand, in patients who are going to be prone to having ulcerative colitis, they may have an imbalance in the mucin layer. So, the bacteria can potentially get across more readily. 03:02 There may be defective regulation of the tight junction, separation of the epithelial cells. 03:06 There may be a change in the commensal microbiota. 03:10 In that setting, we get an increased involvement, increased permeability and antigen uptake of all of the organisms that are otherwise sitting in the lumen. 03:23 And in the appropriate host, associate with HLAB27 for example, then, the antigen-presenting cells, the dendritic cells and the macrophages will stimulate proinflammatory T-cells. 03:36 In the setting of Ulcerative Colitis, this is going to be predominantly a Th2, a helper T-cell type two response, recall or if you have not yet looked at the video in Crohn's disease, it's predominantly a Th1 response. 03:55 In the setting of a Th2 response, we will get now an increased production of those cells as well as the production of Th2-like proinflammatory mediators like interleukin-4, interleukin-10, interleukin-13. 04:10 The clinical presentation, the patients who have Ulcerative Colitis in general systemically, there may be anemia. 04:17 They may have a malabsorption syndrome. There will be weight loss. 04:21 Although, mostly, this is impacting the colon. The colon being the major source of absorption of water, you can still have weight loss by having increased bowel motility and the proinflammatory state overall may drive an anorexia and an increased weight loss. 04:45 There may be a low-grade fever because of the proinflammatory state. 04:49 The GI manifestations as opposed to the systemic manifestations. 04:53 There's a refractory, often, blood diarrhea. There's focal urgency and incontinence. 04:58 There is tenesmus which is the strain of stool. 05:01 And because of the straining of stool, there's often frequently increased colicky lower abdominal pain. 05:08 All of this is because that inflammation is causing increased spasm of the smooth muscle lining the colon. 05:16 There are a number of extraintestinal manifestations and you may just have to memorize these. 05:21 There is no rhyme or reason to these particular entities but they are associated with in-patients who have Ulcerative Colitis. 05:28 Some of this may be a general proinflammatory setting. Some of this may be specifically related to unique antigenic responses. 05:37 In any event, patients with Crohn's, in any event, patients with Ulcerative Colitis will be more likely. 05:44 They won't always but be more likely to have primary sclerosing cholangitis, pyoderma gangrenosum. 05:50 I will show you that in the next slide. Erythema nodosum which is what we're looking at on this slide and eye inflammation. 05:57 As promised, on this side, there is pyoderma gangrenosum. So, a cutaneous gangrenous legion with ulceration and a peripheral erythema. 06:08 Other extraintestinal manifestations are peripheral arthritis, inflammation of the spine, ankylosing spondylitis and osteoporosis, maybe due to vitamin D or calcium malabsorption. 06:20 Painful oral ulcers such as aphthous ulcers and hypercoagulability may occur because of the proinflmmatory state driving the production of procoagulant factors. 06:32 Making the diagnosis. So, ultimately, it's going to be a pathologic diagnosis that cements this and that's where pathologists come in. 06:42 This is just showing you an example of a focal lesion within the colon and in a resected specimen. 06:50 We will do some other ancillary studies. So, we'll do a complete blood count, see whether the patient is anemic, whether they have an elevated white count. 06:58 See whether they're kind of systemically proinflammatory in which case, we might see elevated thrombocytosis. 07:04 There is a metabolic panel for electrolyte imbalances. 07:08 We may look for iron deficiency and vitamin B although, those are less common in ulcerative colitis because this typically only affects the colon and not the areas of the small bowel responsible for absorbing those nutrients. 07:21 However, if we are losing blood because of ulceration of the colon, we may have an iron deficiency anemia. 07:28 There will be systemically elevated, kind of inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein. 07:37 CT may be used. Although it's not going to be our gold standard for making the diagnosis. 07:44 And you may see areas on CT of induration, thickening of the bowel. 07:50 On the left-hand side, the arrow is pointed to a segment of the ascending colon near the cecum that is markedly indurated. 07:57 So, this was Ulcerative Colitis that went all the way around and involved the cecum. 08:02 On the right-hand side, we're just seeing involvement mainly within the sigmoid column. 08:08 Biopsy is your friend in this instance. And a colonoscope will go up, look for areas of ulceration, loss of mucosa, erythema and we'll take a biopsy there. We will see loss of epithelium. 08:22 We will see a very prominent, intense lymphocytic and macrophage rich infiltrate within the lamina propria and that's the findings that will make our diagnosis of Ulcerative Colitis. Having made the diagnosis, what do we do? So, we want to make sure that we don't ignore the nutritional deficiencies if they exist and we'll supplement with vitamins as necessary. 08:48 We will give antidiarrheal agents just because that provides some symptomatic relief to our patients. 08:52 Although, it clearly doesn't fix the underlying inflammation. 08:55 To do that, we need to give antibiotics, sometimes, by changing the colonic microbiota, we can influence what antigens are being presented to make the proinflammatory Th2 cells. 09:08 Similarly, corticosteroids by damping down inflammation may also be helpful and we may eventually go to other immunomodulators or anti-tumor necrosis factor therapies, infliximab and adalimumab and those are quite effective. 09:25 In severe disease, it may be that all of those interventions don't work and we then, have to do a colonic resection. 09:37 However, it's also important to realize in patients with ulcerative colitis. 09:41 They have chronic inflammation in the setting of epithelium that's regenerating. 09:46 That's a perfect storm for generating adenocarcinoma. 09:50 And for every decade that a patient with ulcerative colitis has active disease, there's a 10% increased risk of them developing adenocarcinoma. 09:59 So, we may elect in patients to prophylactically remove their colon so they don't develop colon cancer. 10:07 With that, we've reached the end of Ulcerative Colitis and one flavor of inflammatory bowel disease.
About the Lecture
The lecture Ulcerative Colitis by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
What is the age distribution of ulcerative colitis?
- Bimodal distribution: 15–35 and 50–70 years old
- Bimodal distribution: 15–45 and 60–70 years old
- Bimodal distribution: 5–45 and 60–80 years old
- Unimodal distribution: 35–45 years old
- Unimodal distribution: 25–35 years old
What is a genetic risk factor for ulcerative colitis?
- HLA-B27
- HLA-B14
- DRQ4
- DRQ8
- ATM2
What is NOT a risk factor for ulcerative colitis?
- Tylenol use
- Increased dietary fat intake
- NSAID use
- Stress
- Intestinal infection
What is an extraintestinal symptom of ulcerative colitis?
- Osteoporosis
- Weight gain
- Bloody diarrhea
- Fecal incontinence
- Night sweats
What is NOT typically part of the management of ulcerative colitis?
- PDL1 inhibitors
- Antibiotics
- Corticosteroids
- Immunomodulators
- Anti-TNF therapies
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |