Playlist
Show Playlist
Hide Playlist
Thrombotic Microangiopathies
-
Slides BleedingDisorders QuantitativePlateletAbnormalities.pdf
-
Download Lecture Overview
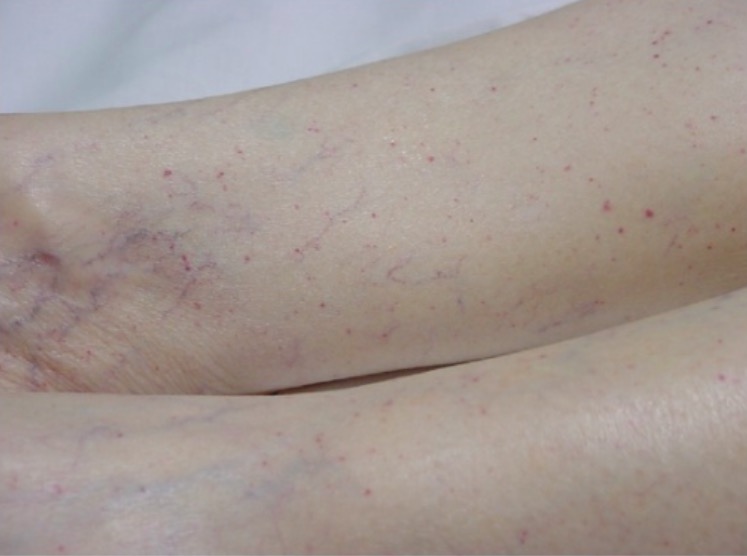
00:01 Thrombotic microangiopathies, what's going on with this? The little blood vessels are not developing thrombi. 00:09 Why? Well, we'll take a look at differentials coming up. 00:12 Common features, however, extensive formation of microthrombi in your blood vessel. 00:17 With the formation of the thrombi then you're consuming the platelet in the circulation, therefore, the patient is forming or suffering from thrombocytopenia. 00:27 And then with microangiopathies, remember, as the RBCs'a different cell? as it journey's through the blood vessel may then bump its head against the thrombi. 00:41 The head may then be sheared off forming something called schistocytes or helmet cells on peripheral blood smear. 00:50 So in addition to, obviously, issues with the platelet you're gonna find issues with hemolytic anemia as well. 00:57 Usually intravascular type, remember? With thrombotic microangiopathies take a look at the schistocytes here that we're looking at. 01:05 They look like sickle cells but be careful, the history here if the patient has let's say TTP, HUS or DIC which we'll talk about in great detail, then as the RBC's passing through the microvasculature may then form a helmet like structure. 01:20 Let's take a look at TTP. 01:24 Thrombotic thrombocytopenic purpura. 01:27 It is a genetic issue. 01:29 So what happens here is the fact that you formed a thrombi which means that the platelets are being consumed but now the problem is you don't have the proper cleaving mechanism intact. 01:42 So therefore, what TTP is an issue with the inhibition of what's known as your von Willebrand factor cleaving protease? In other words, the scissors that's supposed to cut the particular thrombi is no longer present so therefore, you're left with these thrombi'thrombotic. 02:08 Now that the thrombi is being formed you're now consuming a platelet therefore, the common discussion of thrombocytopenia and then purpura. 02:18 The particular gene that you must memorize called ADAMTS-13. 02:23 Please memorize ADAMTS-13. 02:26 It is that mutation in which the von Willebrand cleaving protease is inhibited. 02:32 Only in the idiopathic autoimmune form and then lack the enzyme active preventing breakdown of von Willebrand factor. 02:41 Once again, you can't get these huge von Willebrand multimers. 02:45 So now these multimers, what are they doing? Well, they're promoting what step in terms of platelet functioning? The adhesion. 02:54 You're focusing upon excessive adhesion to the endothelium and it's obviously is going to form tons of thrombi resulting in thrombocytopenia. 03:03 And tell me about those RBCs again please? Hmm, passing through and we form the schistocytes. 03:09 Microangiopathic hemolytic anemia. 03:12 With TTP, clinical pathology would include? Well, could be idiopathic. 03:17 We talked about mutations taking place with ADAMTS-13, secondary or acquired. 03:23 In other words, may be from cancer, pregnancy and such. 03:26 Maybe immunosuppressants, FK-506 is Tacrolimus, HIV perhaps or no ADAMTS-13 suppression. 03:37 TTP possible pathogenesis. 03:41 Inherited, Upshaw-Schulman syndrome. 03:46 Classic pentad of the following: Fever, thrombocytopenia because of thrombotic formation, microangiopathic hemolytic anemia'all things we've talked about? renal failure because of lack of blood flow to or through the renal vasculature and altered mental status because of, once again, lack of blood supply taking place up into the head. 04:10 It's the pentad most of these we've talked about due to the thrombi formation. 04:14 Inherited form which we then refer to as being Upshaw-Shulman syndrome. 04:20 If not properly treated then fatal. 04:24 Treatment'what are we trying to do? Well, we have to do plasma exchange so you got to remove the antibodies and, hopefully, you're trying to replenish? What was that called again? It's the protease that has been inhibited, correct? So the von Willebrand type of protease which was inhibited has to be properly replenished and maybe treated or managed with corticosteroids.
About the Lecture
The lecture Thrombotic Microangiopathies by Carlo Raj, MD is from the course Hemostasis: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is a typical finding in a blood smear from a patient with thrombotic microangiopathy?
- Schistocytes
- Hypochromic erythrocytes
- Cigar cells
- Spherocytes
- Howell–Jolly body
Which of the following cells most closely resembles a schistocyte?
- Sickle cell
- Neutrophil
- Eosinophil
- Basophil
- Spherocyte
Which of the following enzymes is mainly affected in thrombotic thrombocytopenic purpura (TTP) ?
- ADAMTS13
- Cyclooxygenase 1
- Cyclooxygenase 2
- Thromboxane-A synthase
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |