Playlist
Show Playlist
Hide Playlist
Tachycardia: Multifocal Atrial Tachycardia: Diagnosis and Treatment
-
Slides Tachyarrhythmia MultifocalAtrialTachycardia CardiovascularPathology.pdf
-
Download Lecture Overview
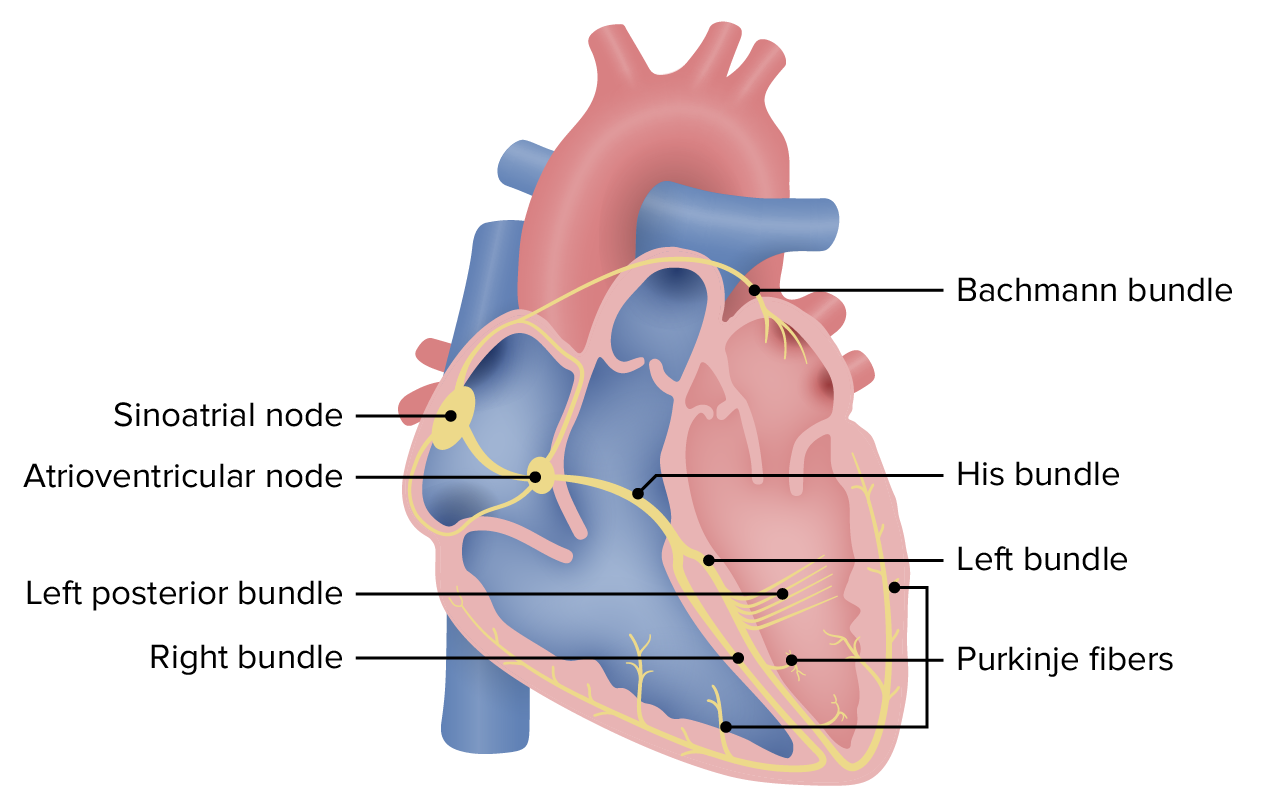
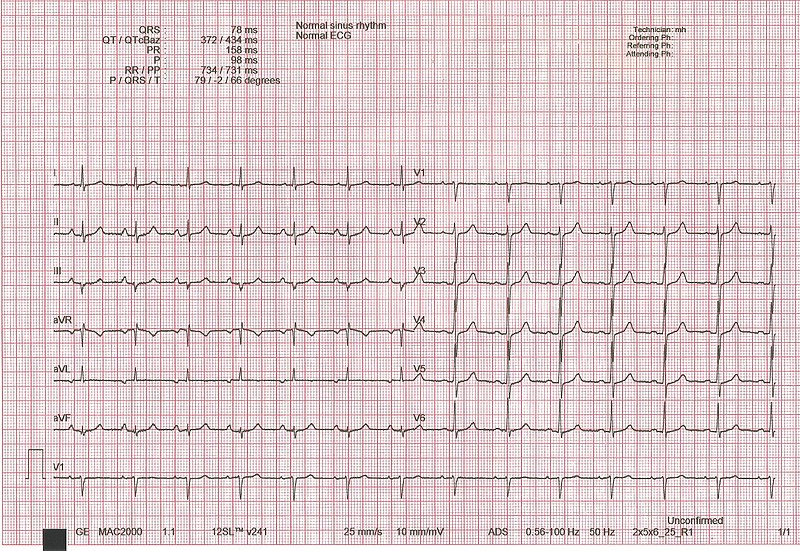
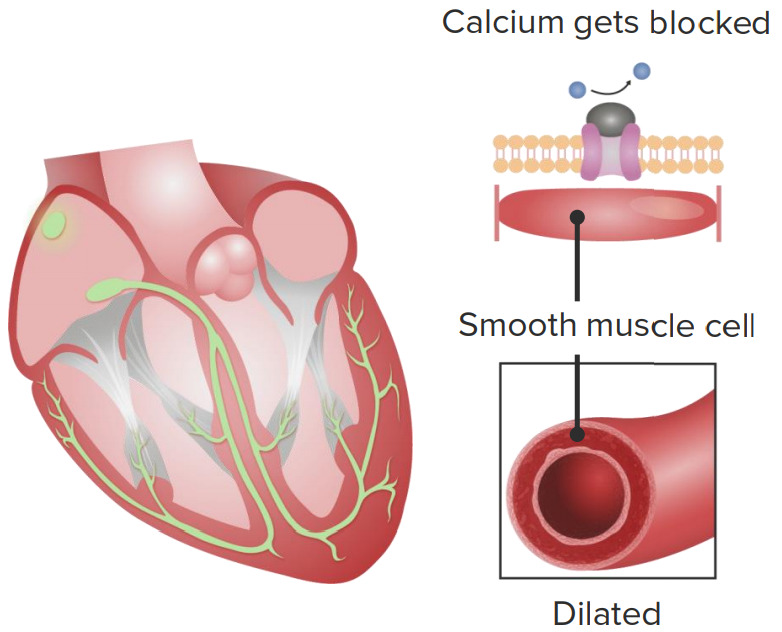
00:00 Now, couple of definitions have become important for us. We are tachy, so it has to be above 100. Put you in the cateogry. If it is less than 100 and the P wave looks abnormal and I will tell you what this abnormality of the P wave is in a second. Be careful because remember if you find the EKG and here we are going to push you a little bit, but you can handle it. If you take a look at an EKG, you are going to look for a P wave preceding the QRS complex, an upright QRS complex, especially lead II. 00:34 And then that gives you sinus type of rhythm. You take a look at the rate. Take a look at axis deviation and the P wave should be well as you would expect a P wave. However, when I show you the P wave upcoming, you will notice that the P wave is going to look rather dysmorphic. 00:55 Not fibrillated. Not fluttered meaning saw-tooth, but fibrillated or, in other words, it is wandering. It is going to look dysmorphic. If you find a dysmorphic type of P wave and if you find the heart rate to be almost within normal range, you will not call it multiatrial tachycardia, you will call it wandering atrial pacemaker and it really comes down to a simple definition such as less than 100 beats per minute. Next, what about the ECGs? We will see now we get into a dysmorphic or P waves in which its morphology has been altered. And when I it show to you, it would be quite obvious, but before we get there though, a couple of other definitions that you want to keep in mind. In one strip of EKG, on the same lead, you need to find at least three distinct P waves and by distinct I do not mean wave, like fibrilation. I do not mean two, like sawtooth. No. Three distinct each P wave looks a little bit more different than the other. So rather distinct in morphology of whom? The P wave. Do not touch the QRS complex because this is SVT. Hope that is clear. Spend a little bit of time with that last bullet point there because that really is going to be the description or the distinguishing point in words of an SVT known as multifocal atrial tachycardia. And then less than 100 beats per minute would be your wandering atrial pacemaker. What do you want to do? You'll correct the underlying issue, of verapamil now in terms of drugs up until now when we try to control that rhythm, we tried to cardiovert and we can do our cardioversion by medicine or medical cardioversion. And if that is not effective, your next step of management would have to be electrical cardioversion. Right? When we did our other SVTs including afib and atrial flutter, we tried to cardiovert medically and we did so by slowing things down. We did that by giving digoxin. We did that by giving metoprolol, a beta-blocker. Right? Now, verapamil, which is a calcium-channel blocker much more specific for the heart. Think V, verapamil; V, ventricle. 03:27 It slows down the heart rate or it tries to convert your abnormal distinct P wave into a proper normal sinus rhythm. Is that clear? Do you understand the concept of cardioversion now? Now if it is calcium-channel blocker, you try to control that heart rate. Well let me one more time bring this up and I am going to keep reinforcing this until you fully understand when we do pharmocologically with antiarrhythmics as to what you are dealing with. Earlier when we were talking about SVTs and I was talking to you about that phase 403 because we were talking about heart rate, which would be the pacemaker. That phase 4, which was funny with the sodium channel. I told you specifically that has to be ligand-gated, the only effective or should I say a more effective antiarrhythmic class that work on that phase 4 was that class II, which was a beta-blocker. "Dr. Raj, really it is not making sense. It is not sticking." It has already, believe it or not. When? When you did autonomic nervous system, when you did CNS physiology, you looked that the autonomic nervous system and you looked at the parasympethetic nervous system, how do you slow down that heart rate? Can you picture that? 403, parasympethetic, acetylcholine, working on antireceptors on the heart and how do you slow that heart rate? By causing a decreased gradient of phase 4. 04:53 Are you seeing this? And if you're not, listen to what I am saying. Go draw it out or go look at it where you take a look at your action potential and slowing down of your heart with parasympethetic and you worked through your phase 4. Is that clear? Acetylcholine, that has to be ligand-gated. Is that clear? That has to be cleared. Now that was when we were dealing with phase 4. Now let us talk about phase 0 of your pacemaker, heart rate. What is phase 0 as a pacemaker? You see how it is an integrating stuff. Stick with me. Phase 0 in a pacemaker potential is going to be your calcium channel. So, therefore, a drug or a class of antiarrhythmic that might have work here would be something like a calcium channel blocker. Let us continue. What are the drugs? Well. Beta-blockers to a certain extent could be used. Same concept. You are trying to slow down that heart rate. What phase? Phase 4. You know that. It decreases heart rate. And do not use dig in the treatment of MAT, though. That is important. Multifocal atrial tachycardia, there are too many other factors that are in play in which digoxin might actually not be effective. Keep that in mind whereas digoxin was a drug that you definitely thinking about using or considering when dealing with afib and atrial flutter. And that is another huge distinction point. 06:15 That last bullet point right there with digoxin. Hope that is clear. Let us continue. 06:21 So I want you to take a look at the bottom ECG lead and with that strip, you are paying attention to the P wave, does that look fibrillated to you? So what are you doing now? When you are going through these lecture series with SVTs, supraventricular tachycardia, is comparing atrial fibrillation, atrial flutter and now multifocal atrial tachycardia. Please do that for me. It is the best way to then identify each one. Is this the P wave is not fibrillated? It is definitely not saw-tooth and on the same lead, you will find three different rhythms in which the P wave is rather distinct, even within the same lead. This then gives you multifocal atrial tachycardia with a beat per minute or heart rate above 100, tachy. 07:13 If by chance it falls below 100, then you start thinking about the alternate diagnosis of wandering HO pacemaker. Let us continue.
About the Lecture
The lecture Tachycardia: Multifocal Atrial Tachycardia: Diagnosis and Treatment by Carlo Raj, MD is from the course Arrhythmias: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is true regarding multi-focal atrial tachycardia?
- A 12-lead ECG reveals multiple P wave morphologies.
- There is a regular rhythm with a 2:1 block.
- The heart rate is less than 100/minute.
- A widened QRS complex > 0.12 seconds is seen.
- A 12-lead ECG reveals similar P wave morphologies.
What is a difference seen on ECG between wandering atrial pacemaker (WAP) and multifocal atrial tachycardia (MAT)?
- WAP has a heart rate of < 100 bpm, and MAT has a heart rate of > 100 bpm.
- WAP has a heart rate of > 100 bpm, and MAT has a heart rate of < 100 bpm.
- WAP causes more symptoms than MAT.
- WAP is a type of AV nodal dysfunction.
- WAP may be differentiated by the morphology of the P wave.
Which of the following drugs is not recommended in multifocal atrial tachycardia?
- Digoxin
- Metoprolol
- Warfarin
- Verapamil
What type of ions are associated with phase 0 of the action potential in a cardiac pacemaker cell?
- Calcium ions
- Potassium ions
- Sodium ions
- Chloride ions
- Hydrogen ions
Which of the following phases of the pacemaker action potential is affected by beta-blockers?
- Phase 4
- Phase 1
- Phase 0
- Phase 3
- Phase 2
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |