Playlist
Show Playlist
Hide Playlist
Structure of the Glomerulus
-
Slides RenalClinicalAnatomy RenalPathology.pdf
-
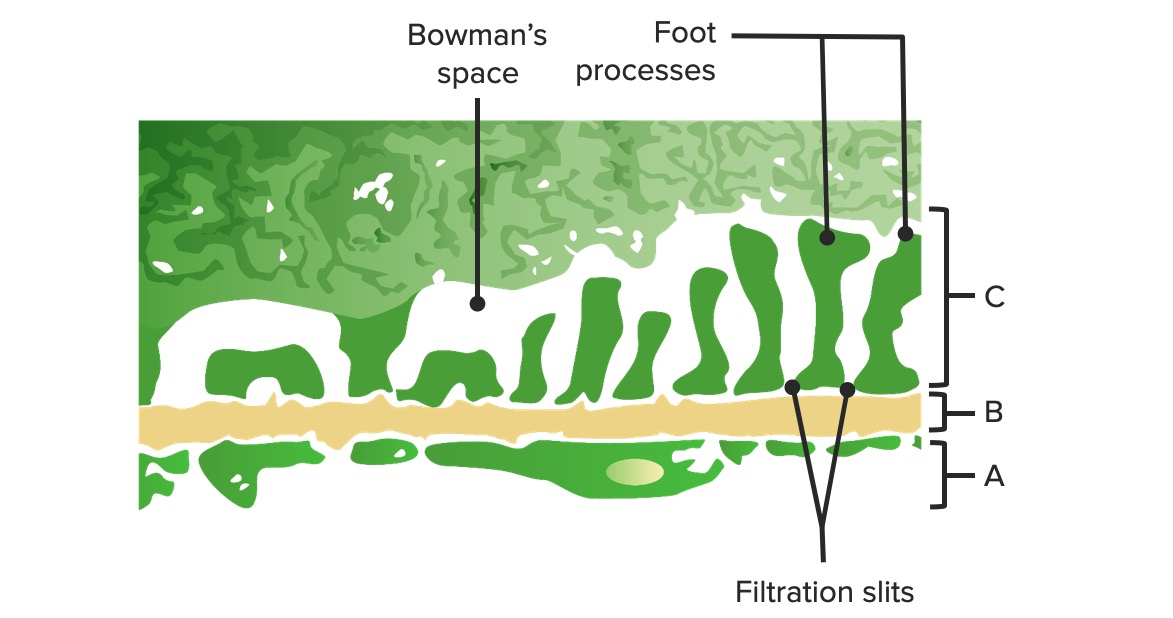
Download Lecture Overview
00:01 The structure of the glomerulus, we talked about the fenestrations. The fenestrations if it is on the side of the endothelial side well that allows for filtration to take place, these holes. If it is a glomerular basement membrane, what is the basement membrane always made up of? Four the floor, collagen type. Collagen type IV, collagen makes up the floor. 00:26 In other words basement membrane. Why is that important? You know pathology or you will know pathology in which that collagen type IV ends up being deficient, is that clear? Which one would that be? Something like output. You have heard of that before. An output syndrome you are literally missing type IV collagen. Obviously, we will discuss all this and I don't think we are going to have issues with the basement membrane of your kidney, but then you also have basement membrane issues in the ear, don't you? With output. Of course, you do. Kidney and deafness, that is output. Let's us continue. Size and charge we talked about earlier. What is the charge please at the basement membrane? Negative, has to be. 01:08 What is it that contributes to the negative charge? Called heparan sulfate. You noticed that I dramatically pronounced heparan and the reason for that, don't confuse this with heparin. 01:22 So heparan. Sometimes I just crack myself up just because of learning purposes. 01:25 But anyhow this is heparan sulfate, not the drug heparin. What does it do? It contributes to the negative charge. Let us continue. Cationic, protein, low molecular weight are permeable. 01:36 Is that clear? It has to be. You can get little proteins through there, but not large proteins like albumin. Next question obviously is going to be the following. 01:46 If by chance albumin does pass through the filtration barrier into the Bowman space, would you tell me what Starling's force has been affected? Question number 1. Oncotic pressure. 01:55 Good. Next, if oncotic pressure has been affected, is it increased or decreased into the Bowman space? Good. It is an increase in oncotic pressure. Good. And normally you shouldn't have oncotic pressure in your Bowman space. You see the terminology there. I was asking about the Bowman space and not the glomerular capillaries. Let us continue. 02:19 Structure. Albumin, strong negative, not permeable. Loss of the negative charge allows for maybe albumin to get through. Now what I need to be clear here as well is nephritic or nephrotic if there is glomerular damage, obviously, there would be. Then albumin would be passing through both the nephritic and nephrotic. But the abundance would be much greater in nephrotic. Hence, you will focus upon the letter O, and nephrotic referring to protein. 02:49 Well, selective proteinuria and that, of course, would be something like minimal change disease being the most common cause of nephrotic and glomerular nephritis in children. Glomerular basement membrane could be permeable to water. Why is it permeable to water? And as far as low molecular rate, hypertension, amino acids. Amino acids as you know can be filtered through, but not albumin. Causes of glomerular basement membrane, thickening is what the next step is and so close your eyes. I showed you on the previous discussion of electron microscopy with that glomerular basement membrane. It is thickened. How do that occur? Maybe it is immune complex deposition. And when you have immune complex deposition, it might either be underneath that epithelial cell. What is the name of that epithelial cell? A podocyte. 03:43 What kind of epithelial cell technically? A visceral epithelial cell. If it is underneath that epithelial cell, what is? An immune complex. Let me give you an example such as post-streptococcal glomerulonephritis secondary to perhaps a pharyngitis or maybe even a skin infection. 03:59 We've talked about all this, just process of reinforcement, but I need to give you a clear story as to what we are headed. Anyhow when you have post-streptococcal glomerulonephritis, you have these immune complexes that are then going to deposit where? Underneath the epithelial side. Epithelial, you call that subepithelial deposit. I will show you pictures. How else can you thicken your glomerular-based membrane? Literally collagen type IV ends up undergoing proliferation. Example, diabetes mellitus. Would you expect your type IV collagen to be thickened? Sure. Could you have involvement of mesangium? Sure. What is that called when you have light microscopy at diabetic nephropathy? It is called a Kimmelstiel-Wilson nodule. 04:46 I will show you pictures there as well. Says you can see here it is the clinical anatomy that you start off with being normal and then the physiology that we have talked about prior and then bit by bit by bit, we are going to stop plugging in our pathologies as we have been doing the entire time. 05:03 Let us talk about the podocyte, shall we? What does that call? A visceral epithelial cell. Close your eyes or go back to that picture of electron microscopy where you can clearly see that podocyte. That podocyte has foot processes. What about these foot processes? If they get fused, a couple of differentials. Couple? That was only one, Dr. Raj. No, they are a couple. The first major fusion of foot processes that you know is minimal change disease in that child. At some point in time, when our discussion takes us into focal segmental glomerulonephritis, could you perhaps find a fusion of your foot processes? Yes, you can. What if the foot process would become, the pores get larger in between the foot processes? That's you are thinking about along the lines of glomerulonephritis. The slit pore between the podocyte allow for passage of water and small amino acids, electrolytes serves as a distal barrier preventing protein loss in the urine. That is important. Fusion of foot processes could be seen in nephrotic syndrome such as minimal change disease. Let's talk about the mesangium. What does mesangium mean? You know that tissue in between the glomerular capillaries and the tuft of capillaries, all that tissue in the glomerulus. Think of this as being smooth muscle, please. This is called mesangium. The mesangium just like you would talk about any type of tissue in an organ, such as the interstitium. Here we will provide support to the structures surrounding the tissue. This would then include the glomerular capillaries. Mesangium can release inflammatory mediators and proliferate. This then brings us to once again the discussion of diabetic nephropathy. So apart from your glomerular basement membrane, which undergoes thickening, the mesangium could also get involved and forms that huge Kimmelstiel-Wilson nodule. In the mesangium, you could also deposit immunoglobulins pathologically. The most famous of them all would be IgA. So this then brings us to a diagnosis of IgA nephropathy. You might have heard of this in your medical education as Henoch-Schonlein purpura or you might have heard of this being Berger. What is the difference? You have think to yourself that both pathologies are involved with IgA? Sure. So what is the difference between Berger and Henoch-Schonlein purpura? Hence, nowadays, we have got rid of the eponym, the names per se, and we are strictly going into the pathology, which I love because then the pathology gives you exactly what you need to know for diagnosis without any confusion. But the difference is the following. When you have Henoch-Schonlein purpura, could you have IgA deposition in mesangium? Yes. If it is Henoch-Schonlein purpura, what does purpura represent? You have heard of palpable purpura and that palpable purpura is referring in the lower extremity, most likely a child, in the buttocks or in the lower extremity in which blood vessel undergoes inflammation and so therefore may result in a little bit of hemorrhage. That is called purpura, palpable. So Henoch-Schonlein purpura is referred to as IgA vasculopathy technically. Is that clear? In addition though, you could also have IgA deposition in your mesangium, that must be understood. We will talk about that again later reinforcement, but if it is strictly only IgA deposition in the mesangium of the kidney, without IgA deposition anywhere else. This is Berger. Hence, now we call this or have been calling this IgA nephropathy. Do you want to know that? Yes, you do. The most common worldwide glomerulonephritis is your IgA nephropathy. Let's move on. 09:04 We are going to the parietal cell. What does that mean to you? Parietal always means outer. 09:12 Visceral means inner. What was the other name or the most infamous name of the visceral epithelial cell? Well, it is more commonly called or popularly called your podocyte at your visceral? So which one is your parietal? Well, let me give you the example of your diagnosis. In that way you clearly see what the heck a parietal epithelial cell is. If you had a patient that has pharyngitis in a child that was inadequately treated, two to four weeks later ends up developing hematuria, and you would tell me at this point high in your differential would be post-streptococcal glomerulonephritis. 09:48 Oh! my goodness. Within 12 weeks, the kidney is dead. Twelve weeks is only three months. 09:57 That is not a chronic renal failure. It is not an acute renal failure. It is rapidly progressive glomerular nephritis. We will talk about this again. The reason I bring this up is the following. If you would take a look at light microscopy of your rapidly progressive glomerulonephritis, can you close your eyes or conceptualize to tell me as to what is proliferated within the glomerulus? You've heard of crescentic cell, haven't you? Thus crescentic cells are these, the parietal epithelial cells that are proliferating causing massive damage to the Bowman space. So it lines the Bowman's capsule. Imagine that proliferating. 10:36 You have obliterated the Bowman space. What happens to your kidney? Dead, really quick. 10:45 The proliferation causes crescents that encroach upon and destruction of the glomerulus. 10:49 How quickly can the kidneys die of RPGN? Within 12 weeks. That is not a lot of time. It is only about three months.
About the Lecture
The lecture Structure of the Glomerulus by Carlo Raj, MD is from the course Renal Clinical Anatomy.
Included Quiz Questions
What is the composition of the glomerular basement membrane?
- Type IV collagen
- Type III collagen
- Type II collagen
- Type I collagen
- Type V collagen
Which of the following conditions produces a significant amount of proteinuria?
- Nephrotic syndrome
- Nephritic syndrome
- Post-streptococcal glomerulonephritis
- Rapidly progressive glomerulonephritis
- Renal cell carcinoma
Which of the following produces the negative charge in the basement membrane of the glomerulus?
- Heparan sulfate
- Keratan sulfate
- Heparin sulfate
- Dermatan sulfate
- Glucagon sulfate
Which of the following represents the difference between Henoch-Schonlein purpura and Berger's disease?
- IgA vasculopathy in Henoch-Schonlein purpura
- IgA deposition in Henoch-Schonlein purpura
- IgA vasculopathy in Berger's disease
- IgA deposition in Berger's disease
- Type IV collagen deposition
What is the most common cause of nephrotic syndrome in children?
- Minimal change disease
- Membranous glomerulonephropathy
- Membranoproliferative glomerulonephropathy
- Post-streptococcal glomerulonephritis
- Focal segmental glomerulosclerosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |