Playlist
Show Playlist
Hide Playlist
Status Epilepticus: Evaluation, Prognosis, and Classification
-
Slides Seizures Epilepsy Status Epilepticus.pdf
-
Download Lecture Overview
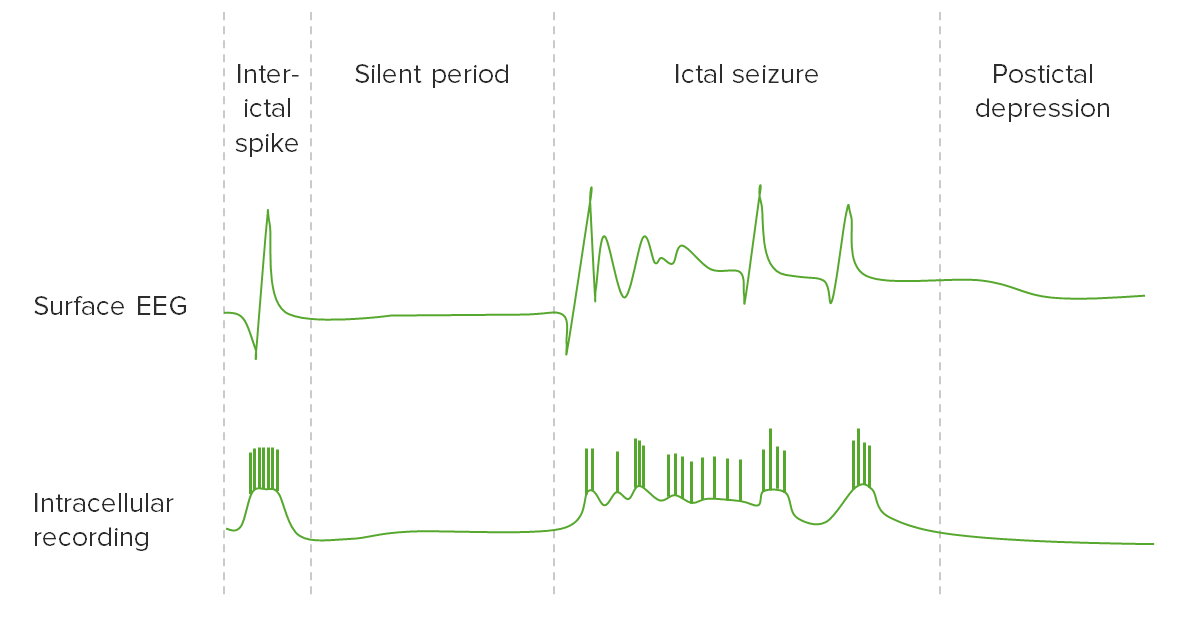
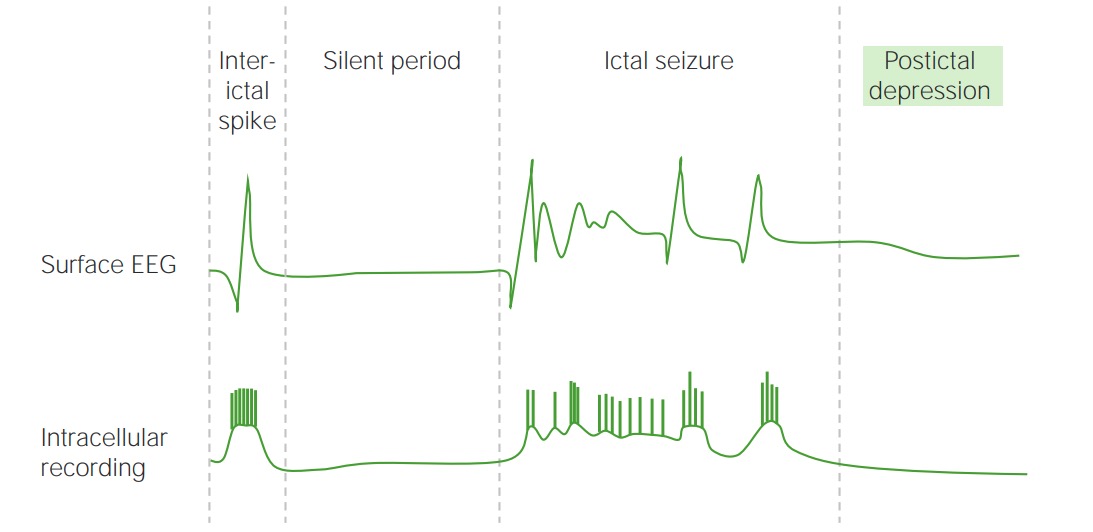
00:01 So let's talk more about status epilepticus and the evaluation of breakthrough seizures and continuous seizures. 00:08 When we're dealing with recurrence of a breakthrough seizure, a patient with epilepsy or with multiple seizures, who has a breakthrough seizure. 00:16 The first thing we need to think about is compliance, compliance, compliance. 00:21 The most common cause of a breakthrough seizure and that's a seizure that occurs in someone with known epilepsy is medication non-adherence. 00:28 There's many reasons not to be able to adhere to a medication. 00:31 It may have not been called in. 00:33 Patients may not be able to afford it. 00:35 They may be experiencing side effects. 00:37 And non-adherence inability to take the medication is the most common reason for a breakthrough seizure. 00:44 We also want to think for other potential exacerbating features. 00:48 Electrolyte abnormalities. 00:49 Infections can lower the seizure threshold and make it more likely for an epileptic patient to seize. 00:55 New medications that lower the seizure threshold like fluoroquinolones. 00:59 Sleep deprivation is one of the most common exacerbating conditions or other things that lower the seizure threshold. 01:08 We typically perform labs to evaluate for those electrolyte abnormalities or other potential causes of exacerbation of seizures. 01:15 But a CT of the head is not indicated unless the exam suggests or support some reason, some new focal neurologic deficit that indicates that we need imaging. 01:27 We typically think about titrating medications first and then think about changing additional agents. 01:32 So in epileptic patients who are on a seizure medicine, like the patient in our case, who was taking levetiracetam, we would increase the levetiracetam before adding additional medications when treating that patient for a breakthrough seizure. 01:48 The patient in our case was suffering from status epilepticus. 01:52 So let's spend some time learning about status. 01:55 And let's start with definitions and semiology. 01:58 The official definition of status epilepticus has been for years prolonged or recurrent seizures lasting at least 30 minutes. 02:07 That may be one seizure lasting at least 30 minutes, or multiple seizures without return to baseline lasting at least a 30 minute period of time. 02:15 But operationally, we know that epileptic seizures are rarely longer than five minutes. 02:21 And a seizure or multiple seizures lasting more than five minutes should raise early concern that we're dealing with status epilepticus. 02:30 We can classify status by the semiology. 02:33 Just like we do each individual seizure. 02:36 Convulsive status and that status then involves convulsion of the body tonic-clonic activity accounts for 77%, the majority of patients who suffer from status epilepticus. 02:48 We also see non-convulsive status. 02:50 That's continuous seizure activity without the motor convulsions. 02:54 This can be hard to diagnose, and more difficult to evaluate, and sometimes treat. 02:59 There are two types of non-convulsive status: Complex partial status. 03:04 And that status that hasn't evolved into that secondary generalized tonic-clonic seizure, but it is continuous. 03:09 And absence status, which is again a primary generalized epilepsy and multiple seizures without return to baseline would be consistent with absence status epilepticus. 03:21 And then lastly, we can see simple partial status epilepticus. 03:24 Those are those simple partial seizures that just continue repetitively. 03:29 Another name for this in the literature has been epilepsia partialis continua or continuous partial seizures. 03:36 This is rare in accounts for less than 10% of patients who present with status epilepticus. 03:44 In terms of some other information. 03:46 Etiology of seizures. 03:48 1 to 8 hospital admissions for epilepsy will be for status epilepticus, so we see it, it's rare, but it is an emergency. 03:56 Four to 16% of patients with epilepsy will have one episode of status epilepticus. 04:01 So up to 10% of our patients, one in 10 epileptic patients will develop status. 04:08 In children status epilepticus is most common in those that are younger than two years of age. 04:13 80% will present with febrile or acute symptomatic status epilepticus. 04:18 And so in these patients, we need to look for an underlying etiology. 04:22 And some of the things we think about would be fever or systemic infection that's causing status in a patient with underlying epilepsy. 04:29 A change in medication can result in the development of status and someone who previously had well controlled seizures. 04:35 Sometimes we don't find a cause. 04:37 Metabolic derangements, congenital abnormalities, anoxia. 04:42 CNS infections, trauma, strokes. 04:45 Other CNS insults, alcohol or drug intoxication, or new tumors can cause the development of status epilepticus in someone who previously had a diagnosis of epilepsy. 04:58 What about the prognosis? Convulsive status is a medical emergency. 05:03 This is one of the conditions in neurology, where we don't wait and watch. We intervene abruptly. 05:09 About 4% to 11% of children will die because of status epilepticus, And somewhere between 4 to up to 37% of adults in some reports will suffer death from status epilepticus. 05:21 What are the risk factors for death in status epilepticus? The underlying etiology is important and patients who suffer status from anoxia, cerebral anoxia, are at increased risk of death. 05:32 Patients at the extremities of age. 05:34 Very young neonates or the severe elderly are at higher risk of death from status epilepticus. 05:41 The duration of time is important. 05:43 Patients whose seizures are longer than an hour have a 32% risk of mortality compared to 2.7%, who seizures are stopped within an hour of their onset. 05:54 And inadequate treatment is important. 05:57 And this is why as you'll see, when we talk about treatment, we talked about early and acute quick intervention to stop the status or stop the seizure from where it started. 06:07 What do we see in the brain? Well, brain compensatory mechanisms begin to fail at about 30 minutes after continuous seizure. 06:16 And this is why that 30 minute mark is very important. 06:18 We want seizures to stop and we treat them to stop well before that period of time. 06:23 We see excitotoxicity with neural injury and cell death, especially in the hippocampus and amygdala for prolonged seizures greater than 30 minutes in duration. 06:35 Decreased brain oxygen tension, there can be a fall in cerebral blood flow, and depletion of brain glucose can all occur with prolonged seizure activity. 06:45 This is why we really treat these seizures aggressively and are looking to stop the status about as soon as it starts. 06:53 So in terms of classification, we can classify status epilepticus, both based on its initial presentation the semiology as well as response to treatment. 07:03 In terms of initial presentation, we can classify status as convulsive status, nonconvulsive status and simple partial status. 07:11 And in general, convulsive status is easier to treat than nonconvulsive status. 07:17 It's also easier to recognize. 07:19 patients who have motor jerking activity, we can recognize that as can caregivers. 07:24 Nonconvulsive status often has a delay to presentation or recognition. 07:29 Simple partial status epilepticus can be particularly difficult to treat. 07:33 And oftentimes, treating the underlying lesion finding a nidus, and treating that lesion can be important. 07:41 So for example, if the simple partial status is coming from a tumor, we need to diagnose the tumor and surgically remove it, and that can be much more effective than additional anti-epileptic drugs. 07:51 In addition, we can also categorize status epilepticus based on its response to treatment. 07:56 We'll talk about the treatment algorithm for status and it starts with initial anti-epileptic drugs. 08:03 Status that fails to respond to those initial interventions we call refractory status epilepticus. 08:09 Those patients are typically put in the ICU, and treated with a medically induced coma, to shut the brain down, turn the brain off, restart the brain to try and treat the status and prevent that seizure activity. 08:23 Patients who fail that intensive intravenous therapy are considered or categorized as having super-refractory status epilepticus. 08:32 And with each failed attempt at treatment, the status becomes more difficult to control. 08:38 So, this classification helps to orient us to the prognosis of the patient and how difficult their situation and condition may be to treat. 08:47 Looking at that classification system algorithmically, we see that convulsive status can be categorized as well as non-convulsive status. 08:56 For convulsive status it can be categorized as tonic clonic, or myoclonic. 09:01 And with non-convulsive status, it may be simple partial, complex partial, or absence status epilepticus. 09:08 The simple partial status manifests with based on the part of the brain that's involved. 09:13 So if the status is coming from the somatosensory cortex, it's a somatic sensory, simple partial status, or motor simple partial status, or in aphasic simple partial status. 09:25 What about convulsive versus non-convulsive status. 09:27 This is an important differentiator. 09:30 Convulsive status is more common. 09:31 It makes up 80 to 95% of patients with status epilepticus compared to nonconvulsive status around five to 20% of cases. 09:41 We can see varying degrees of convulsions. 09:43 And so some patients start with convulsive status, and then become subclinical status epilepticus. 09:49 They lose the motor activity. 09:51 We don't see clinical signs of status even though that EEG discharge has continued. 09:56 We can also see subtle motor findings myoclonic subtle myoclonus, or other subtle status epilepticus presentations. 10:04 Nonconvulsive status epilepticus can be categorized as absence status, which is a confusional state. 10:10 Often with eyelid myoclonus, or myoclonus of the face, or nystagmus, which we are clues to this diagnosis, or complex partial status epilepticus. 10:19 Again a confusional state that can wax and wane with motor automatisms and varying degrees of level of interactivity and awareness.
About the Lecture
The lecture Status Epilepticus: Evaluation, Prognosis, and Classification by Roy Strowd, MD is from the course Seizures and Epilepsy.
Included Quiz Questions
Which statement is the most accurate with regard to breakthrough seizures?
- Medication compliance is critical in preventing breakthrough seizures.
- Fevers are the most common cause of breakthrough seizures.
- A head CT is necessary after every breakthrough seizure to look for a potential nidus.
- Routine labs should be avoided following a breakthrough seizure.
- Changing the patient’s medication regimen is the first step of treatment.
Which statement is the medical definition of status epilepticus?
- A prolonged or recurrent seizure lasting longer than 30 minutes.
- Any convulsive episode that does not respond to treatment.
- Any seizure that does not resolve spontaneously in under 5 minutes.
- A prolonged seizure lasting more than 1 hour.
- Any seizure that causes lasting brain damage or death.
Which statement regarding the epidemiology of status epilepticus (SE) is the most accurate?
- It usually presents as a febrile illness in young children.
- It accounts for 20% of all hospital admissions.
- Most patients with epilepsy will have at least one episode of SE.
- SE is more common in children over the age of 8 years.
- Most cases of SE present without convulsions.
Which statement is the most accurate regarding the prognosis of status epilepticus (SE)?
- Mortality is significantly higher if the episode lasts longer than 1 hour.
- It is a medical emergency with a mortality rate higher than 50% in children.
- The mortality in adults is lower than that in children.
- The underlying etiology does not impact mortality.
- Advanced age is protective in terms of mortality.
Which statement is the most accurate when discussing the classification and treatment options of status epilepticus (SE)?
- Refractory SE is a term used when a patient does not respond to antiepileptic drugs.
- Convulsive SE is harder to treat than non-convulsive SE.
- Non-convulsive SE is usually easy to recognize.
- Patients with super-refractory SE are treated effectively by a medically induced coma.
- Patients with refractory or super-refractory SE generally become more responsive to treatment with each episode.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |