Playlist
Show Playlist
Hide Playlist
Sialolithiasis
-
Slides GIP Sialolithiasis.pdf
-
Download Lecture Overview
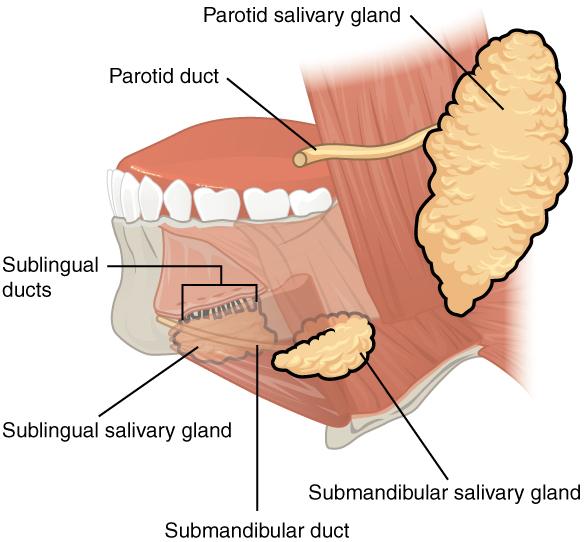
00:01 Welcome. In this talk, we're going to discuss Sialolithiasis. 00:05 Sialo, the root word meaning salivary gland. Lithiasis meaning stone. 00:10 So now, you know this is going to be about stones in the salivary gland. 00:15 Doesn't sound very pleasant. 00:16 So Sialolithiasis is the formation of calculi, a stone within the salivary glands or the ducts. 00:23 Epidemiology of this. An estimated incidence of about 0.3 to 1 in 10,000 people, so not super common but not all that uncommon either. 00:35 And for reasons we'll discuss in a minute, more likely to occur in men than in women. 00:41 But clearly, women can get this. 00:43 The typical age range is between 30 to 60 years but clearly, kids can get this depending on other pathologies and certainly, geriatrics can get it as well. 00:52 So let's talk about pathophysiology. 00:55 We're looking here at the three main salivary glands. 00:58 The parotid gland, up in the cheek, the submandibular gland at the angle of the jaw and the sublingual gland that sits underneath the tongue. 01:05 For reasons that I don't completely understand, about 80% of stones will occur in the submandibular glands involving the duct that drains into the mouth that is Wharton's duct. 01:18 So as part of the pathophysiology, we have to understand what's in spit, what's in saliva. 01:25 It's a number of things that are there to both kind of lubricate food as we ingest it but also to start the digestive process and to protect against all of the bacteria that are in the mouth. 01:38 It's a fairly nasty place if you think about it. 01:41 Anyway, the other components within spit or saliva is going to be water, electrolytes, sodium, chloride, calcium, etc. 01:50 There's going to be mucus. That's going to be part of the lubrication process. 01:53 There are going to be a variety of proteins including Amylase which is important for the beginning the digestive process. 01:59 There are going to be immunoglobulins. 02:01 That's going to be bacteriostatic that's going to prevent some infections and there are going to be a variety of other proteins that keep the bacterial count way down, bactericidal proteins. 02:11 With the formation of stones, we have mostly inorganic materials So there's a little bit of protein in there, there's a little bit of mucus, but it's mostly calcium and other inorganic compounds. 02:25 And you see it forming there within the duct. Why does this happen? Well, one is that you just don't have enough salivary flow. 02:34 So if you don't have constant flow, you can get desiccation. 02:38 You can get drying out of the secretions within the duct. 02:42 So you want to have a lot of good salivary flow all the time. 02:44 There may be an anatomical duct stenosis just the way you were born and it's partially occluded. 02:51 There may be inflammation that's there. 02:54 And we'll talk about some of the inflammatory disorders that can affect the salivary gland and/or the salivary ducts. 03:00 It just may mean that you're dehydrated. 03:03 You're not able to salivate, make saliva, spit because you are dry. 03:09 That can go along with anorexia, just not taking adequate fluid intake. 03:13 There may be allergies that cause then a reduction in the amount of salivary flow and certain medications can clearly do this. 03:23 Or you may have increased alkaline viscous and mucus-rich saliva that will impede the normal flow. If you don't have nice, watery spit. 03:32 Then, that slow viscous material is more prone to forming stones, in particularly, there will be deposition of calcium phosphate. 03:42 So how does this present? Well, you may or may not have some degree of glandular swelling. 03:49 That's because the duct is obstructed with a stone and the salivary gland is trying to make fluid and it can't get out. 03:56 So you may have swelling that's associated with that even without necessarily having inflammation. 04:01 So you may not have pain and tenderness. 04:03 But when pain and tenderness occurs, that means that the salivary gland itself is inflamed. 04:09 Frequently the pain is worse with eating. Why would that happen? Well, because when you eat, you salivate more. 04:18 And if there's an obstruction, clearly, all that stuff is backing up behind the point of obstruction. 04:23 You may also feel the presence of the calculus, either with your tongue or what's indicated here, a digital palpation, literally, put your finger in there and kind of root around you. 04:34 It's like, “Uh, it feels like there's a rock.” There will be increased dental carries, the teeth are starting to rot. Why is that happening? It's because you're not getting the normal saliva with all those bactericidal proteins and things in it. 04:50 So you're going to get more cavities as a result of that if you have chronic obstruction. 04:55 That's your clinical presentation. What about a diagnosis? So usually, you can either feel the stone or you can have some of the other kind of manifestations as swelling, pain when you eat, etc. 05:09 Or you can confirm it with x-rays, or ultrasound, or CT, or sialography. 05:15 In this particular case, we're looking at an x-ray. 05:17 This calcium-rich stone is like, don't even need the arrow. 05:20 You can see it right there. How do we manage this? So, hydrate. More saliva, you'll get better flow. 05:28 You will also dilute out those inorganic compounds that are more likely to form the stone. 05:33 Hot compresses by causing dilation of the salivary duct will help and help to pass any stone that might be there. 05:40 You can physically massage the gland and try to move things through. 05:45 Clearly, you want to treat pain. 05:48 So you'll give non-steroidal anti-inflammatory agents. 05:51 Sialagogues. What's that? It's just something to increase salivation. 05:55 And so peppermint oil is something that's frequently administered. 05:59 In those cases where you can't get the stone to move on its own, you may have to actually go in and take it out. 06:08 You can do a manual expression. In many cases, you can compress and pop it out. 06:11 You can actually go in with an endoscope and snare it or you may use ultrasound from the outside. 06:18 And do Lithotripsy where you are fragmenting the stone into little bits that can more easily flow out.
About the Lecture
The lecture Sialolithiasis by Richard Mitchell, MD, PhD is from the course Disorders of the Oral Cavity and Salivary Glands.
Included Quiz Questions
What is the most accurate definition of sialolithiasis?
- Salivary gland stone
- Salivary gland obstruction
- Gastrointestinal obstruction
- Gastrointestinal stone
- Kidney stone
What is not a pathologic mechanism of sialolithiasis?
- Decreased alkaline viscous saliva
- Stagnant salivary flow
- Duct stenosis
- Dehydration
- Inflammation
What is a possible symptom of salivary gland inflammation?
- Pain with eating
- Weight gain
- Rib pain
- Loose stools
- Dizziness
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |