Playlist
Show Playlist
Hide Playlist
Second Seizure: History and Forms of Screening
-
Slides Seizures Epilepsy New Onset Seizure.pdf
-
Download Lecture Overview
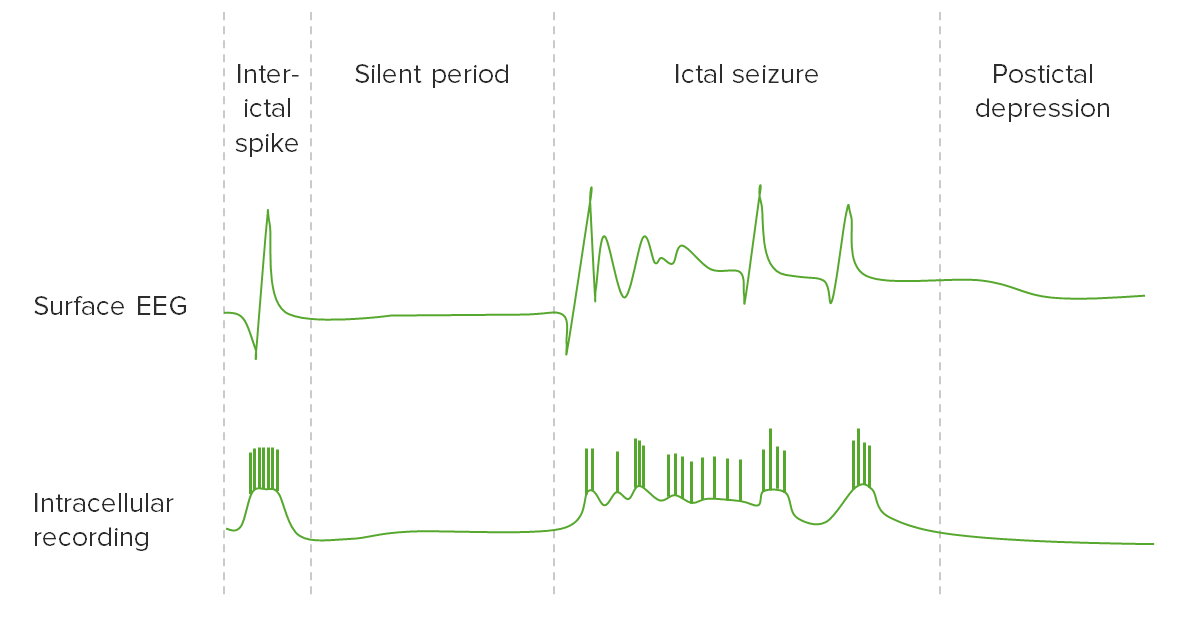
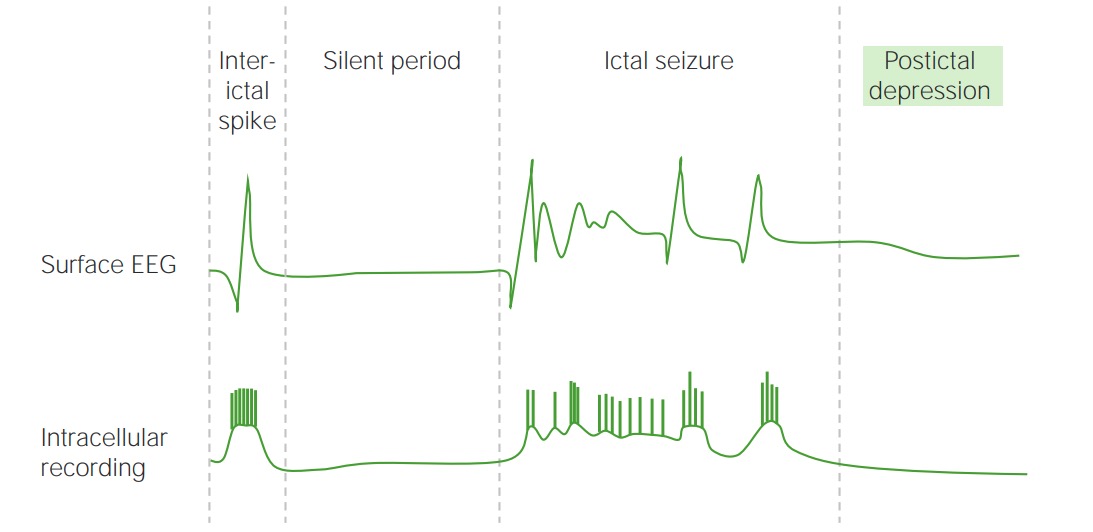
00:01 In terms of the risk of second seizure, when we're looking at the history, we're looking for findings that point us towards a higher or lower risk of developing a second seizure. 00:11 The risk of second seizure after a focal seizure is about 60%. 00:15 compared to 40% for generalized onset seizures. 00:18 Some generalized onset seizures can be induced by hypoglycemia, or hyponatremia, or hypercalcemia, or other electrolyte or medication, inciting factors. 00:29 And so focal onset seizures should raise our suspicion for a risk of a second seizure. 00:33 Seizures that occur out of sleep have a higher risk of patients suffering a second seizure 60% compared to those out of wakefulness 35%. 00:42 So we never want to ignore the risk of a nocturnal onset, new first time seizure. 00:47 Of those with a second seizure 73% will occur in the same state. 00:52 So the state of the first seizure really tells us when we should be concerned and help with counseling patients. 00:58 Frontal lobe seizures are important. 00:59 They can look very uncommon and present very uncommonly. 01:03 They can occur out of sleep or in the early morning. 01:06 Patients often have bizarre behavior. 01:09 Frequently with retained awareness, many patients are aware during their frontal seizure, with altered behavior, or even psychogenic behaviors that can mimic a psychogenic spell. 01:20 Those seizures that occur out of sleep, particularly where we're concerned about a frontal lobe origin those patients should undergo full evaluation. 01:28 And we should never discount a spell out of sleep. 01:33 When we're thinking about the studies that we perform for a patient with the first time seizure, EKG is important to look for cardiac abnormalities. 01:40 electrolytes in a urine drug screen, to look for potential exacerbates for seizure. 01:45 A sepsis evaluation may be needed if we're concerned for risk of infection or a lumbar puncture if meningitis is a possibility. 01:52 Head CT is typically done to look for abnormal findings that could suggest nidus for seizure. 01:58 and particularly in patients with an abnormal neurologic exam, a focal onset seizure where we need to look for a mass lesion or other predisposing history. 02:06 History of stroke or traumatic brain injury. 02:09 Outside of the emergency department we think about other studies. 02:13 Most patients undergo an EEG, a brain MRI, sometimes will consider tilt table test if we're worried about convulsive syncope and prolonged EEG, either ambulatory EEG in the outpatient setting or admission to the hospital to an Epilepsy Monitoring Unit. 02:28 Maybe you needed to characterize what happens on the EEG during the event and differentiate between an epileptic origin or a non-epileptic origin. 02:39 When we're looking at the EEG, the goals of the EEG are to observe interictal epileptiform abnormalities. 02:44 Those are epileptiform discharges spikes that occur in between episodes and suggest a reduced seizure threshold or a focal origin of the epileptic events. 02:55 They we're looking for focal sharp waves that spike and wave that indicates an area of the brain that is at risk to cease. 03:02 We also would like to observe any ictal or interictal patterns that would correspond to a known seizure syndrome or an epilepsy syndrome. 03:10 There are certain findings on the EEG and the one to think about is a 3 Hz spike and wave finding that we see with absence epilepsy. 03:18 That 3 Hz spike and wave is seen both ictally and interictally. 03:22 And it points towards a diagnosis of absence epilepsy. 03:25 So we're also looking for those characteristic findings on the EEG. 03:31 So what are we looking for on the EEG after a first time seizure? Well, we're looking for interictal findings that may classify the seizure type and help us determine that treatment. 03:42 There are certain specific interictal EEG patterns that can lead to a precise diagnosis. 03:46 A 3 Hz spike and wave points to absence epilepsy. 03:50 A 4 Hz spike and wave points to juvenile myoclonic epilepsy. 03:55 In rolandic epilepsy, we see centrotemporal spikes. 03:57 Infantile spasms, hypsarrhythmia. 04:00 With Angelman syndrome, we can see notched to delta waves. 04:03 In myoclonic epilepsies, have a photo convulsive response, where presentation of a photic stimulus and repeated photic stimulus drives a convulsive response either clinically or on the EEG. 04:16 We don't need to know all of these patterns specifically, but that we're looking for specific interictal patterns on the EEG that point us to a diagnosis and can help select a treatment. 04:28 In addition, we're also looking for the non-specific interictal EEG findings. 04:32 The spikes in waves that we may see at a focus interictally that would point us to a risk of seizure. 04:42 So let's talk a little bit more about epileptiform discharges, those spike and waves that we see on the EEG. 04:47 Interictal epileptiform discharges are observed in normal patients who don't have epilepsy, as well as those with epilepsy. 04:55 We see them in about 2% to 4% of children, and less than 1% of adults. 05:00 Normally, in the normal general population. 05:04 Up to 12% of patients with neurologic disease with and without epilepsy will have epileptiform discharges. 05:11 We can see them in dementia, or Parkinson's disease, and other conditions like stroke. 05:16 And in those conditions an epileptiform discharge does not mean that the patient will have a seizure, but is it slightly higher risk. 05:23 And then around 30% to 55% of patients on the initial EEG, and up to 80% to 90% of patients on serial EEG's will have epileptiform discharges for those who have seizures. 05:36 Three 30 minute routine EEGs, three 30 minute interictal EEGs are sufficient to capture 80% to 90% of seizure patients who will have an epileptiform discharges. 05:49 So in conclusion, normal patients can have an abnormal EEG. 05:53 And patients with epilepsy can also have a normal EEG but three 30 minute EEGs. 06:00 If normal, start to draw a question as to whether this patient does have an increased seizure risk? So let's talk a little bit more about the risk of a second seizure. 06:11 The point of an EEG after a first time seizure, the goal of the EEG after a first time seizure is to evaluate the risk of a second seizure. 06:20 If interictal epileptiform discharges are observed on the initial EEG, then the risk of the recurrence of recurrent seizures higher. 06:28 The general risk of seizure with an abnormal EEG is about 50%. 06:34 With a normal EEG, it's down to 25%. 06:37 So a normal EEG after a first time seizure is reassuring, and we would not start the patient on treatment. 06:43 An abnormal EEG raises that risk. 06:46 And we may consider treatment in the appropriate clinical setting. 06:51 Importantly, EEG is performed within the first 24 hours of a seizure are higher yield. 06:56 There's a 51% chance of finding those abnormal epileptiform discharges. 07:00 So we like to do them early. 07:02 And EEG is performed after the 24 hour period, after that first time seizure. 07:07 The chance of finding abnormal epileptiform discharges goes down to 34%. 07:12 So if we're going to do the EEG, we like to do it early. 07:15 And if abnormal, it would raise our suspicion for risk of a second seizure. 07:21 So let's talk about the role of neuroimaging and evaluating the first time seizure. 07:25 There's a few things we need to know. 07:27 First of all, all patients with the first time seizures should get imaging. 07:31 Second, we see both CT and MRI performed. 07:35 There are some nuances to that. 07:36 but what I want you to take away is neuroimaging should be done. 07:40 If we look at the AAN practice guideline, it does not differentiate between CT or MRI. 07:46 Both are okay. 07:47 Though there are some studies that have favored MRI over CT. 07:51 An interesting study looked at the expertise of the radiologist showed that the sensitivity of finding an abnormal lesion for non-expert radiologists was about 40%, for expert radiologists 50%, and the sensitivity for an epilepsy radiology expert was up to 91%. 08:09 So the data here is a little confusing. 08:11 The key is that MRI is helpful. CT is probably just as good. 08:16 And you'll see both of these performed in patients with first time seizures. 08:20 The chance of seeing an epileptic focus on the MRI varies. 08:25 Overall, we see about 30% of first time seizure patients present with an abnormality on their MRI. 08:32 If the CT is normal, 15% of patients will still have an abnormality on the MRI. 08:37 And this is why sometimes in patients where we're have a strong suspicion for an underlying lesion, a normal CT scan won't make us feel comfortable. 08:46 And we will still consider an MRI for those patients. 08:50 And those patients we're looking for things like mesial temporal sclerosis, a post-traumatic focus, or a rare cortical dysplasia that could be missed on the CT scan. 09:00 A lot of things can be seen on MRI that may drive seizures. 09:03 In this study of patients who presented with a new-onset first time seizure 30% of patients had an underlying focus on imaging. 09:12 And if all those findings, we saw a varying range of diagnoses. 09:18 Strokes were seen in a third of patients who had an abnormal MRI. 09:22 We saw post-traumatic lesions in about a fifth of patients. 09:25 Mesial temporal sclerosis in 6% of patients with an abnormal MRI. 09:30 Neoplastic lesions can be seen and more common in patients as they age. 09:35 Cortical dysplasias are uncommon, but a very important potential nidus for seizure that can be missed with an untrained eye on the MRI. 09:44 Cavernomas or vascular lesions, other vascular malformations, perinatal insults, and other findings. 09:50 So many things can be seen on the MRI and about 30% of patients will have an abnormal MRI when presenting with a first time seizure. 09:59 I think the key things to remember about neuroimaging is we're using neuroimaging to differentiate the risk of a second seizure. 10:06 We're using it to evaluate those patients who are at low risk of a second seizure, and we won't initiate treatment or high risk of a second seizure. 10:13 And we may consider treatment earlier for those patients. 10:17 If we look at the risk of a second seizure at one year, after first time presentation with a normal CT or MRI, it's about 40%. 10:25 So less than 50%. 10:27 With an abnormal MRI, with an epileptogenic lesion on the CT or MRI, that goes up to 60%. 10:33 So again, when we find those abnormalities on imaging, we would favor treatment or earlier treatment in some of those patients because of the higher risk of a second seizure.
About the Lecture
The lecture Second Seizure: History and Forms of Screening by Roy Strowd, MD is from the course Seizures and Epilepsy.
Included Quiz Questions
Which statement is the most accurate with respect to the risk of a second seizure?
- After a focal-onset seizure, a patient has a 60% risk of recurrence.
- A generalized seizure has a greater risk of recurrence than a focal-onset seizure.
- Seizures occurring during sleep have a lower risk of recurrence than those occurring while awake.
- After experiencing a nocturnal seizure, a subsequent seizure is most likely to occur during the day.
- Patients experiencing bizarre nocturnal behaviors should be reassured that recurrence is unlikely.
Upon presentation to the ED for a seizure, which test is likely to be deferred to the outpatient setting?
- EEG
- ECG
- Blood work
- Toxicology screening
- Head CT
Which statement is the most accurate with regard to an EEG in an outpatient setting?
- An EEG can determine specific epileptiform patterns and non-specific paroxysmal depolarization shifts.
- Epileptiform discharges do not occur in healthy adults or children.
- Having a neurological disease does not change the likelihood of epileptiform discharges.
- Compared with a single EEG, a serial EEG decreases the diagnostic sensitivity of the study.
- The time elapsed between a seizure and the initial EEG does not impact sensitivity.
Which statement is the most accurate with regard to neuroimaging when diagnosing a seizure?
- All patients with a first-time seizure should undergo a CT or MRI.
- MRI and CT have equal sensitivity in determining the epileptic focus.
- After a first-time seizure, an MRI has almost a 75% success rate in determining the epileptic focus.
- If the CT is negative, a seizure focal point should be ruled out regardless of suspicion.
- Neuroimaging is used to guide treatment options, but it cannot predict recurrence risk.
Which statement is the most accurate when discussing recurrence risk after the first seizure?
- Overall, a patient with a normal MRI has a 40% chance of seizure recurrence.
- An abnormal EEG after the first seizure suggests a 90% chance of recurrence.
- A negative EEG after a seizure suggests a recurrence risk of < 5%.
- An epileptogenic lesion on MRI after the first seizure indicates an 80% risk of recurrence.
- EEG does not predict recurrence risk.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |