Playlist
Show Playlist
Hide Playlist
Scleroderma
-
Slides ConnectiveTissueDisease RespiratoryPathology.pdf
-
Download Lecture Overview
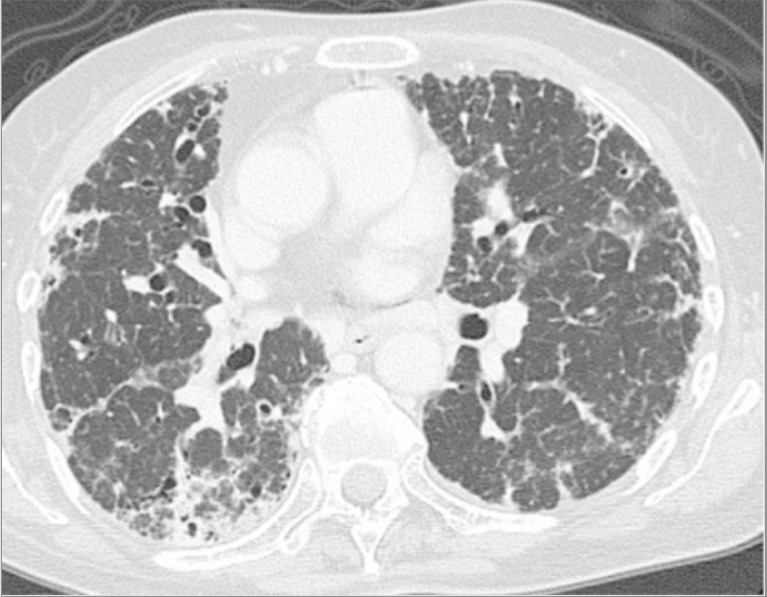
00:00 Now scleroderma. 00:02 Obviously scleroderma itself, the first description that should come to mind is automatically, reflexively, Oh, Fibrosis. 00:09 Where is the fibrosis that you might find? Well, here there might be two manifestations And by that mean there might be two method by which scleroderma is developing in your patient. 00:20 It might be the cutaneous type. 00:22 And if it's the cutaneous type of manifestation, then there's going to be excess deposition of collagen , fibrosis on the skin - cutaneous. 00:32 Whereas if there's skin and an organ to be affected, then that is going to be more of your systemic type of issue Is that clear? It is that black and white when dealing with scleroderma. 00:43 At some point, when you have reviewed your connective tissue diseases, and we discuss our sclerodermas, then we'll take a look at particular markers that are important for you. 00:53 For example, let me show you the one that you all know so very well which is CREST, right? CREST Syndrome. 00:59 C-calcinosis, R-Raynaud's, E-esophageal dysmotility, S-sclerodactyly, T-telangiectasia Now if it is esophageal dysmotility that you find with scleroderma, read the first statement here, then you can imagine that your patient most likely would be suffering from Well, what if your patient now has fever, and also has come back to be positive for anti-centromere? that fever and the type of lung issue that you might find in this patient would be aspiration pneumonia. 01:31 I need you to be very clear and understand the, well the pathogenesis of how the lung is being damaged This will be aspiration pneumonia. 01:41 Whereas if there was fibrosis that's taking place, of the lung Oh, maybe there wasn't much, initially. 01:47 and so therefore it might have been nonspecific. 01:49 Uh oh, there's quite a bit of fibrosis taking place in lung You see "honeycomb appearance" on your chest x-ray, Oh my goodness, this is idiopathic pulmonary fibrosis. 02:00 Do you understand? Just by looking at scleroderma and you're walking through CREST, And you're affecting the esophagus, you have answered choices, and you missed and all that you've memorized is scleroderma and fibrosis, and you're not thinking things clearly, because it's a long clinical vignette and you're tired, Well there's every possibility that you missed that your patient might have been suffering from esophageal dysmotility from scleroderma therefore the lung lesion here would be more of the aspiration type. 02:31 Are we clear? I hope so. 02:33 Now, diffuse interstitial disease or alveolitis seen in patients with systemic disease more frequently than those with CREST. 02:43 Once again, that is, that's a huge statement. 02:46 Understand the difference. 02:47 There are two different patterns of scleroderma. 02:50 One of these is systemic disease, what does that mean? Could the skin be involved? Absolutely. 02:55 In addition, what else is being involved? An organ. Now severe organ. 02:59 So in this case, we're talking about the lung so therefore it will be diffuse interstitial disease, so will be quite a bit of fibrosis. 03:06 Whereas if it was CREST, you pay attention to E - esophageal dysmotility and what's causing lung damage? Good, aspiration pneumonia. 03:15 CREST patients are more likely to have pulmonary hypertension, and so therefore look for issues within the right ventricle Alright so that's important for you to pay attention to - the two patterns.
About the Lecture
The lecture Scleroderma by Carlo Raj, MD is from the course Restrictive Lung Disease.
Included Quiz Questions
Which statement is correct?
- Diffuse interstitial disease is seen more frequently in patients with systemic disease.
- Diffuse interstitial disease is seen more frequently in patients with CREST.
- Focal interstitial disease is seen more frequently in patients with systemic disease.
- Focal interstitial disease is seen more frequently in patients with CREST.
- Diffuse interstitial disease is not seen in patients with systemic disease.
Why is aspiration pneumonia likely in patients with scleroderma?
- Esophageal dysmotility
- Dietary habits
- Vocal cord paralysis
- Hyperplasia of the buccal mucosa
- Immunocompromise
Which of the following pulmonary manifestations is commonly found in patients with CREST syndrome?
- Pulmonary hypertension
- Usual interstitial pneumonia
- COPD
- Spontaneous pneumothorax
- Pleural effusion
What is the most likely disease complication in a patient with shortness of breath, positive anti-centromere antibodies, and prominent esophageal dysmotility?
- Aspiration pneumonia
- Community acquired pneumonia
- COPD
- Bronchitis
- Bronchiolitis obliterans
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |