Playlist
Show Playlist
Hide Playlist
Rheumatoid Arthritis (RA): Signs and Symptoms
-
Rheumatology I 03 Connective Tissue Diseases.pdf
-
Download Lecture Overview
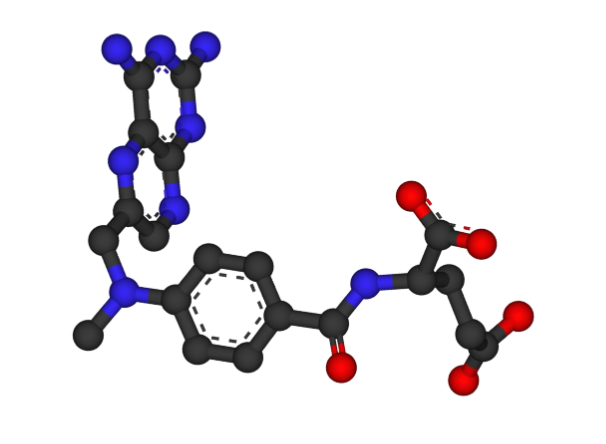
00:01 Signs and symptoms, polyarticular, symmetrical, we’ve talked about. 00:05 Active synovitis we talked about and I showed you that you would have tons of synovial fluid or reddening, and if you touch the metacarpal phalangeal, you know what it feels like? Spongey, okay? Like it’s spongey, filled with fluid, synovial fluid. 00:22 The patient’s complain of morning stiffness. 00:24 This is incredibly important, let me stop here for one second. 00:27 In osteoarthritis, a 72-year-old male shall we say or to make it more common, a 72-year-old female in osteoarthritis. 00:38 She wakes up in the morning and she’s complaining of, “Doc, I’m having a hard time moving my knees.” “How long before you can actually move them?” “About 25 minutes.” This is not rheumatoid arthritis. 00:52 This is not rheumatoid arthritis, that’s osteoarthritis and you go on to ask about that pain and the joints and such, and she says, “The more weight that I try to put on there, doc, it hurts more, and more, and more.” That’s osteoarthritis. 01:09 Here, rheumatoid arthritis, the pain of the morning stiffness lasts greater than one hour. 01:15 That is probably one of the most important and significant histories that you’ll be taking from this patient in any way, shape, or form, they have to give that to you. 01:25 Also, with rheumatoid arthritis is when the patient starts moving is when the patient says, “I want to keep going, because if I stop, then the stiffness comes back and that is just very inconvenient, doc.” The patients have involvement of multiple joints. 01:46 I gave you so for metacarpal phalangeal, I gave you so for the PIP, rarely ever the DIP, maybe the knee. 01:54 The wrists, MCP, and PIPs are commonly involved. 01:58 The joints are involved in a symmetrical fashion. 02:00 The patients may develop rheumatoid nodules, what are those? The fibrinoid necrosis and you have the histiocytes that are arranged in pulsating pattern. 02:08 Rheumatoid factor positive patients is usually when you’ll find rheumatoid nodules. 02:13 Now, the synovium is often affected. 02:16 Some may result in tendons involvement called tenosynovium causing carpal tunnel syndrome, keep that in mind or rotator cuff tendonitis is all due to synovium. 02:33 In other words, you’re thinking about shoulders, you’re thinking about the knee, maybe you’re thinking about the carpal tunnel issue by the wrist. 02:39 As the disease progresses, destruction will continue to become worse. 02:45 You’ll have ulnar deviation. 02:48 The fingers are moving in the ulnar region or excuse me, within the ulnar direction. 02:54 You’ll have swan-neck deformity of the fingers. 02:57 I’ll show you a picture coming up. 02:58 You will have, now picture the following, the DIP becomes hyperextended. 03:06 I’ll try to do this as best as I can. 03:09 And then, the PIP then becomes hyper flexed. 03:14 It’s the extensive flexion of the PIP and extensive extension of the DIP results in what’s known as Boutonniere deformity of the finger and I’ll show you a picture of that. 03:27 You have the atlanto-axial region C1-C2 subluxation may then cause the spinal cord to then become involved and as I told you earlier that AM stiffness, in other words, morning stiffness will be greater than one hour, no doubt. 03:45 If you take a look at this picture here, this is the ulnar deviation of the finger. 03:53 As the disease becomes worse, it’ll have more and more ulnar deviation. 03:58 It will have involvement of the metacarpophalangeal joints. 04:02 It will then undergo inflammation with pannus formation and such, what I’ll show you also would be your Boutonniere deformity. 04:13 What you’re seeing her on the left, take a look at those knuckles. 04:17 That’s you metacarpophalangeal. 04:19 Take a look at the fingers. 04:21 They’re moving in which direction? Ulnar. 04:25 Please take a look at the picture on the right. 04:27 I want you to take a look at the pads of your fingers, they are hyperextended and you have flexion of the PIP. 04:36 A combination of the two on the right is then called Boutonniere. 04:41 How many wrists are being involved? Symmetrical both. 04:47 This is pretty Pathognomonic for rheumatoid arthritis, isn’t it? Signs and symptoms, extra articular manifestations, as with some heme issues as I told you earlier with chronic issues what rheumatoid arthritis is. 05:02 And it’s anemia of chronic disease. 05:04 And they also have lymphoproliferative malignancies may result in lymphoma but in general, whenever there’s autoimmune diseases, lymphoma is a possibility. 05:14 Pulmonary, if you then have pulmonary nodules, diffuse interstitial fibrosis that we talked about and also a particular condition in which you have rheumatoid nodules and you have pneumoconiosis. 05:29 What’s a pneumoconiosis? Wait, what is the most common pneumoconiosis in the US? It’s silicosis, the combination of rheumatoid nodules which is fibrinoid necrosis with pulsating histiocytes. 05:41 plus let's say silicosis gives you a particular phenomenon called Caplan syndrome, C-A-P-L-A-N, that I’ll talk to you about in a second. 05:51 Keep that in mind for pulmonary extra-articular manifestations. 05:55 In a cardiac, well, you could have your serositis, you could have pleuritis, you could also have pericarditis or pericardial effusion. 06:04 You could have aortitis and there’s every possibility of coronary arterial disease as well with rheumatoid arthritis. 06:12 I told you we would come back and revisit Felty. 06:17 What is Felty? Extra articular manifestation. 06:19 This time, the patient may be susceptible to infection because of neutropenia. 06:24 Neutropenia with the left upper quadrant fullness is then collectively with the splenomegaly and the Neutropenia is then called Felty’s syndrome. 06:35 You could have rheumatoid vasculisits, scleritis, and we began this entire discussion of connective tissue disease and I showed you SLE as having a huge ring and with the ring of SLE, it may then share overlapping signs and symptoms and lab markers with other connective tissue diseases such as SLE, Sjögren, and such. 07:06 In 2010 the American College of Rheumatology and the European League Against Rheumatism revised the criteria for the diagnosis of rheumatoid arthritis. 07:16 The previous criteria, which were mostly based on the clinical presentation, have received a lot of criticism due to their low sensitivity and their ability to diagnose only advanced stages of the disease. 07:29 According to the new criteria, which you can see on the slide, the target population includes patients who have at least one joint with clinical synovitis or synovitis that cannot be explained by an alternative diagnosis. 07:43 The criteria are divided in 4 categories. 07:45 These include joint involvement, serology, acute-phase reactants and duration of symptoms. 07:51 If the cumulative score is 6 points or greater the diagnosis of rheumatoid arthritis can be made. 08:02 Management, first line, NSAIDs. 08:08 Now, usually, it’s going to be for exam purposes but in reality, what are you really going to use? It’s called disease modifying anti-rheumatologic drugs known as DMARDs. 08:20 These DMARDs or glucocorticoid express but these DMARDs include the drugs that I’m going to give you in a little bit including methotrexate. 08:30 In addition, I’m also going to give you your biologics and biologics referring to anti TNF therapy, let’s take a look. 08:37 The goal is to prevent the flares. 08:40 The earlier that you’re able to get in here and manage rheumatoid arthritis, the quality of life in this young lady is going to be that much better and by doing so, you have also increased the patient’s lifespan. 08:55 The biologic agents, unfortunately, when given at the same time for example, remember you need TNF, Tumor necrosis factor alpha to help you forms some of those granulomas. 09:08 For example, if you are exposed to tuberculosis, you’re then going to - well, if you’re immunocompetent, we are going to then form those prisons for those mycobacterial and that prison is then called cases granuloma. 09:20 That granuloma requires what to properly be maintained? Ah, TNF. 09:26 If you’re using biologics that are anti TNFs, you’ve lost your ability to properly imprison your TB and company. 09:33 Therefore, the patient may be at risk for developing life threatening diseases or infections. 09:38 Now, the examples of DMARDs as I told you earlier will come back to methotrexate, so you have Dihydrofolate reductase inhibitor, what are you trying to do? We’re trying to control the DNA components, aren’t we? So please think of Dihydrofolate reductase, sulfasalazine, azathioprine, or leflunomide, dihydroorotate dehydrogenase inhibitor. 10:03 In other words, you can’t probably form pyramidings. 10:05 They use some of your DMARDs. 10:07 What are DMARDs? The disease modifying agents or antirheumatics drugs. 10:13 As examples for your biologics in general, think of that drug which is then inhibiting TNF. 10:22 The big one here, Etanercept. 10:26 Another one would be something like adalimumab would be the big one and then also, infliximab. 10:30 Please at least note those three in its generic form, remember if you’re taking such biologics, your patient is now susceptible to life threatening infections. 10:41 Now, the difference between biologics and the DMARDs in the above two sections.
About the Lecture
The lecture Rheumatoid Arthritis (RA): Signs and Symptoms by Carlo Raj, MD is from the course Connective Tissue Diseases. It contains the following chapters:
- Signs and Symptoms of Rheumatoid Arthritis
- Management of Rheumatoid Arthritis
Included Quiz Questions
Which of the following is NOT typically seen in rheumatoid arthritis?
- Bouchard’s nodes
- Swan neck deformity
- Ulnar deviation
- Boutonnière deformity
- Atlantoaxial subluxation
Which of the following statements best describes boutonnière deformity? (proximal interphalangeal joint [PIP], distal interphalangeal joint [DIP])
- PIP flexion and DIP hyperextension
- PIP extension and DIP hyperextension
- PIP hyperextension and DIP flexion
- PIP hyperflexion and DIP flexion
- PIP and DIP flexion
Which of the following conditions is most likely to present with morning stiffness of the hands for more than 1 hour?
- Rheumatoid arthritis
- Osteoporosis
- Osteopetrosis
- Osteoarthritis
- Ankylosing spondylitis
Patients with both rheumatoid arthritis and pneumoconiosis related to occupational dust exposure (coal, asbestos, silica) may develop peripheral lung nodules known as what?
- Caplan syndrome
- Mesothelioma
- Felty syndrome
- Sjogren syndrome
- Black lung
Which of the following drugs is NOT a disease-modifying antirheumatic drug?
- Naproxen
- Methotrexate
- Sulfasalazine
- Leflunomide
- Cyclosporin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I like how he repeats important points and focuses on distinguishing between RA and osteoarthritis
Excellent presentation by Dr.Carlo Raj, he is the best teacher.