Playlist
Show Playlist
Hide Playlist
Retinopathy of Prematurity
-
Slides OP Retinopathies.pdf
-
Download Lecture Overview
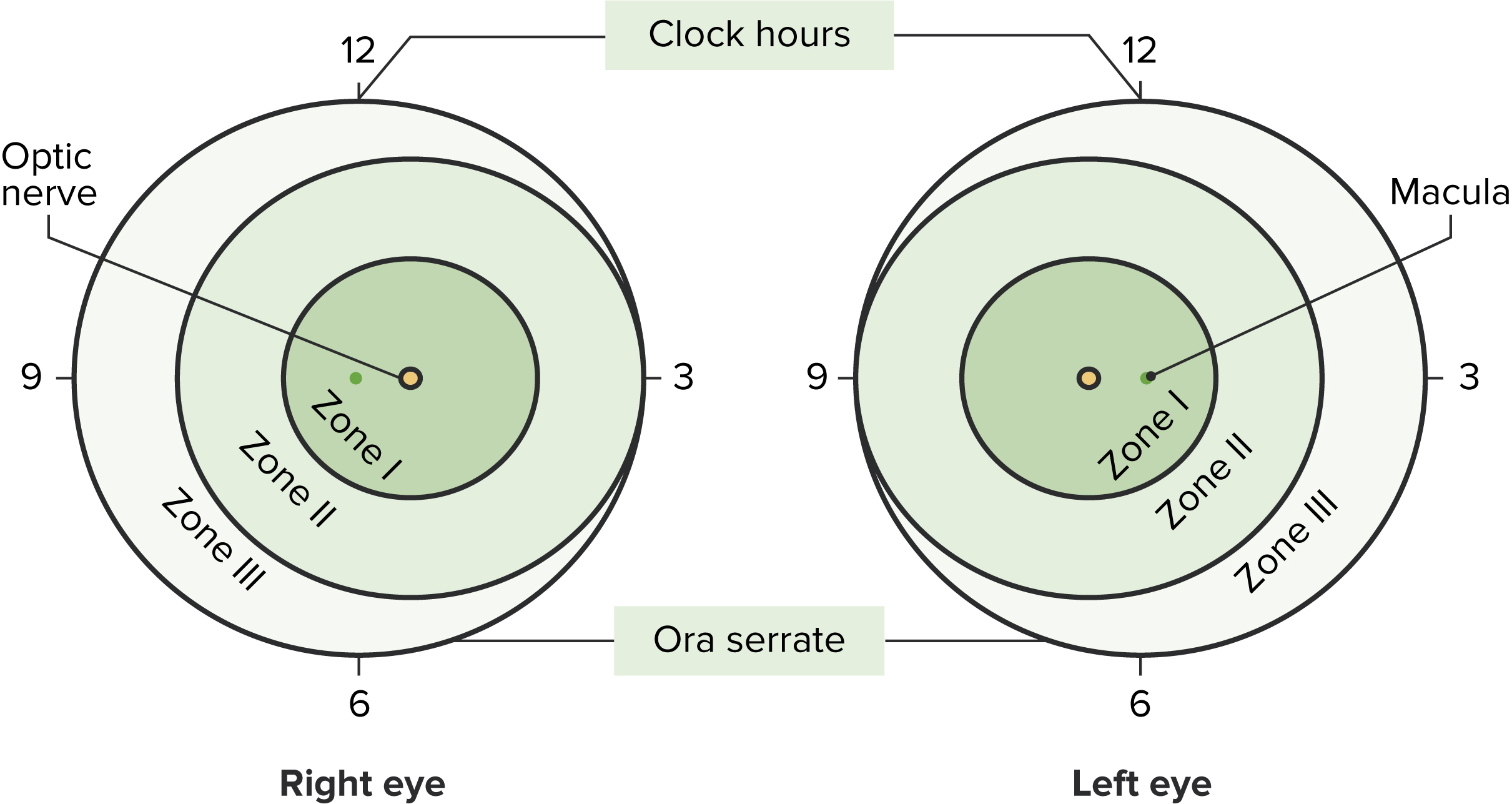
00:00 So it's diabetes, let's talk about the Retinopathy of Prematurity also called retrolental fibroplasia because we do get some fibrosis and scarring and can lead to retraction and retinal detachment. So this is a disease of the retina that occurs in preterm infants, and it's mostly abnormal vessel proliferation, we're going to talk about the pathophysiology about why this happens. The basic endpoint is that we are going to have prominent neovascularization in these eyeballs, in the retinas of these babies. And as a result of the leakiness, the hemorrhage, the scar formation and the retraction we're going to get retinal detachment. So the major features of the retinopathy of prematurity, we're not seeing hard exudates for example, we're not seeing cotton wool spots so much, we're seeing neovascularization and retinal detachment. It is the leading cause of blindness in infants. 01:06 Here, we're going to step through now kind of the pathophysiology of how this happens. 01:13 So, infants who are born prematurely before 36 weeks or so of gestation, remember 40 weeks kind of the normal gestational age. So 36 weeks and certainly if the baby is born at 32 weeks or 28 weeks or 24 weeks, that's even more of an issue. The vasculature of the eye requires a certain level of oxygenation to develop normally. And in ___, that level of oxygenation is determined by what is perfusing through the baby but clearly the baby is not being exposed to high levels of oxygen and the eye has not seen high levels of oxygen. 01:51 So the eye is trying to develop and is used to developing under certain oxygen tensions. 01:57 Baby gets born early and the lungs are immature so we do not have the normal production of surfactant, the lungs can inflate appropriately and what we do is we do a variety of maneuvers including putting the babies in little isolettes and we give them higher oxygen tension so that the rest of the body gets enough oxygen except that the eye wants to develop those last 4-8 weeks under a lower oxygen tension. That higher level of oxygen in the eye now of this premature infant will lead to increased reactive oxygen species, ROS on your slide, and that combination will lead to injury in the newly forming endothelial cells. 02:41 Remember this in an immature vascular bed that wants to develop at a relatively lower level of oxygen and now it's seeing too much oxygen. So that higher oxygen concentration leads to damage and we end up with capillary constriction. So, it's the appropriate response of the eye under those circumstances, but now we're not getting adequate flow to the developing retina. The response of the retina says "Dude we need more blood supply." And so what it does is it makes a whole lot more of vascular endothelial growth factor. That's going to be the major driver of this is that there's a relative hypoxia, too much VEGF, and now we're going to drive whole new sprouting of brand new immature blood vessels kind of inappropriately by having this elevated VEGF. And it's all a matter of putting too much oxygen too soon into an immature vascular bed. As an end result, we get abnormal neovascularization and because those vessels are immature as they're sprouting and growing quite happily, they have increased vascular permeability. There's going to be bleeding, there is going to be organization of the hemorrhage, there is going to be scarring, there is going to be contraction of that, and then we're going to detach the retina. So that's the pathophysiology related to this. The associated risk factors, you can have babies who will have a low birth weight but really it's about low gestational age. So less than 36 weeks. 04:21 And it's largely because we're giving them supplemental oxygen therapy that's driving this process. There may be genetic elements that make certain babies more prone to this. Not every baby that we put in an isolette and give supplemental oxygen will develop the retinopathy of prematurity, but there are certain polymorphisms within the human population such as the predisposition to make a certain level of VEGF that will influence that. Clearly, secondary infections can feed in to this process and there can be congenital cardiac defects sometimes associated with prematurity that will affect oxygenation overall. So we're looking at the eye, the fundoscopic exam of this eye, of the eyes of the baby who has this and we're seeing arterial tortuosity, venous dilation, this is representing the response of the vasculature to hypoxia. We're also seeing retinal hemorrhages because of the neovascularization. And then, in this area we will get the retinal fibrous proliferation in response to the organization of retinal hemorrhages. We will have whole areas of the retina that become relatively avascular and will die and we will get then also the separation, we'll get retinal detachment.
About the Lecture
The lecture Retinopathy of Prematurity by Richard Mitchell, MD, PhD is from the course Posterior Segment Eye Diseases.
Included Quiz Questions
What is retinopathy of prematurity also known as?
- Retrolental fibroplasia
- Non-proliferative retinopathy
- Proliferative retinopathy
- Hypertensive retinopathy
- Retrolental metaplasia
What is one of the hallmarks of retrolental fibroplasia?
- Retinal detachment
- Retinal reattachment
- Retinal tear
- Retinal degeneration
- Retinal agenesis
What is a predisposing factor for retinopathy of prematurity?
- Congenital cardiac defects
- Increased paternal age
- Postpartum depression in the mother
- High birth weight
- Maternal diabetes mellitus
What is a feature seen on the fundoscopic exam in a patient with retinopathy of prematurity?
- Avascular retina
- Cotton wool spots
- Hard exudates
- Flashes and floaters
- Retinal arterial aneurysms
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |