Playlist
Show Playlist
Hide Playlist
Renovascular Hypertension
-
Slides Hypertension.pdf
-
Download Lecture Overview
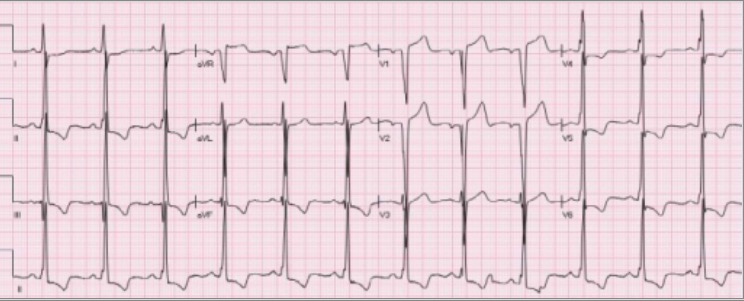
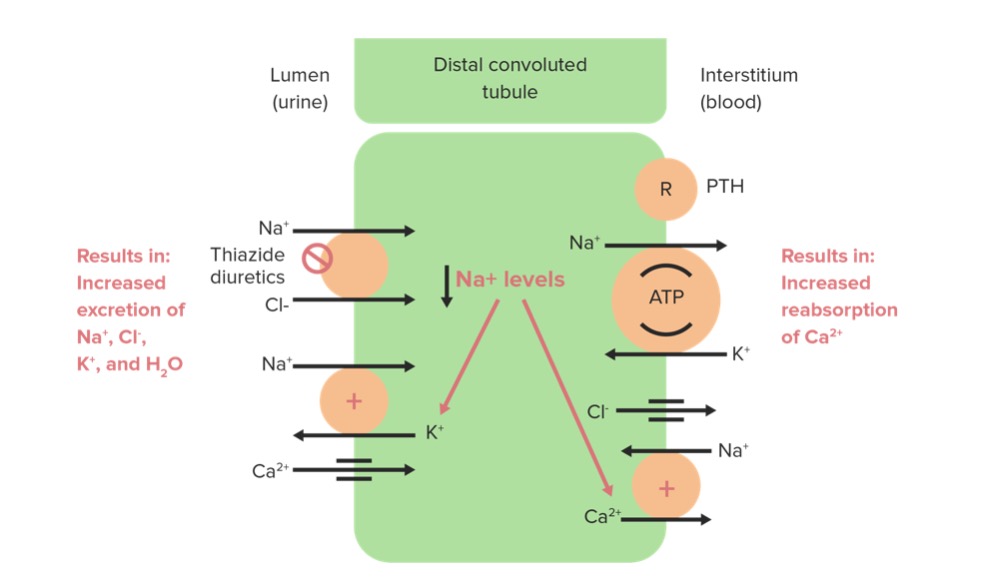
00:00 So, as I said earlier, let's say it's the renal ischemia. How? Elderly patient male approximately 45 years of age, obese. Without a doubt, you're thinking what, please? Atherosclerosis. Young female, 37 years of age, not obese, not hyperlipidemia, lipid profile perfect, but you do a renal angiogram. What does that mean? You are actually checking out the renal arteries and in there you ended up finding a beaded appearance in a young female 30 years of age. Where am I? Renal artery. What does that mean in terms of perfusion to the kidney and the glomerulus? Decreased, what is this called? Renal ischemia. What receptor do you have in juxtaglomerular apparatus, please? Beta-1, good. You have beta-1 receptors, are they stimulated? Yes, they are. 00:47 Just like the heart, what does beta-1 mean to you? Catecholamine. Here in the juxtaglomerular apparatus, the beta-1 receptors have been stimulated. Why please? Renal ischemia. Why please? Ask yourself the question why every single time and you get your answer. Absolutely you will because you have asked the fundamental question and at some point you will find the answer that everyone is satisfied with. Let it be the patient. Let it be a question. Let is be an attending. Who may ever it may be. But now you have renal ischemia due to atherosclerosis maybe fibromuscular dysplasia. What have you? You have increase in renin. You continue. 01:21 Increase in angiotensin 1 go up into lungs, don't you? What enzyme do you have there, please? ACE. What are you going to create? Angiotensin II. What are you trying to do? We have decreased perfusion to the kidney specifically. You increased the angiotension II. Are we done? No. But what do you know about angiotension II, please? Angiotension II causes vasoconstriction everywhere globally. But if it is down in your glomerulus, where does the angiotensin II love to act? The efferent arteriole is its preference. Is that clear? The efferent arteriole. Are you picturing that? The efferent arteriole. Remember in physiology, the efferent arteriole, if it underwent a vasoconstriction, what then happens to the hydrostatic pressure over the glomerulus. Good. You increase you hydrostatic pressure over the glomerulus. 02:11 What are you trying to do? You are trying to restore the GFR, glomerular filtration rate because it had an initial decrease, why? Because of renal ischemia. Are you putting things together? Do you understand this is not just pathophys, this is medicine? This is not just pathology. This is not just a subject. It is the concept of medicine and you need to bring everything together so you connect the dots so that you are able to walk through this particular journey. Now with angiotensin II may cause direct vasoconstriction or it may then actually work on the PCT so that it reabsorbs the sodium. In addition to that, what else does it do? Angiotensin II works on the adrenal cortex. Really? Are you picturing that? Do you know cortex, what are the layers? GFR. How convenient is that? We have GFR referring to the kidney, we have GFR in the adrenal cortex. But the GFR in adrenal cortex stands for glomerulosa fasciculata reticularis. You learn that from physio already and in anatomy and every other subject, which you have already looked at. So here I want you to focus upon the glomerulosa. Ready? Your automatic reflex will tell me what hormone? Aldosterone, good. Guess what is responsible for releasing or forming your aldosterone. Angiotensin II. What does aldosterone do? Are you with me? Where are you now? Aldosterone, once you go to the collecting duct. What do we trying to do? With aldosterone, you are going to reabsorb sodium. My goodness gracious. 03:35 You are reabsorbing a lot of sodium. What is that going to do to your blood pressure? Secondary hypertension, all because you caused renal ischemia, why? If it is young female, what is my diagnosis? Most likely, please. Good. Fibromuscular dysplasia. If it is an elderly male, atherosclerosis. Good job. Let us continue. 04:02 Here it is. You see that arrow right there. What does that look like? It look like atherosclerosis to you. My goodness no, that is beaded appearance, isn't it? It looks like a string of beads that you may wear around your neck right now. You see that necklace that you have on your neck. That is a beaded apperance. Here it is. But where am I? This is not around your neck it is your renal artery. It is undergoing dysplasia in what patient? Young female. What do you think is happening to the caliber of that renal artery? Is it decreasing? The renal artery. What happens to perfusion to kidney? Decrease. What is that called? Renal ischemia. 04:36 What are you going to do JGA? Stimulate. What is the receptor? Beta-1 receptor. What are you releasing? Renin. We just talked about all these. Renin does what, angiotensin I, angiotensin II. 04:45 Angiotensin II what does it do? Vasoconstriction. Take a look at that algorithm we just went through. Angiotensin II has direct vasoconstricting activity. It also increases aldosterone, also reabsorbs sodium, diagnosis number 1. Diagnosis number 2, atheromatous disease. You think athero. 05:06 Please focus upon athero. But what if you are giving this patient an ACE inhibitor in the setting of atherosclerosis? You have just completely inhibited the formation of your angiotensin II. Why would you want to do that in this patient when the kidneys are trying to be protected? So, therefore, it's contraindicated in this patient, is that clear? Now give me where an ACE inhibitor would be the first line of treatment or call it "renal protective". In diabetes mellitus, ACE inhibitor is the first thing that you want to give if your patient comes in with microalbuminuria. 05:43 Now renal parenchyma disease. What are we talking about here? Talk about PKD, polycystic kidney disease. As soon as you hear this, we will talk about this in nephrology and it is the fact that you have autosomal dominant polycystic kidney disease. That is one I want you to focus upon. You should be able to quickly tell me the gene, with that remember all we are doing here is review, but it is also important that you make sure that you connect the dots very quickly. Eighty-five percent of your patients with polycystic kidney disease, autosomal dominant type is PKD1. Is that clear? This is an autosomal dominant. You have a cyst in the kidney resulting in hypertension. Do not equate polycystic kidney disease with renal failure immediatley, is that clear? They're two different entities. "What did you say Dr. Raj?" I said do not equate polycystic kidney disease with the renal failure immediately. 06:31 They are two different diagnoses. Could you go into renal failure with polycystic kidney disease? Yes, you can. Immediately? No, ,it is insidious. What does that mean? It takes a long time before we actually go into renal failure. Is that clear? With that said, with PKD you have hypertension. What kind? Secondary may result in berry aneurysm amongst other things. Diabetes mellitus. Once again what is that going to cause? It is called non-enzymatic glycosylation, NEG. Or some of you might have heard of it as being advanced glycosylated end products. What is going to happen to your blood vessel? Specifically done in your arterial. It might undergo closure. It might undergo once again closure in which it may result in secondary hypertension. Important diagnosis and differentials under secondary hypertension, is that clear? And at this point, I will look at. It is pretty much to kidney. We know vascular hypertension, secondary.
About the Lecture
The lecture Renovascular Hypertension by Carlo Raj, MD is from the course Hypertension: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following receptors is found in the juxtaglomerular apparatus?
- Beta-1 adrenergic receptor
- Beta-2 adrenergic receptor
- Angiotensin receptor
- Alpha-1 adrenergic receptor
- Alpha-2 adrenergic receptor
What substance is released during renal ischemia that leads to angiotensin I induced vasoconstriction?
- Renin
- Angiotensinogen
- Angiotensin II
- Epinephrine
- Aldosterone
Where is the site of action of angiotensin II?
- Efferent arteriole
- Afferent arteriole
- Macula densa
- Granular cells
- Mesangial cells
What is the most likely cause of hypertension in a young woman (under age 40) and what is the diagnostic test of choice?
- Fibromuscular dysplasia and renal angiography
- Atheromatous disease and renal angiography
- Fibromyalgia and renal angiography
- Diabetes mellitus and renal ultrasound
- Fibromuscular dysplasia and renal ultrasound
Which of the following drugs is contraindicated in atheromatous disease?
- Enalapril
- Metoprolol
- Nifedipine
- Hydrochlorothiazide
- Aliskiren
Customer reviews
4,4 of 5 stars
| 5 Stars |
|
6 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
he speaks too fast and goes too fast while lecturing i wants more explanations not like this
Raj!!! Lecturio couldn't have picked a better physician to teach us.
Dr Raj has awesome gift of explaining medicine :) Thank you, dr Raj :)
Make me understand this so well. Thanks you Dr. Carlo Raj