Playlist
Show Playlist
Hide Playlist
Polyarteritis Nodosa vs. Erythema Nodosum
-
Slides Erythema Nodosum.pdf
-
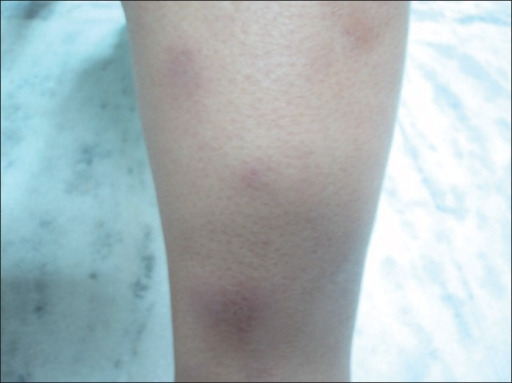
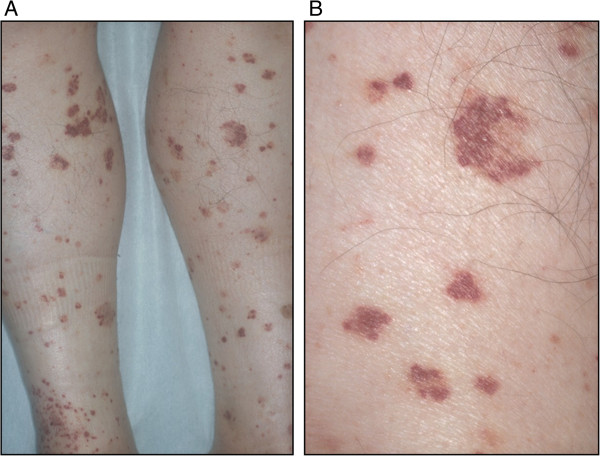
Download Lecture Overview
00:03 So let's go revisit polyarteritis nodosum for a second. 00:06 So, again, this is a systemic necrotizing vasculitis of medium-sized arteries in multiple organ systems, whether it's the skin, the intestines, the kidneys, etc. It's idiopathic. We don't really know what causes pretty much any of the primary vasculidities, though it has been often linked with hepatitis B and hepatitis C virus, maybe about 30% of the time. 00:34 What we see if we were imaging arteries, we see it's segmental, transmural -- that means through the entire wall of the vessel -- inflammation that leads to either luminal narrowing, potentially thrombosis within the vessel with downstream ischemia, ballooning aneurisms of the vessel, as we see in our image here on the right, and of course, tissue necrosis due to downstream ischemia. The diagnosis would be performed by checking a variety of autoimmune tests. 01:06 It is an ANCA negative vasculitis, unlike a variety of ANCA positive vasculidities. 01:12 You typically do require a biopsy, whether it's a biopsy of the skin where you might see leukocytoclastic vasculitis, or a biopsy of a kidney, for example. And a slam dunk finding would be evidence of those aneurisms, those scattered aneurysms and irregular constrictions when you performed a mesenteric or a renal arteriography. 01:35 Treatment for polyarteritis nodosa and for most other vasculidities is steroids up front, plus or minus cyclophosphamide. And, of course, since our patient does have hepatitis B, we probably would want to take care of that as well. 01:51 Other manifestations of PAN to consider knowing that we're talking about arteries that go to multiple organs in the body, you may see palpable purpura on the skin, tender subcutaneous nodules, which is what we're seeing in our patient. You may see a pattern of livedo retcularis, particularly in the lower extremities. 02:08 Renal disease with PAN involves renal artery aneurysms, which can, of course, lead to downstream ischemia, potentially hypertension, renal infarcts and acute kidney injury. Our patient's creatinine was a 1.4, which may support that. Neurologically, because you're also talking about the blood supply to nerves, you can see mononeuritis, potentially mononeuritis multiplex if multiple peripheral nerves are involved. 02:32 And then from a gastrointestinal standpoint, you'd be looking for mesenteric ischemia. 02:37 So, having spoken about polyarteritis nodosa for a moment, I don't want to write off erythema nodosum yet, so let's take a little bit of a closer look at E. nodosum. 02:46 Erythema nodosum is a delayed type hypersensitivity reaction leading to inflammatory panniculitis, which means inflammation in the subcutaneous fat, particularly, of the anterior lower legs, though it can occur in other locations as well. It's more common in younger women, and there's a variety of different causes, as we've suggested. Medications, most commonly sulfas, oral contraceptive pills, penicillin. 03:11 One drug you probably won't find on this list is the drug that she newly started, entecavir. So, I'm thinking that may just be a coincidence. 03:20 Infections, streptococcus, tuberculosis, some fungal infections like histiocytosis, coccidioidomycosis. A number of inflammatory conditions most classically would be sarcoidosis -- particularly with the Lofgren's subtype of that -- inflammatory bowel disease. Some malignancies you may see E. nodosum, pregnancy, and then a third of cases are actually idiopathic and we never never find out exactly what precipitated it. 03:49 Shown here, is a picture of some tender, non-ulcerated erythematous nodules. It's, of course, hard to visualize tender subcutaneous nodules since you may not see much on the skin because it's really palpating the area and finding that tender, indurated area that tells you what's going on there. 04:07 The onset can be over several days. It, sort of, depends on what the etiology is. 04:12 And it is often preceded by some URI symptoms; maybe some fevers, maybe some arthralgias, maybe even some coughing, and sore throat. And it may, of course, depend on what the particular etiology of our patient's erythema nodosum is. 04:28 A biopsy, if you were to perform it, would not tell you what caused the erythema nodosum, but it would confirm the diagnosis because you'd find a granulomatous panniculitis in the skin. 04:40 So, we've still got E. nodosum and PAN on our hands. Let's take a look back at the case again, and highlight some key points. 04:49 So, again, 52-year-old woman, this would go more in line with polyarteritis nodosum, in particular with the recently acquired hepatitis B infection, neither one of which would be seen with erythema nodosum. 05:03 The presence of those fevers, arthralgias, painful bumps, and sub-acute onset of symptoms, kind of supports both diagnoses, so it's not going to help to tease those 2 things apart. 05:15 The prandial abdominal pain, however, exacerbated by eating, again, that's concerning for mesenteric ischemia, much more likely to be seen with polyarteritis nodosa. 05:24 But keep in mind, that patients will have inflammatory bowel disease, which could also be characterized by some belly pain, and even some hemoccult positive stool, could also lead to erythema nodosum. 05:36 o, something to be mindful of. And then lastly, the weight loss, the fatigue, the malaise, all those constitutional symptoms really can go along with both conditions as well, so that's not helping to tease apart our diagnosis. What I think is most important here is the absence of the things that would support E. nodosum. So, we're not getting a story of sarcoidosis. We're not getting a story of any of the 2 inflammatory bowel disease types. There's no new medications or at least no common culprits. Entecavir would not be one of the ones we'd think of. 06:10 No recent strep infection, no tuberculosis, etc. All those things are going to steer us away from EN, especially when you're looking at a board review question. There should be an obvious associated condition in the history. On physical exam, the most characteristic features here that steer one way or the other is the tender purpuric papules on the calves, not on the pretibial areas, definitely suggest more of a polyarteritis nodosum type picture, and you can imagine that if we were to biopsy that area, we'd find a leukocytoclastic vasculitis. In contrast, the anterior or pretibial area of the legs is where we do a biopsy and you'd find panniculitis supporting erythema nodosum. 06:55 So, with that, I think we can safely say that despite this being the erythema nodosum video, this looks like polyarteritis nodosum, instead. 07:05 If our patient, however, did have erythema nodosum, just to round off this topic, we would, of course, want to identify and treat the underlying condition. Maybe it's the beginnings of sarcoidosis, maybe tuberculosis, a variety of other things. 07:17 We want to make sure we try and find what could be the cause. 07:21 Treatment is pretty straightforward. You can use some NSAIDs for pain control and using the anti-inflammatory properties of NSAIDs to cool it down. Steroids would be a, something you would use only as needed if they're particularly painful lesions involved, but would be reserved for only extreme cases. And alternatively, since it's kind of is a self-limiting condition, it's probably going to resolve either after you treat the underlying cause, or it'll just resolve on its own within weeks to months. You could just wait it out.
About the Lecture
The lecture Polyarteritis Nodosa vs. Erythema Nodosum by Stephen Holt, MD, MS is from the course Allergic and Immune-mediated Skin Disorders.
Included Quiz Questions
Which of the following statements is true regarding polyarteritis nodosa (PAN)?
- Renal arteriography reveals multiple constrictions and aneurysms.
- HBV/HCV infection is the most common cause of PAN.
- Skin biopsy reveals granulomatous panniculitis.
- It is a self-limiting condition and can be managed with NSAIDs and corticosteroids.
- It is associated with antineutrophil cytoplasmic antibodies (ANCAs).
Which of the following is associated with erythema nodosum?
- Prodromal symptoms
- Recent staphylococcal infection
- Type II hypersensitivity reaction
- Treatment with glucocorticoids plus cyclophosphamide
- Positive ANCA test result
Which of the following is useful for distinguishing polyarteritis nodosa from erythema nodosum?
- Location of the lesions
- Subacute onset
- Constitutional symptoms
- Painful nodules
- Arthralgias
Which of the following pairings is correct?
- Erythema nodosum – Panniculitis
- Polyarteritis nodosa – Large vessel vasculitis
- Thrombophlebitis – Delayed hypersensitivity reaction
- Mycosis fungoides – Fungal infection
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
The way the cases are worked through is really good. explaining each differential is something not many people do and works really well