Playlist
Show Playlist
Hide Playlist
Pneumothorax
-
Slides 09 PleuralDiseases RespiratoryAdvanced.pdf
-
Download Lecture Overview
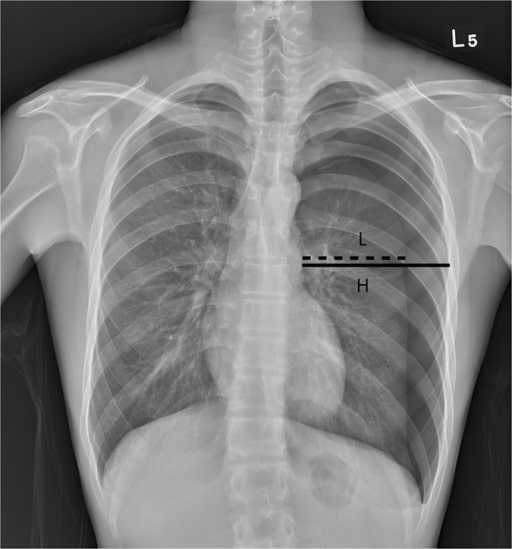
00:01 So the next part of this talk, I’m going to discuss pneumothorax, and that’s air in the pleural space. There are different types of pneumothoraces. First of all, there are spontaneous pneumothoraces which are occurring without any evidence of trauma. And those are divided into primary. That means patients with no underlying lung disease, and this tends to be young, tall, thin man. They may have an inherited disease of the connective tissues such as Marfan’s which makes them much more likely to have this or secondary pneumothorax, and those occur in patients with underlying lung disease such as COPD, cystic fibrosis, etc. Then there are traumatic pneumothoraces which actually most often are probably iatrogenic ones which occur during patients having needle insertion around the thoracic cavity. So that will be a lung biopsy or central line insertion, something like that, where in fact, the chance of getting a small pneumothorax is relatively high, and of course trauma can cause a pneumothorax as well. 01:01 So, primary pneumothoraces normally occur around the age of 20. They’re two or three more times common in men than women. They’re increased in smokers and they’re increased in patients who use recreational drugs such as cocaine and marijuana. This also increases, as I mentioned, in patients with Marfan’s syndrome due to the weakness of their connective tissue. Secondary pneumothoraces would occur in older people, usually over 50, and they normally have a known lung disease such as COPD. The symptoms of pneumothorax are very simple; sudden onset chest pain, tightness, and dyspnoea. One moment the patient is well, the next minute, they have a problem with their chest. Normally, with pain initially, and then increasing breathlessness as the pneumothorax develops. 01:47 When you examine the patient, the pneumothorax is usually obvious. The trachea is deviated away from the pneumothorax affected side. Percussion note will be resonant, in fact, may be hyper-resonant that is quite tricky to detect. There will be reduced breath sounds and reduced vocal resonance. At that right-hand side, for example, in this person with the right sided pneumothorax, will not expand as well as the left-hand side. And because there are no divisions in the normal pleural space, air will rise to the top. So with smaller pneumothoraces, you hear the abnormalities at the top. With a large pneumothorax, it will be throughout the lung. So, how do you make the diagnosis clinically? It’s very obvious usually and you can confirm it using a chest X-ray, and really no other investigations are necessary acutely. And you can see here on this chest X-ray that the typical finding is somebody with a large pneumothorax which has got loss of lung markings in the periphery of the lung which is just black. There are no visible vessels or bronchi present there at all. And there’s a pleural line which shouldn’t be there. 02:45 How do we treat pneumothorax? It depends on the size. So if somebody presents with primary pneumothorax, and it’s very small and they’re not terribly breathless, actually, you don’t need to do anything at all. It will probably resolve by itself over time. You just need to monitor with a chest X-ray, and the patient may not even need to come into the hospital. 03:01 If it's very large. They’re probably quite breathless and they probably require chest drain, and therefore, they may have to come into the hospital. 03:08 The ones in between where you have a two centimetre rim of air around the lung, for example, the patient is feeling a bit breathless, then there’s a halfway step between doing nothing and insertion with chest drain, and that’s aspirating. This way, you put a needle in, and similar to the pleural effusion, you suck out a large amount of air, and you see whether that makes a difference to the pneumothorax. So you put the needle in, aspirate a litre or two, do the chest X-ray, see whether the lung has come up. If it hasn’t come up, then they may need to come into the hospital to have a chest drain. It depends. 03:43 If somebody has to have a pleural drain, then we normally put the pleural drain for pneumothoraces on an underwater seal. That means that the tube that comes out the chest goes underwater and that prevents air from re-entering the pleural space once it leaves the pleural space. 03:57 This rapidly removes most of the pleural space air and the patient would feel alot better very shortly. The problem with pneumothoraces is that they’re due to a small hole forming in the visceral pleura leaking air into the pleural space. And this hole forms spontaneously in primary pneumothorax and will heal, but until it’s healed, the way air leaking out from the lung into the pleural space, and that’s called the bronchopleural fistula. 04:26 So if somebody has a continuing bronchopleural fistula, what will happen is the air will drain, the air will go out into the pleural space, and then go down the drain, and be visible as bubbles as the patient breathes or coughs coming underneath the underwater drain. So, a continuing bubbling in somebody with an inserted chest drain and a previous pneumothorax suggests there's continuing bronchopleural fistula, which means if you remove the drain, all that will happen is that the air in the lung will collapse again with a new pneumothorax. 04:56 In patients where you do have a persistent bronchopleural fistula, and normally, we give patients about five to seven days to heal, then you may want to do surgery to repair the hole. You also do surgery if the patient presents with two primary pneumothoraces on one side as the chances are that then they would have the third one and the fourth one. 05:17 After one pneumothorax, the chance of recurrence is about 30% after two, it goes up to 50%, 60%. 05:23 If you had three on the same side, then it goes up to 70%, 80%. Hence, we suggest that surgery is going to be required if you had two on one side. 05:31 The treatment so far described is for primary pneumothorax, for patients with no underlying lung disease. With secondary pneumothorax, the patient has a big problem because they have an underlying lung disease, their lung reserves their ability to cope with the small pneumothorax or even a minimum pneumothorax becomes much harder, and they may be much more breathless with a very small amount of air in the pleural space than somebody with a primary pneumothorax, and therefore, they probably will require chest drain. So secondary pneumothorax, most of the patients, especially the asymptomatic, will require chest drain to make sure that they’re safe and they can recover from a pneumothorax without risking respiratory failure.
About the Lecture
The lecture Pneumothorax by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Pleural Disease.
Included Quiz Questions
Which patient with pneumothorax is considered to have a primary spontaneous pneumothorax?
- A patient with absent clinical lung disease
- A patient with chronic obstructive pulmonary disease
- A child with cystic fibrosis
- A patient after lung biopsy
- A patient with a recent rib fracture
Which physical examination finding is not typical for a pneumothorax?
- Unilateral hyperresonance with ipsilateral tracheal deviation
- Decreased breath sounds over the region with hyperresonance
- Decreased vocal resonance over the region with hyperresonance
- Decreased unilateral vocal fremitus with ipsilateral reduction of breath sounds
- Reduced unilateral chest expansion with reduced vocal fremitus
Which of the following percussion notes is most characteristic of pneumothorax?
- Hyperresonance
- Resonance
- Dullness
- Stony dullness
- Normal findings
Which of the following is FALSE regarding the treatment of pneumothorax?
- A 1st episode of a small primary spontaneous pneumothorax rarely responds to treatment with supplemental oxygen.
- Bronchopleural fistulas require underwater seal drain.
- A 1st episode of a small primary spontaneous pneumothorax generally resolves spontaneously.
- A 1st episode of primary spontaneous pneumothorax > 2 cm in a stable patient is usually aspirated with a syringe.
- Large pneumothoraces are generally treated with a chest drain.
Which of the following is the most appropriate next step in the management of a patient with a 2nd episode of ipsilateral primary spontaneous pneumothorax?
- Chest tube
- Oxygen supplementation if < 2 cm
- Needle aspiration if > 2 cm
- Oxygen supplementation and needle aspiration if < 2 cm
- Observation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |