Playlist
Show Playlist
Hide Playlist
Peripheral Vascular Disease (PVD): Management
-
Slides Peripheral vascular disease Special Surgery.pdf
-
Download Lecture Overview
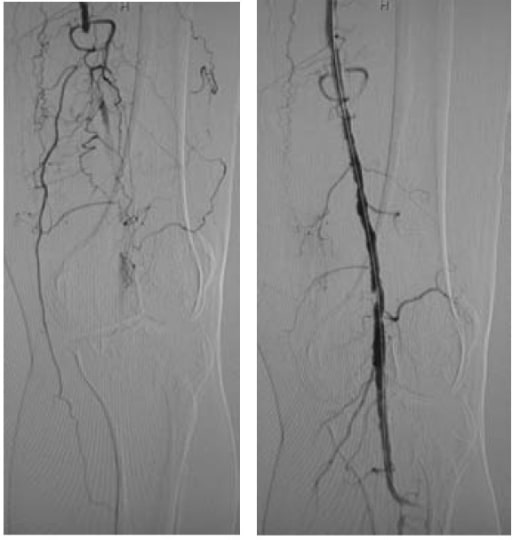
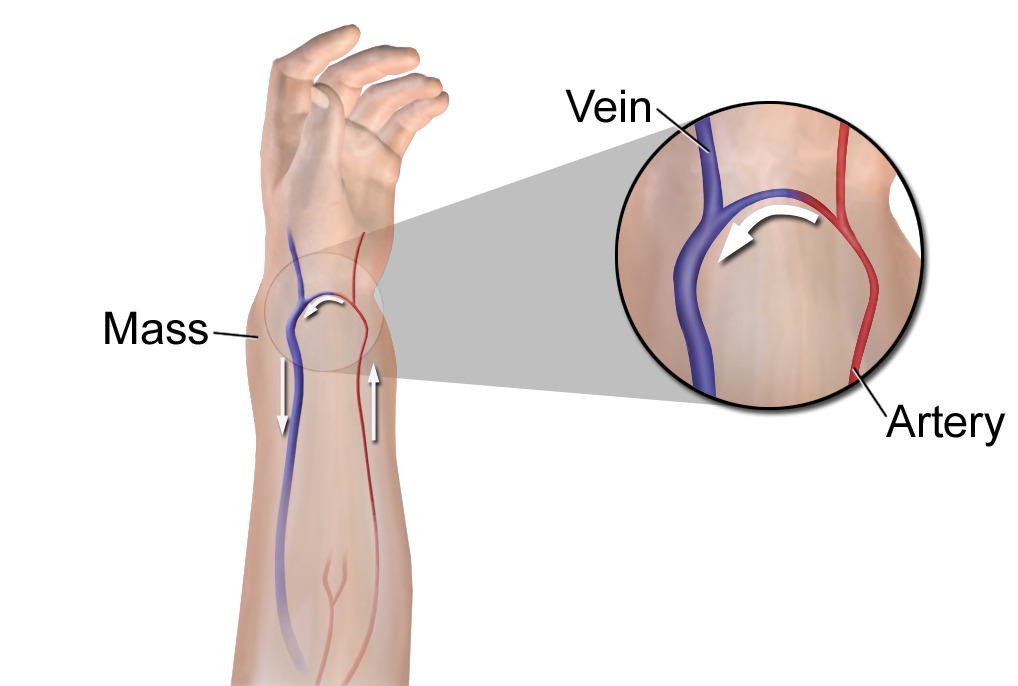
00:01 Medical therapy is incredibly important in patients with peripheral arterial occlusive disease. 00:06 Here, we’ll take a look at a few pharmacologic and lifestyle change options. 00:11 Pharmacologically, we can put the patient on antiplatelet therapy, whether it's aspirin or Plavix. 00:18 Next, statins. 00:20 As you recall, statins have the (inaudible 0:22) properties. 00:24 And as a result of chronic biomechanical stresses on the arterial walls, hypertension or antihypertensive medications can be helpful in these disease processes. 00:34 Unfortunately, these usually limit the propagation and doesn't actually treat the stenosis. 00:42 Lifestyle changes are quite important. 00:44 And oftentimes, it's very easy for us to recommend. 00:47 Unfortunately, it’s more difficult for the patients to follow the programs. 00:51 Smoking cessation, as you know, smoking is a risk factor for all vascular disease. 00:57 Cessation of smoking is one of the most important things to do. 01:02 Exercise, particularly in patients with claudication, exercise is the first line therapy, not surgery. 01:09 So, remember, if a clinical scenario is presented to you, the next step of management is a regimen of exercise, smoking cessation. 01:17 And lastly, some patients are put on a peripheral arterial dilator called cilostazol. 01:22 Now, let's focus a little bit more on the peripheral arterial occlusive disease management. 01:27 Remember, the most common location for arterial occlusion is in the superficial femoral artery. 01:34 This leads to calf claudication symptoms. 01:38 It's fairly easy to figure out what level of occlusion there is. 01:41 Usually, the symptoms occur one joint space below the area of the occlusion. 01:49 For aortoiliac disease, typically, the symptoms are in the upper thigh or buttocks. 01:58 Now, let's describe Poiseuille’s law. 02:02 Remember, when I described how there is a pressure differential in a stenotic region, this is the premise behind an ankle brachial index. 02:11 On the left side of the screen, you notice a normal-sized vessel. 02:16 As it progresses to a stenotic region, the pressure drop is proportional – directly proportional to the flow. 02:24 However, it's indirectly proportional to the fourth power of the radius. 02:29 Therefore, when your radius completely drops, the pressure gradient is actually decreased to the fourth power by the radius. 02:38 This is, again, the premise behind why there's a pressure difference between the ankle and the arm. 02:47 Let me ask you a question. 02:48 So, what’s so concerning about peripheral arterial occlusive disease. 02:52 I’ll give you a second to think about this. 02:56 The answer is risk of limb loss. 02:59 Thankfully, the vast majority of patients with particularly claudication symptoms do not lose their extremities. 03:06 This is due to adherence to medical and lifestyle changes, as well as a very aggressive exercise regimen. 03:14 However, sometimes patients have tissue loss and a deterioration of their clinical arterial disease and amputation is unavoidable. 03:25 The most important determinant of risk for limb loss in peripheral arterial occlusive disease is diabetes, age and, again, continued smoking. 03:36 Remember, vascular societies recommend, if the patient is already bedridden and not mobile, there's no need to revascularize the patient. 03:45 Amputation is perhaps the best approach. 03:50 Let’s start with another question. 03:52 As you know, patients can develop ulcers, but sometimes ulcers are due to arterial disease and other times due to venous disease. 04:00 What is the difference between an arterial versus venous ulcer? I’ll give you a second to think about this. 04:09 Venous ulcers typically occur on the medial ankle or malleolus. 04:13 They are associated with pigmentation, typically bilaterally. 04:18 And usually unless it's infected, the patient is painless. 04:22 This is a little different than arterial ulcers, which normally occur in the heels and toes, can be painful and have a punched-out appearance due to the ischemic regions. 04:32 Now, let's discuss what indications for surgeries are. 04:35 Rest pain, necrosis, non-healing infection. 04:40 Remember, claudication that does not respond to medical therapy and affects quality of life significantly – take a look at this list of indications for surgery. 04:50 These have one thing in common. 04:52 They’re all end stages of peripheral arterial occlusive disease. 04:56 Your job and my job, as a physician, is to try to halt the progression to end stage diseases that require bypass surgery. 05:06 Nevertheless, some patients will require surgery. 05:10 For example, this patient has gangrene of the foot. 05:13 This patient – a gangrene and ulcer will not heal unless there is adequate inflow.
About the Lecture
The lecture Peripheral Vascular Disease (PVD): Management by Kevin Pei, MD is from the course Special Surgery.
Included Quiz Questions
According to Poiseuille's law, which of the following relationships does the pressure in a stenotic region of the blood vessel have?
- Directly proportional to the fourth power of the radius
- Inversely proportional to the third power of the radius
- Inversely proportional to the second power of the radius
- Directly proportional to the third power of the radius
- Indirectly proportional to the fourth power of the radius
Which of the following options is NOT an indication for surgery in cases of peripheral arterial occlusive disease?
- Claudication that respond to therapy
- Rest pain
- Necrosis
- Non-healing infection
- When medical therapy and lifestyle fail to improve the condition
Which of the following risk factors are the most important determinants of limb loss in cases of peripheral arterial occlusive disease?
- Diabetes, age, and continued smoking
- Smoking, age, and hypertension
- Obesity, age, and coronary artery disease
- Obesity, age, and continued smoking
- Diabetes, coronary artery disease, and continued smoking
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
it's easy to keep up with the pp and the professor, and the best: questions during the video, so I don't lose focus ( which is a big problem for me)