Playlist
Show Playlist
Hide Playlist
Pelvic Inflammatory Disease (PID) in Adolescents
-
Slides UrethritisandPID Pediatrics.pdf
-
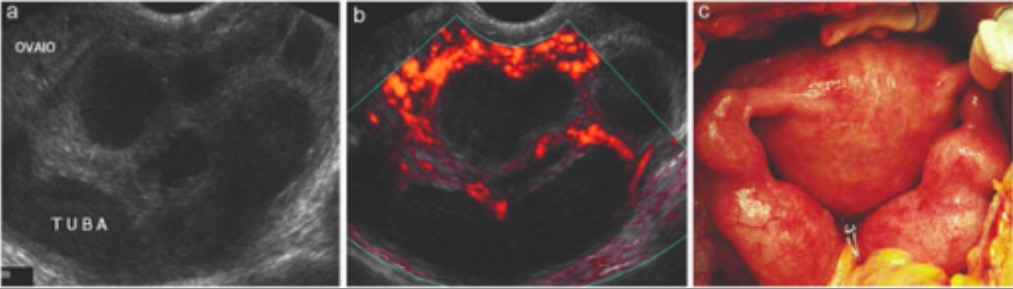
Download Lecture Overview
00:01 Let’s shift gears a little bit and talk about pelvic inflammatory disease or PID. This is a sexually transmitted disease of the upper female genital tract. It’s a complication of cervicitis. 00:16 These patients will have an ascending spread of microorganisms from the lower genital tract into the upper tract. This can include endometritis, salpingitis, tubo-ovarian abscesses, pelvis peritonitis, peri-hepatitis. That peri-hepatitis is also known as Fitz-Hugh-Curtis syndrome. 00:36 Adolescent females are responsible for one-third of all pelvic inflammatory disease in the United States. 00:45 We need to make adolescent females aware of this disease and treat them aggressively when they have it. 00:50 Teen girls are at a higher risk for sexually transmitted diseases than even adults. 00:57 Chlamydia and gonorrhea have a predilection for columnar cells which are in the cervical os of adolescents. 01:04 These cells gradually transform to squamous epithelium during adulthood. Thus, higher rates of chlamydia and gonorrhea can occur in adolescents and PID is common. There are certain risk factors for sexually transmitted diseases in children. One is being at a young age with the first sexual encounter. 01:28 Having multiple sexual partners, having unprotected sex, having a previous history of pelvic inflammatory disease or having bacterial vaginosis associated with pelvic inflammatory disease. 01:42 So, what are the causes of pelvic inflammatory disease in adolescents? One is Neisseria gonorrhoeae and another is Chlamydia trachomatis. There are other organisms that can cause this problem such as Streptococcus, E. coli, Mycoplasma, Ureaplasma, and Bacteroides. Generally, in patients with urethritis, they’ll have a lower genital tract infection, usually cervicitis. This results in an inflammatory disruption of cervical barrier which permits ascension of the bacteria up into the uterus. 02:19 Then multiple vaginal organisms can follow along route. These patients can get a polymicrobial upper tract infection. The plasma cells infiltrate the endometrium and this can decrease motility of fallopian tubes due to inflammation. That can, in turn, lead to a hydrosalpinx or a pyosalpinx. 02:43 Thus, patients can get complications and infections of their upper tract. This can include peritonitis, peri-hepatitis, and a tubo-ovarian abscess. So, let’s talk about what our historical findings or signs and symptoms that we can see in these patients. First, they usually complain of having a lower abdominal or pelvic pain or cramping. That’s in about 80%. About half will have a vaginal discharge. 03:13 These patients may have dyspareunia or pain while having sex. They can have irregular vaginal bleeding. 03:21 And they may have difficulty ambulating secondary to pain. Some call this the PID shuffle. 03:27 Other symptoms include dysuria, fever, nausea, and vomiting. When we see a patient with pelvic inflammatory disease, it’s important to take vital signs. Patients with Fitz-Hugh–Curtis may be very sick. 03:42 We need to assess their hemodynamic stability. We have to assess them for abdominal tenderness. 03:50 Let’s review the physical exam findings for pelvic inflammatory disease and in particular, the pelvic exam. 03:57 The exam with the speculum is not necessary for the diagnosis of PID in an adolescent. 04:04 We don’t typically do that. Usually, we defer the pelvic, that part of the pelvic exam for the regular checkup. However, if a speculum exam is performed, it may reveal vaginal or cervical discharge and an inflamed cervix. A bimanual exam is critical. We have to check for tenderness of the uterus, adnexa, and cervix involvement. If there’s cervical motion tenderness, that definitely raises our concern that this could be PID. So, for the diagnosis of PID, we need at least one of the following: cervical motion tenderness, uterine tenderness, or adnexal tenderness. 04:46 It’s important to get a sense of is it a reliable tenderness or is it just they’re discomfortable with the bimanual exam. That requires a little bit of experience and some careful observation of the patient during the exam. Additional criteria supporting a diagnosis of PID include a temperature greater than 38.3 °C, abnormal cervical or vaginal mucopurulent discharge, the presence of white cells on a wet mount, an elevated sed rate or a CRP, or a positive test for gonorrhea or chlamydia. 05:20 What extra lab findings will we get? Well, we usually check a pregnancy test to make sure they aren’t pregnant. A CBC may show elevated white count especially in frank PID. A sed rate and a CRP may be elevated. In Fitz-Hugh-Curtis, the hallmark is elevated liver function test. We will get a urine dip which will show maybe leukocyte esterase. Vaginal microscopy, a wet mount may show more than 10 white blood cells per high power field. Testing for gonorrhea and chlamydia is indicated and specifically an NAAT which has to be on the first void, not a clean catch specimen. 06:03 Additionally, we will test for other sexually transmitted diseases like syphilis, HIV, et cetera. 06:11 In patients with significant adnexal pain or with significant abdominal pain, we may choose to get a pelvic ultrasound. This can reveal things like fluid-filled fallopian tubes and may be useful to narrow our differential diagnosis, in other words, to rule out appendicitis or some other cause of pain. 06:31 Additionally, the pelvic ultrasound is important for visualization of the tubo-ovarian abscess which is a surgical emergency. So, how do we treat this? Well, antibiotics are the first line. 06:43 Usually, we’ll start with ceftriaxone and doxycycline. Don’t forget to treat sexual partners. 06:49 That’s very important to prevent recurrence of disease. What are the indications for hospitalization? We don’t hospitalize these patients as much as we used to. We used to hospitalize them for education but it’s turning out that it’s not clear that that’s much better than not hospitalizing them. 07:07 That said, we do hospitalize them for surgical emergencies, if they are pregnant, if they’ve failed or had poor response to outpatient therapy, if they’re incapable of tolerating an outpatient regimen of say doxycycline, for severe illness, nausea, vomiting, or high fever, or if they are operable such as a tubo-ovarian abscess. So, what are complications? Well, for a TOA, we worry about bacteria, inflammatory cells, and fluid in the fallopian tubes. This can then lead to an ovarian abscess which is quite a complex problem. Also, in patients with fallopian involvement, there’s a risk for ectopic pregnancy, infertility, and chronic pelvic pain. So to prevent this problem, we have to educate patients on safer sexual practices and condom use. We have to educate them about sexually transmitted infections. It’s important also to consider routine screening of asymptomatic adolescents for sexually transmitted infections. If we can treat the chlamydia early, it’s less likely to become pelvic inflammatory disease. So, that’s my review of urethritis, cervicitis, and pelvic inflammatory disease in adolescent patients. Thanks for your time.
About the Lecture
The lecture Pelvic Inflammatory Disease (PID) in Adolescents by Brian Alverson, MD is from the course Adolescent Medicine. It contains the following chapters:
- Pelvic Inflammatory Disease (PID)
- Historical Findings
- Treatment
Included Quiz Questions
A patient has right upper quadrant pain, fevers, and cervical motion tenderness. What is the most likely diagnosis?
- Fitz-Hugh-Curtis Syndrome
- Klippel-Trenaunay-Weber Syndrome
- Sister-Mary-Joseph nodule
- Kasabach-Merrit Syndrome
- Krukenberg tumor
Which of the following is a key initial event in the pathogenesis of pelvic inflammatory disease?
- Cervicitis
- Vaginitis
- Urinary tract infection
- Endometriosis
- Salpingitis
Which of the following is NOT and important risk factor for pelvic inflammatory disease in adolescents?
- Use of barrier contraception
- Younger age
- History of prior pelvic inflammatory disease
- Multiple sex partners
- Unprotected sex
Which of the following symptoms is least likely to be caused by pelvic inflammatory disease?
- Low-back pain
- Abnormal vaginal discharge
- Worsening of pain during coitus
- Lower abdominal pain
- Abnormal uterine bleeding
Which of the following allows for a presumptive clinical diagnosis of pelvic inflammatory disease and initiation of antibiotic treatment in a sexually active adolescent who presents with lower abdominal pain?
- Cervical motion tenderness
- Nausea and vomiting
- Fever
- Raised creatine phosphokinase
- Low back pain
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I particularly appreciated the explanation of the pathophysiology which helps a lot to understand the symptoms of the disease. Thank you!