Playlist
Show Playlist
Hide Playlist
Pelvic Inflammatory Disease (Emergency Medicine)
-
Emergency Medicine Bord Sexually Transmitted Diseases.pdf
-
Download Lecture Overview
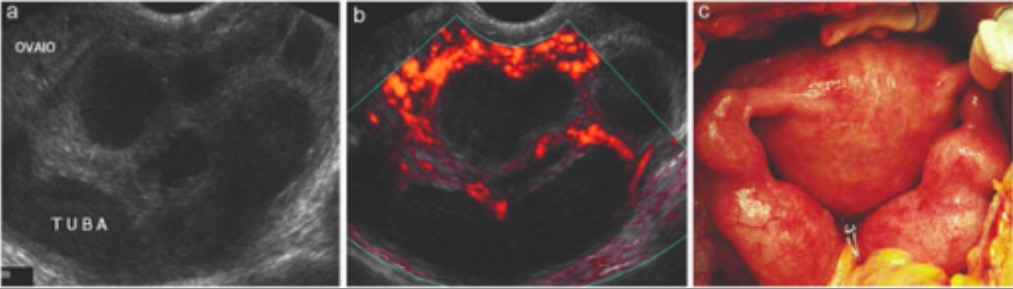
00:02 We’re gonna move on and talk about pelvic inflammatory disease. 00:05 This is an ascending tract infection. 00:07 When I was a student, I was oftentimes very confused about the difference between cervicitis and PID. 00:14 Essentially what it means is that the infection ascends from the cervix into the uterus, the fallopian tubes, and possibly the ovaries, and potentially even into the abdominal cavity. 00:24 So patients can get endometritis which is inflammation and infection of the uterus. 00:31 Salpingitis, which is inflammation and infection of the fallopian tubes. 00:36 A tubo-ovarian abscess that is abscess on the ovary, and then potentially even peritonitis which is when the infection leaves the fallopian tubes and goes into the intra-abdominal cavity. 00:51 Now, the causative organisms here most commonly are gonorrhea and chlamydia, but it can also be associated with anaerobes or possibly enteric organisms. 01:01 We wanna make sure that we’re thinking about PID 'cause there are a lot of implications and complications that can happen down the line if a patient isn't treated. 01:09 So if we see a patient in the Emergency Department with lower abdominal pain, burning when they urinate, some other kinds of you know, symptoms related to the GU tract, we wanna make sure that we’re thinking about this diagnosis, because if you missed it the patient can then go on to develop infertility, chronic pelvic pain, and possibly related to ectopic pregnancy development in the future. 01:32 So for all patients who come to the Emergency Department with lower abdominal pain and any kind of GU symptoms that are female, you wanna make sure that you’re doing that pelvic exam. 01:41 You’re thinking about whether or not it could be pelvic inflammatory disease, and then you're asking about the sexual history. 01:49 So what kind of history is the patient gonna tell you? What kinds of things are they gonna be experiencing? Now patients may be reasonably asymptomatic. They might have a little bit of lower abdominal pains, some burning when they urinate to very severe illness. 02:02 Patients can have lower abdominal pain most commonly, they can have fever and systemic symptoms, they can have nausea and vomiting, they can have a lot of discharge, burning when they urinate, dyspareunia. 02:15 So patients can range from really not that symptomatic to being very, very sick. And I've taken care of patients on all kind of ranges within this spectrum. 02:23 Patients who you know, look very well to patients who are very ill and need to be admitted to the hospital for PID. So it’s really a wide range. 02:33 On the physical exam, you may have a patient who have some lower abdominal tenderness, cervical motion tenderness. 02:40 So when you do the cervical exam and you go and you move their cervix, they may experience pain. 02:46 Sometimes, we call that the chandelier’s sign. 02:49 So a patient, when you move their cervix and the pain is so severe that they can almost jump off the bed, and kind of hold on to the chandelier, we call it the chandelier sign. 02:57 And you may also see discharge on exam. 03:00 It might be white, it might be yellow in color. 03:02 You can always ask a patient if they normally have vaginal discharge and if they feel like this looks different. 03:09 On by manual exam, the patient may have adnexal tenderness. 03:12 You may feel a mass if they have a large TOA, tubo-ovarian abscess. 03:17 And then the cervix may be friable. 03:19 So it might bleeding, or appear irritated, or kind of reddish in color. 03:28 PID is a clinical diagnosis. 03:31 Again, I wanna make sure that I'm stressing that for women who are presenting to the Emergency Department with symptoms of lower abdominal pain and GU symptoms, go ahead and think about this. 03:41 Make sure you’re doing that pelvic exam. 03:44 Again, the main test we send off here is the Nucleic Acid Amplification Test for gonorrhea and chlamydia. 03:49 And for a majority of patients we will stop there. 03:52 Now, if your patient appears very ill or is having a lot of adnexal tenderness on one side or the other, you wanna move on and get some additional imaging. 04:01 For the most part we get an ultrasound, 'cause ultrasound is really the best test to look at those GU structures, it’s the best test to look at the uterus, and the ovaries, and the fallopian tubes. 04:11 But if you don’t have ultrasound available, you can also potentially get a CAT scan to take a look for these things. 04:17 On an ultrasound or a CT scan, what you’re looking for is you're looking for is salpingitis. 04:21 You're looking for inflammation around the fallopian tubes, or also passively a tubo-ovarian abscess. You're looking to see if the ovary has an abscess, or is very swollen, or inflamed in that area. 04:36 And for PID, due to significance of sequelae of untreated infection have a very low threshold to treat presumptively based on your patient’s symptoms and history. 04:46 Again, remember that that Nucleic Acid Amplification Test isn’t gonna come back right away. It’s going to be delayed for a period of time, so make sure that you're treating and thinking about this if you think that it’s present. 04:59 Now, uterine or adnexal tenderness or that cervical motion tenderness support the diagnosis. 05:07 So what shall we do for patients who have PID? We wanna make sure that we treat them and we have to sort of figure out if our patient can have outpatient treatment or in-patient treatment. 05:17 The outpatient treatment for PID is ceftriaxone intramuscularly again. 05:22 So similar to what we do for cervicitis. 05:24 And then doxycycline twice a day for 14 days. 05:29 Now, it’s not important that you memorize these doses but it’s important that you remember that you wanna treat for a long period of time. 05:35 You wanna treat your patient for 14 days. 05:39 If you are all concerned for anaerobic cause such as trichomoniasis or another anaerobe, consider adding on metronidazole as well to treat that additionally. 05:51 For in-patient treatment, so some patients need to be admitted and we’ll get to who needs to be admitted in a moment, you can choose with cefotetan plus doxycycline or cefoxitin plus doxycycline. 06:03 So doxycycline is always included in those regimens. 06:07 Now, for the most part many of these patients can go home. 06:11 Who needs to be admitted to the hospital? This is a really key thing. 06:15 So the people who need to be admitted are pregnancy and PID. 06:18 PID and pregnancy is relatively rare and that’s due to the fact that the mucus plug forms very early on in pregnancy. 06:26 So the mucus plug basically blocks the cervix and blocks an infection from getting up into that area. 06:32 But definitely in very early pregnancy, patient’s can develop PID. 06:36 Keep it in mind if you're concerned that a pregnant patient has PID, always involve your OB-GYN consults and more than likely that patient’s gonna need to be admitted for IV antibiotics. 06:49 Patients who have a tubo-ovarian abscess always need to be admitted. 06:53 Sometimes, they need to go to the operating room to get treatment for that and then anyone who has intractable vomiting, so if you're unable to tolerate your oral medications, you're unable to take the doxycycline, you need to be admitted to the hospital. 07:08 And also if a patient has been on oral medications for a few days, so let’s say, you discharge them, they go home, they’ve been talking their medication, they return and they’re still having pain they're still having discharge, they may still be having a fever. 07:22 Those patients also need to be admitted to the hospital. 07:26 A little clinical pearl here is a condition known as Fitz-Hugh-Curtis syndrome, and what this is it’s a peri-hepatitis associated with PID. 07:35 So it’s patients who come in with right upper quadrant abdominal pain and symptoms of PID. 07:41 You wanna think about this diagnosis. 07:43 Patients may have elevated liver function test, they might have pain and tenderness in the right upper quadrant, and this is a hepatitis that's associated with PID. So a liver infection associated with PID.
About the Lecture
The lecture Pelvic Inflammatory Disease (Emergency Medicine) by Sharon Bord, MD is from the course Abdominal and Genitourinary Emergencies. It contains the following chapters:
- Pelvic Inflammatory Disease
- PID Examination
- PID Management
Included Quiz Questions
What is the most common symptom reported in patients with pelvic inflammatory disease?
- Lower abdominal pain
- Epigastric pain
- Low back pain
- Right upper quadrant pain
- Nausea and vomiting
What is the Chandelier sign?
- A whole-body reaction to severe pain provoked by movement of a tender cervix when performing a pelvic examination
- Friable cervix
- Adnexal mass
- Vaginal discharge
- Vaginal bleeding on pelvic examination
What is the test of choice for gonorrheal and chlamydial infections?
- Nucleic acid amplification test
- FTA-ABS
- VDRL test
- Microagglutination test
- Wet mount
What is the empiric treatment for pelvic inflammatory disease?
- Ceftriaxone and doxycycline
- Cefuroxime and azithromycin
- Ceftriaxone alone
- Metronidazole and ciprofloxacin
- Erythromycin and ciprofloxacin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |