Playlist
Show Playlist
Hide Playlist
Pediatric Pneumothorax
-
Slides Pulmonary diseases in older children.pdf
-
Download Lecture Overview
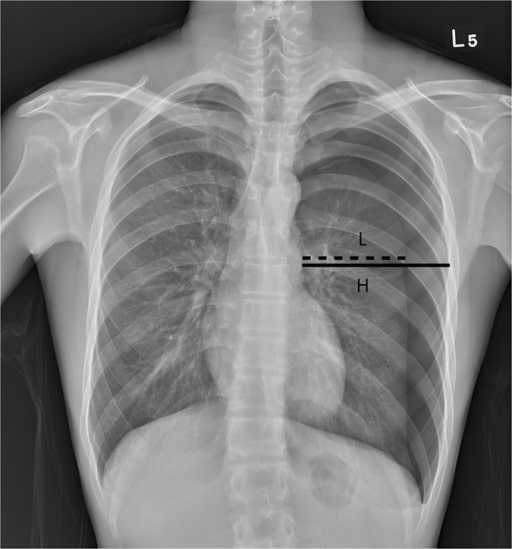
00:01 Let’s close by talking a little about the pneumothorax. 00:07 So pneumothoraxes are a collection of air between the lung parenchyma and the pleural lining on the chest wall. 00:16 They can be spontaneous or they can be traumatic. 00:20 Let’s just pause for a moment and think about lung mechanics. 00:24 When I take a breath in, I expand my chest wall, the air rushes in because I have a vacuum between my lung parenchyma and chest wall and those lungs now expand. 00:35 In a pneumothorax, a hole has been created either externally or internally into that pleural space, such when I breathe in, air can now accrue between the lung and the chest wall. 00:49 So what are some congenital causes of pneumothorax? Well, the CCAM, or congenital cystic adenomatous malformation, can certainly erode into that pleural space and create a conduit for air to get into our pleural space, or a patient may have something like congenital lobar emphysema, where a piece of lung ruptures open and then air can get in. 01:13 Alternatively, later in life, asthma can cause a spontaneous pneumothorax, as can bronchiolitis. 01:20 Both of these are obstructive airway conditions, where children end up hyperinflated or having difficulty getting the air out of the lungs, and that hyperinflation can result in microruptures and air accrual in the pleural space. 01:37 Likewise, foreign body can do the same thing, by acting as a ball valve and allowing for a focal area of hyperinflation. 01:45 And, of course, patients with cystic fibrosis are at risk for pneumothorax for similar reasons. 01:52 In some patients with underlying connective tissue diseases, these patients may have risk of pneumothorax by virtue of the tissues themselves being able to break apart a little bit more easily. 02:06 These are generally conditions where there are problems in collagen. 02:09 Examples are Marfan syndrome or Ehlers-Danlos syndrome. 02:15 Patients with these illnesses are at increased risk for spontaneous pneumothorax. 02:21 Lastly, infections can also cause pneumothorax. 02:24 So, a patient with a lung abscess, or a pneumatocele, or a bronchopleural fistula, these are all examples of where bacteria have chewed through the lung tissue and allowed a way for air to get down and in between the lung and the chest wall. 02:44 So let’s talk about how these patients present and it really depends on the size of the pneumothorax. 02:51 Patients with small pneumothoraces are sometimes asymptomatic and it’s simply found incidentally on chest x-ray. 02:59 These often will resolve on their own and don’t necessarily require any therapy. 03:05 Patients with large pneumothoraxes will generally have a sudden onset pain, especially with deep breath. 03:13 These patients do not want to take a deep breath in because those pleural surfaces are exquisitely tender. 03:21 There’s one kind of pneumothorax that shows up a lot on multiple choice tests, which is the tension pneumothorax. 03:27 This is the pneumothorax in its most severe state. 03:32 If these patients will have profound dyspnea to the point perhaps of altered mental status or may even be in shock, this is a huge pneumothorax that has actually created increased pressure on that side of the chest and is pushing material, like the mediastinum, over towards the other side. 03:52 How do we examine patients and find pneumothoraces? Well, small pneumothoraces typically take up less than 20% of the lung field and you really aren’t likely to detect them on exam. 04:06 You’re not going to hear anything or palpate anything that’s going to look any different. 04:10 In a large pneumothorax, you will see the patient starts having difficulty with breathing, they may have hypoxia either from a lack of inflation of that lung and V/Q mismatch or through voluntary reduction in their respiratory effort as a result of pain, they may have an asymmetric chest rise, especially if there’s trauma or some piece of rib that’s not moving right. 04:36 This is also where you see the flail chest, which is where the chest is moving in a different direction as they breathe. 04:43 In patients who have a large pneumothorax, they will be hypertympanic to percussion. 04:49 Percussion is the lost art of the lung exam. 04:52 Simply percussing on a patient’s chest wall, you’ll hear a hyperresonance that’s typical, almost like that pneumothorax is creating a drum. 05:03 Patients will have decreased or diminished breath sounds in the area of the pneumothorax because that air between the lung and the chest wall is not moving and, thus, you can can’t hear breath sounds through it. 05:16 Tension pneumothorax is critical to appreciate on physical exam because the diagnosis is made exclusively by physical exam and the treatment is fairly severe and needs to be done rapidly. 05:31 In these patients, they will notice tracheal deviation away from the side of the tension pneumothorax. 05:37 The pneumothorax is creating increased pressure and pushing that trachea over. 05:43 You’ll notice shifting of the apical cardiac pulse away from the pneumothorax or farther laterally if it’s on the right side or medially if it’s on the left side. 05:54 These patients will have tachycardia and hypotension from their decreased venous return. 06:01 The blood is having a hard time getting back into the chest because the pressure is so high there. 06:09 On an x-ray, you should be able to make the diagnosis of a pneumothorax. 06:14 It’s a little bit embarrassing to get a chest x-ray and diagnose a tension pneumothorax because you should have made that diagnosis on physical exam and the x-ray was delaying your therapy. 06:26 But in patients where you’re unsure, where there’s not a tension pneumothorax, the x-ray is the way to go. 06:33 Generally, we’ll take an upright because it’s easier to see as air may layer up if they’re supine and you won’t be able to see a contrast between the air and the lung. 06:44 You’ll find the place where there are no lung markings. 06:48 So there’s no lung markings, no those fine little lines, which are invading the area where that pneumothorax is happening. 06:56 It’s pure air. 06:58 Small ones can be subtle. 07:01 Probably, many of you viewers have been looking at this X-ray and thinking, " I don’t see anything." It can be a very subtle thing. 07:10 A tension pneumo is not subtle. 07:12 It would be a little bit inappropriate to get a chest a x-ray, as I said, because you’d be delaying therapy. 07:22 But let’s look a little closer at this x-ray. 07:25 So here’s a close up of the top of this x-ray that I’ve been showing you and maybe you’ve seen it and maybe you don’t. 07:31 I’m going to draw a little line for you right here. 07:35 That line, I’ll take it away, now you can probably see it. 07:40 Do you see that area where there’s that faint line? Above that line, there really are no lung findings. 07:46 None of those fine little lines, but they are present below. 07:50 There’s the line. 07:51 Now it’s gone. 07:56 So, the diagnosis of pneumothorax. 08:00 Well, you’ve made the diagnosis, you’ve said it’s either a small pneumothorax or a large or a tension pneumothorax, and now you want to know what you’re going to do. 08:10 So in a small pneumothorax, such as maybe that one in the last x-ray, we’re not going to do a whole lot. 08:17 We’re going to provide a hundred percent oxygen by a non-rebreather mask. 08:22 This is complicated how this helps, but it probably does. 08:26 A hundred percent oxygen by mouth has no nitrogen in it. 08:31 When we breathe in, about 70% of our air is nitrogen. 08:36 Remember oncotic forces. 08:38 If we now breathe in a hundred percent oxygen, 70% of the air in that pneumothorax is actually nitrogen. 08:46 Now, in the blood, there’s less nitrogen. 08:49 So the nitrogen in this pocket will want to be reabsorbed through osmotic forces. 08:54 Thus, a hundred percent oxygen will allow that to shrink and it probably will let it resolve sooner. 09:02 It’s nice especially to do this in a patient who’s symptomatic. 09:05 But typically these will resolve within in a week. 09:08 We’ll provide oxygen only as long as it takes for them to feel better in the in-patient or the ER setting. 09:14 For a large or a tension pneumothorax, the indication is to immediately decompress the lesion. 09:21 That means we have to get the air out. 09:23 It’s under great pressure. 09:25 So in a tension pneumothorax in particular, we’re going to do that right away. 09:30 This is going to be an emergency needle decompression. 09:33 And then after that decompression, we’ll put in a chest tube and we’ll put that chest tube to suction to allow that lung to remain inflated. 09:44 Now, that lung is going to gradually heal up, the holes will be closed. 09:48 And when there’s no longer drainage of fluid and there’s no longer adequate suction, we’ll put it to water seal, and then eventually remove the chest tube. 09:57 Rarely, the leak persists and that requires surgery to repair the leak. 10:05 After patients are treated with pneumothorax, we have to prevent recurrence. 10:10 So these patients in particular have some unusual limitations. 10:15 First off, no smoking. 10:17 Really, no smoking. 10:19 Second, no deep sea diving. 10:22 Seems unusual, but those increased pressures could cause that patient to redevelop an acute pneumothorax while underwater, which has got to be the worst place to have a pneumothorax. 10:34 And lastly, we need to be careful about letting them fly in unpressurized planes. 10:39 Until they’ve truly healed up, we worry that those could recur. 10:45 So let’s go through how to decompress a tension pneumothorax, this is high-yield information on an exam. 10:52 Basically, you’ve got a patient who’s coming in with a tension pneumothorax. 10:56 Let’s say, as in this case, the patient has tracheal deviation, the patient has absent breath sounds on one side, the patient has a shifted apical pulse of the heart, the patient is in respiratory distress, or is hypotensive, we need to fix this problem immediately. 11:14 So in this case, you’re going to run into the next room and get a large bore angiocatheter or an IV 16, 18 gauge. 11:24 In this patient, we’re going to imagine there’s a right-sided tension pneumothorax; the trachea has deviated to the left, the patient’s apex of the heart is far lateral, they’re in respiratory distress and shock. 11:38 We’re going to find the second intercostal space in the ribs. 11:43 We’re then going to draw an imaginary line down the midclavicular line. 11:48 So find the center of the clavicle and draw a line right -- it’s a little bit past the middle of the lung field. 11:55 Where those two things intersect, you’re going to take that large bore angiocatheter and push it in and remove the needle. 12:02 You should hear an immediate woosh of gas as that highly pressurized air rushes out. 12:09 This patient should feel much better very quickly. 12:13 Then, you’re going to have to go about putting in a chest tube. 12:17 That’s all I have for you today about this particular problem. 12:20 Thanks for listening.
About the Lecture
The lecture Pediatric Pneumothorax by Brian Alverson, MD is from the course Pediatric Pulmonology.
Included Quiz Questions
A patient comes in with acute respiratory distress, midline apical heart beat, trachea deviated to the right, and absent breath sounds over the left lung. What is the next best step in the management of this patient?
- Insert a large gauge needle into the 2nd intercostal space along his left midclavicular line.
- Provide oxygen
- Order a chest x-ray STAT
- Provide albuterol
Which of the following congenital condition can lead to spontaneous pneumothorax?
- Congenital Cystic Adenomatoid Malformation
- Kartagner syndrome
- Patau syndrome
- Asperger syndrome
- Congenital Diaphragmatic Hernia
All of the following findings are specific to Tension Pneumothorax, EXCEPT?
- Prolonged QT interval
- Tracheal deviation
- Hypotension
- Decreased venous return
- Shifting of the apical impulse
A patient with suspected spontaneous pneumothorax is about to undergo chest X-ray. Which view would be the most appropriate?
- Upright and posteroanterior
- Upright and Lateral
- Supine and Anterioposterior
- Supine and Lateral
- Chest X-ray is useless
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Clear classification between small, large and tension. Clear risk factors of spontaneous PNE. All in all, I learned new things to appropriately diagnose and manage PNE.