Playlist
Show Playlist
Hide Playlist
Pain: Definition – Opiates and Sedatives
-
05 - Opiates and Sedatives.pdf
-
Download Lecture Overview
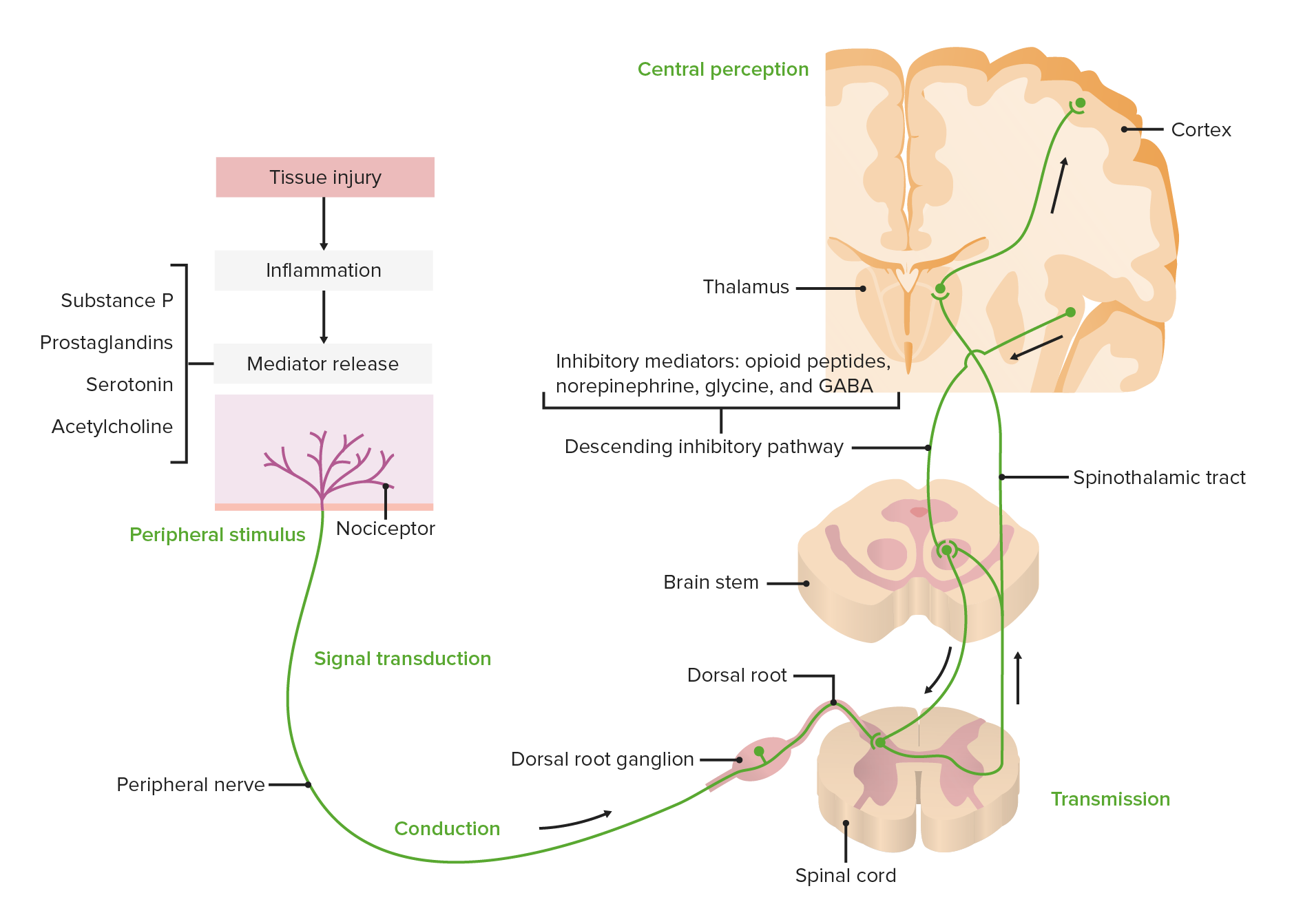
00:06 Hello ladies and gentleman. This is a continuation of our discussions and lectures on Anesthesia. In this presentation we are going to talk about Additional Anesthetic Drugs. And we're going to spend a little time talking about pain, although we'll have a much fuller discussion of the Management of Pain in a future lecture. 00:30 So what is Pain? The International Association for the Study of Pain (IASP), defines pain as an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage. So, when we talk about pain, we often talk as if something had been damaged, even when we don't know that that in fact has happened. So these are some of the subcategories that the IASP has defined, and I'm not going to go through all of these. You can look them up if you wish, but it's a very complex, extensive list of subcategories of pain. And there are variations in treatment depending upon which type of pain an individual suffers from. We're going to talk in more general terms about pain. 01:24 So the IASP states that about 30% of humans suffer from chronic pain at some point in their lives. And chronic pain is pain that lasts for greater than 3 months. 01:36 Some people say greater than 6 months. They further go on to say that about 7% of people are completely incapacitated by chronic pain. It's the most prevalent cause of disability that we have in healthcare. Greater cause, greater cost of disability than cancer and heart disease combined. 02:00 It's universal. It's a human characteristic that exists in every one of us. Perception of pain is not modified by ethnic background, but presentation of pain is affected by the culture from which you come. And let me give you an example of this. I often teach anesthesia residents in Uganda. 02:24 And one of the things I noted the first time I went to Uganda, was how unbelievably stoical Ugandan people are. They never complained about pain, they never asked for drugs. The amount of pain medication given was minuscule. And I thought this was odd, because my understanding was that, we all feel pain the same, it didn't matter what culture we were in. So, I did a little study where we actually went and saw patients postoperatively. And we asked them to give them, to provide a pain score. 0 for nothing, up to 10 for absolutely excruciating pain. And what we discovered was what I expected to discover, is that Ugandans, like everybody else in the world, have pain and they have pain at about the same level as everybody else. 03:12 But culturally, it's not really acceptable for them to show pain. Stoicism is expected. The reality is, they suffer pain just like the rest of us. 03:24 Surgical pain is acute pain. But we must discuss chronic pain, and we will discuss chronic pain in a future series of slides. So pain is not a benign process. Cardiovascular and respiratory systems are significantly affected by the pathophysiology of pain. There's dramatic adrenergic stimulation. 03:48 This is release of Norepinephrine throughout the body and from the adrenal gland. 03:54 Hypercoagulation can occur leading to disseminated intravascular coagulation. 04:00 Heart rate goes up. Cardiac output goes up. Myocardial oxygen consumption goes up, which can lead to myocardial ischemia or myocardial infarction. Pulmonary vital capacity drops because, particularly if you've had an injury to your chest or surgery to your chest, you splint your muscles and you can't breathe deeply. And this can lead to alveolar hypoventilation, reduction in functional residual capacity, atelectasis, pneumonia, and serious problems with arterial hypoxemia throughout the body. Also, pain suppresses immune function, predisposing trauma patients particularly, to wound infections and sepsis. So what are analgesics?
About the Lecture
The lecture Pain: Definition – Opiates and Sedatives by Brian Warriner, MD, FRCPC is from the course Anesthesiology: Introduction.
Included Quiz Questions
Which statement about chronic pain is TRUE?
- It is an extremely common condition.
- It occurs most in people with a "low pain threshold."
- It is easily managed with opioids.
- It requires intervention by doctors only.
- It is usually diagnosed in the first two weeks post-operatively
Which of the following statements about pain is TRUE?
- Everyone can experience chronic pain.
- Pain is caused only after actual tissue damage.
- There are 2 subcategories of pain.
- All types of pain are usually managed by opioids.
- Pain is mainly an unpleasant sensory experience.
Which of the following statements about chronic pain is TRUE?
- It is the most prevalent cause of disability worldwide.
- It is pain that lasts for more than 1 year.
- Its perception is different between people of different cultural backgrounds.
- Approximately 30% of people are completely incapacitated by chronic pain.
- Surgical pain is a characteristic example of chronic pain.
Which of the following is expected to increase when someone is in pain?
- Myocardial oxygen consumption
- Alveolar ventilation
- Arterial oxygen content
- Functional residual capacity
- Effectiveness of the immune system
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This lecture was informative and engaging. The speaker did an excellent job of presenting the material in a clear and concise manner, making it easy to understand.