Playlist
Show Playlist
Hide Playlist
Oncogenes and Tumor Suppressor Genes
-
Slides CP Neoplasia Genetic alterations in malignancy.pdf
-
Download Lecture Overview
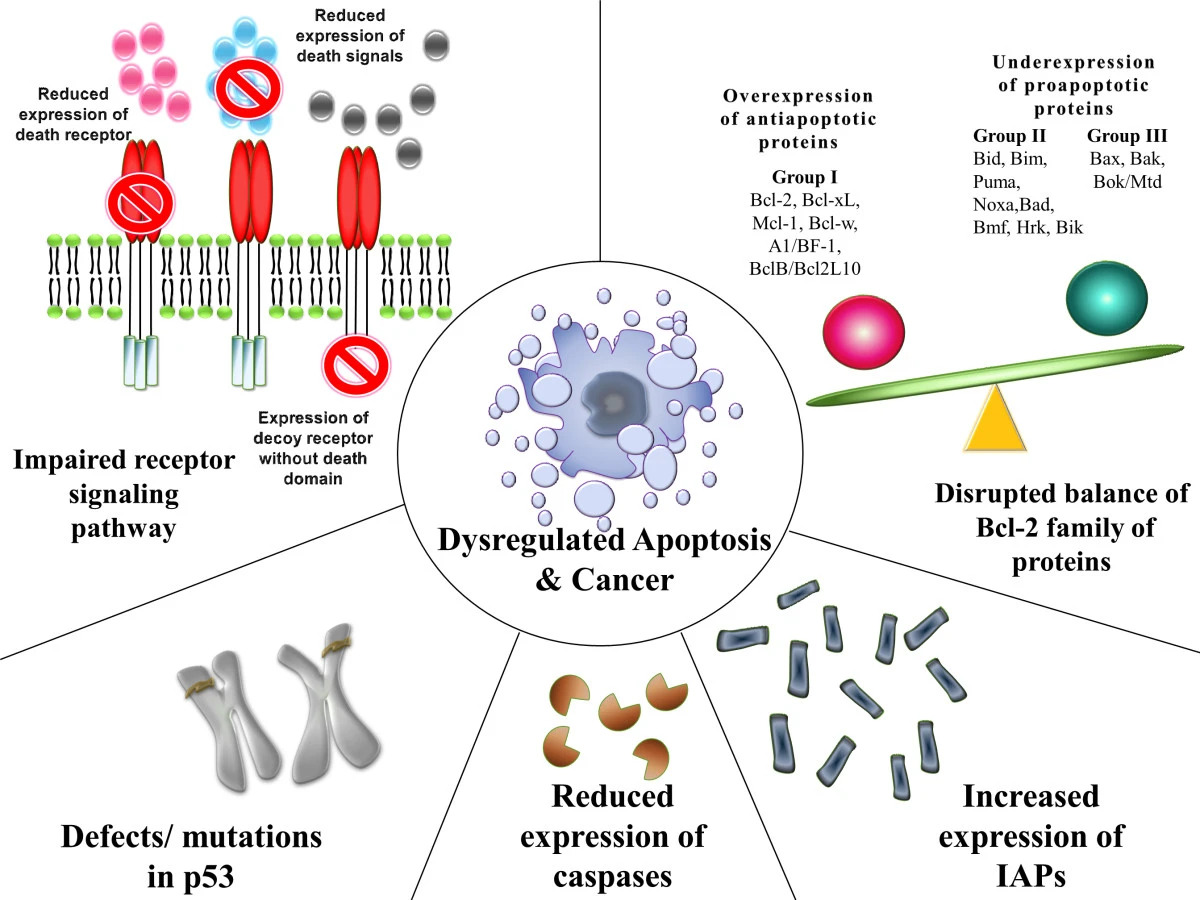
00:00 So, oncogenes. So this is derived from physiologic regulators of cell proliferation, so called proto-oncogenes. And again they are not genes designed to create cancer, they are genes designed to drive the cell through its proliferative cell cycle. They become oncogenes when they become mutated. So for example an EGF receptor, normally it would be a receptor, the epidermal growth factor receptor will be on the surface of a cell and when appropriate ligand binds then it signals for a period of time and then it turns itself off. 00:42 If it doesn't turn itself off, that initial signal continues to occur. There can also be mutations where you don't need the ligand to cause activation to other receptor. So, that's an oncogene. We have now lost the regulatory piece driving cell cycle progression. It can happen when there is chromosomal translocation, so the BCR-able mutation that occurs in chronic myelogenous leukemia that leads to a fusion protein that is constitutively active as a kinase and drives subsequent gene transcription. That's an oncogene. It is driving cells through the cell cycle, but this is by virtue of a chromosomal translocation. And then there's overexpression or amplification. And so you could have something that would be okay at 2 copies per cell but when it gets up to 200 copies per cell then it overwhelms any negative regulatory pathway. So that's another mechanism by which you can have an oncogene. And MYC overexpression and amplification is actually a good example of that. 02:00 So basically with all these changes that can occur in the oncogenes, the accelerator is stuck on. We are going through the cell cycle at a frantic cleave because we never tightly regulate the things driving cellular proliferation. Okay, the accelerator stuck-on. And what that means is that we have gain of growth-promoting activities and usually all it takes is 1 out of the 2 genes for this to happen. So they generally act mutations and oncogenes usually act in an autosomal dominant fashion. All it takes is 1 bad gene and you are often running. Let's locate an example of an oncogene in action. So, the RAS oncogene is a signal transduction molecule. It's going to be kind of that orange box-like thing that is there. 02:54 Normal activation of the cell requires a growth factor binding to the growth factor receptor. 02:59 There will be some bridging proteins that interact then with the RAS oncogene. And normally at baseline if a cell is not going through cell cycle, RAS is an inactive form. What is actually bound there, the green pentagon with the 2 little dots associated with it is a GDP molecule. 03:20 So it's got 2 phosphate groups, G diphosphate. And that is anchored in the membrane. 03:27 When a growth factor comes in and stimulates the receptor through the bridging protein, we get activation of the inactive RAS. And whenever you might inactivation is that we kick out the GDP that was in there and we bring in a new fresh GTP, a triphosphate group. 03:47 And that will allow then the RAS protein that has now become activated to interact with other proteins and will drive the subsequent transcription translation of various proteins it allows to go through the cell cycle. So that's the normal pathway. Well how does that normally turn off? Well it normally turns off because RAS has a built-in timer where over a period of time it's going to cause the loss of a phosphate group and then we will have just GDP bound which is inactive, which makes for an inactive RAS. So that would be the normal pathway that turns off and it's usually kind of on a very carefully regulated clock. That active RAS is that thing for a while until it hydrolyzes one of the phosphates off the GTP to make GDP and now we're back to inactive. That's perfect, that's the normal regulatory pathway. And we get one round of replication from that growth factor. But if there are mutations in RAS, say it loses its ability to hydrolyze the GTP, now everytime it gets turn on I don't get that feedback inhibition and I get upregulated expression and ongoing expression of everything that's going to drive cell cycle progression. Okay, so we've talked about the accelerator being turned on, let's talk about the break being turned off. Those are the tumor suppressor genes. So tumor suppressor genes are regulators of normal cell division. 05:21 We have talked about them, it's p21 and p53 and retinoblastoma. If we lose that function via mutation, then there will be inadequate inhibition of cell cycle progression. That eliminates the break mechanism. We can no longer tempt down the runaway train that is going to be the cell progressing through its cycle. So we' lose checkpoint control and importantly as opposed to the oncogenes which act in an autosomal dominant fashion, one bad gene is sufficient to drive the process. Tumor suppressor genes in general act in a recessive manner. So both genes need to be affected in order to have loss of the breaking function. 06:12 So it will require dual mutations in both genes. And so examples of this are the Rb protein, Np53 protein. So, let's review retinoblastoma very briefly. There are germline mutations in the familial form of retinoblastoma. In this particular case, that has a mutant blue allyl of the retinoblastoma protein, the Rb protein. That means in half of his germ cells, half of them contain that Rb mutation that's going to make it inactive. And so if one of those mutant genes is part of the zygote, then all cells of the child, all somatic cells of the child will have 1 mutant copy. And then if by chance the other Rb protein becomes mutated, we develop retinoblastoma. We've talked about some of that previously. Okay, so it requires a germline mutation in retinoblastoma and 1 single new somatic mutation. If we're talking about the sporadic form of the disease, mom and dad here are both completely normal, everyone has got the red normal retinoblastoma genes. The zygote all completely normal and the somatic cells initially all completely normal, but the mutation randomly in a retinal cell now means that the progeny of that one Rb mutation which by itself is not a problem, that progeny of one of the progeny cells gets a 2nd mutation. Now we're off and running again with the retinoblastoma. Talk about p53 germline mutation. This is the Li-Fraumeni syndrome. So, these patients have defective p53 regulation of the cell cycle because they have mutant p53 and they are prone to a variety of malignancies. So, in our normal cell where p53 is normal, we have some sort of radiation damage, carcinogens, mutations, whatever, we get DNA damage, we get upregulation of p53 which will then drive inhibition of the cyclin CDK process through p21 will hopefully initiate repair through the Gadd45 and if both of those are not successful, it will induce apoptosis, genes that are important in apoptosis. Okay, that's the normal pathway and that's what normally happens; however, if p53 is in some way mutated and is not able to do its job, then now we have DNA damage occurring. Those p53-dependent genes, you now the p21, the Gadd45, the box apoptotic genes are not activated. And now there is no cell cycle arrest, there is no DNA repair, there is no cell death. We get mutant cells that refuse to die, acquire additional mutations and now we have malignancy. So you can see from the retinoblastoma example and also the p53 example how loss of the breaks can cause malignancy.
About the Lecture
The lecture Oncogenes and Tumor Suppressor Genes by Richard Mitchell, MD, PhD is from the course Neoplasia.
Included Quiz Questions
What is an example of a chromosomal translocation event that turns a proto-oncogene into an oncogene?
- BCR-ABL
- EGFR
- MYC
- p53
- p21
What binds to RAS in the inactive state?
- GDP
- GTP
- ADP
- ATP
- AMP
Which of the following is a tumor suppressor gene that can be mutated to contribute to cancer?
- RB
- p21
- MYC
- EGFR
- BCR-ABL
What physical examination finding defines leukocoria?
- A white pupil
- A white retina
- A white iris
- Delayed reflexes
- Hyperreflexia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |