Playlist
Show Playlist
Hide Playlist
Neurofibromatosis Type 1: Clinical Presentation
-
Strowd CNS Tumors Inherited Tumor Syndromes.pdf
-
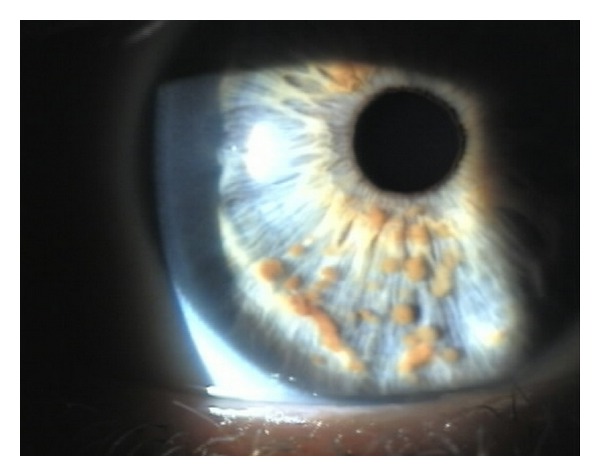
Download Lecture Overview
00:01 What are the common clinical symptoms, clinical scenarios, and presenting features in NF1 patients? Well, the first thing to think about is Cafe-au-lait macules. 00:10 And that's the most common initial symptom that is present in these patients. 00:15 Cafe-au-lait macules, as you see here on the image on the far left, are well circumscribed, that sharply demarcated hyperpigmented lesions. 00:24 We heard that greater than six is sufficient to establish the diagnosis and that's based on this really neat study performed back in the 1990s, that showed that the likelihood of making a diagnosis of NF, which you see on the Y axis. 00:38 It increases with an increased number of cafe-au-lait macules. 00:41 In fact, in patients who had six or more cafe-au-lait macules, almost 80 to 100% of them were diagnosed with NF1. 00:48 In contrast, patients who had less than six cafe-au-lait macules, none of those patients were diagnosed with NF1. 00:55 So we all can have a birthmark. And that's no problem. 00:58 We can even have two, or three, or four. 01:00 But patients who have six or more cafe-au-lait macules or birthmarks, that should tip us off to look for other clinical features of NF1. 01:08 The most common second feature that we'll see is depicted here. 01:12 This is axillary, an inguinal freckling. 01:15 Freckling, where the sun doesn't shine. 01:17 That's not typical. Freckles can happen anywhere, and the shunt <inaudible> can contribute to those, but not commonly in the axilla or inguinal area. 01:26 So freckling in those areas should tip us off that that's not the sun that caused that freckle, that may be a genetic condition, like NF1. 01:33 And it turns out, that's the most common second contributing factor that contributes to the diagnosis of NF1. 01:42 The other thing to think about is the eyes. 01:43 And here we see depicted a Lisch nodule, which is called an iris hamartoma. 01:48 This is basically a cafe-au-lait macule that's on the iris, that outer part right around the pupil. 01:54 The thing that we see with color. 01:57 Here we can see several browns spots, hyperpigmented lesions in the iris, and these are iris hamartomas, Lisch nodules. 02:05 Those are very uncommon in young kids. 02:08 And we can see here at individuals, the age of between zero and two, very few patients have Lisch nodules. 02:15 But by the time that a patient is 21, almost 90% of NF patients will have a Lisch nodules. 02:21 So in adults, this is a really helpful clinical sign. 02:25 And an eye exam is a very helpful examination to establish a diagnosis of NF1 in adults. 02:32 What other things do we see in patients? We'll walk through neurofibromas. 02:36 That second clinical criterion was a neurofibroma, a tumor of the nerve. 02:42 The nerves are in all parts of the bodies. 02:44 The deep nerves are named inside the body and tumors of those deep nerves we call plexiform neurofibromas. 02:51 The nerves then travel outside all the way to the surface of the skin, and tumors can develop anywhere along the path of that nerve. 02:58 The nerves that are out on the very surface of the skin, tumors that develop in those nerves we call cutaneous neurofibromas. 03:04 They're soft, they're fleshy, they're pedunculated. 03:07 You can see them, and feel them, and squeeze them, and it will cause no pain. 03:11 And those cutaneous neurofibromas can be cosmetically unappealing, but it have no risk of malignant transformation. 03:17 They won't become a cancer. 03:20 The second type of neurofibroma that we see are subcutaneous neurofibromas. 03:24 These develop in the dermal layer of the skin just below the epidermis. 03:28 They're still tumors of the nerves, but they develop slightly lower. 03:33 And they cause, they push out on the surface of the skin and you see this bump that could be painful. 03:39 They're not soft and fleshy, like the cutaneous neurofibromas, but you can feel them, and push on them, and it may cause pain. 03:46 And those nodules are occurring deeper underneath the skin. 03:49 They're also can be cosmetically unappealing, they can be painful, or in areas that cause problems like the belt line or where you hold a pin, and could be surgically removed for those reasons. 03:59 But there is also no malignant potential for those subcutaneous neurofibromas, like you see here. 04:06 The last type of neurofibroma is a plexiform neurofibroma. 04:10 These are also tumors of the nerves just like each of the ones that you see. 04:15 But these tumors are occurring deep in those deep highways of nerves that are occurring in the arms, typically legs, or sometimes in the face. 04:23 They occur in the name nerves. 04:25 And you can see here, a large plexiform neurofibroma running the length of the sciatic nerve in this patient's leg. 04:32 The tumor begins in the nerve and starts in the nerve, but you can see here expands all the way out to the surface of the skin. 04:38 And likely involves the bone, the fascia, the muscle, and all tissue in between. 04:44 Tumors like this extensive tumors cannot be surgically removed. 04:48 And for many years, our field is searched, for treatments for this, and we'll talk about some treatments that are emerging at the end of this talk. 04:56 Here's another example of neurofibromas, or rather severe case of neurofibromas. 05:01 Cutaneous neurofibromas out on the skin. 05:03 And you can see these nerves that go to the surface of the epidermis have just grown, and there's unregulated growth. 05:09 Loss of neurofibromin, loss of that NF1 gene has result in unregulated growth, and there are multiple tumors occurring on the skin. 05:17 These are not painful, but can be very cosmetically unappealing and difficult in terms of this patient's dressing and other functions, and would be removed for those reasons. 05:28 What other manifestations do we see? Well, here, we'll walk through some of the bony abnormalities that can occur as a result of abnormal bone growth. 05:37 And the two that I want you to think about are sphenoid wing dysplasia, and a tibial bone fracture with pseudarthrosis. 05:44 Here on the left, you see a great example of sphenoid wing dysplasia. 05:48 The sphenoid wing is that bone that sits just beneath the temporal lobe in the middle cranial fossa, right behind the maxillary sinus. 05:56 And we can see here increased bony deposition, both along the convexity of the brain on the far left. 06:02 You see that osteophytic complex, as well as in the sphenoid wing to the right. 06:07 And this is a good example of sphenoid wing dysplasia. 06:10 Similar to some of the other patients we've seen, that abnormality starts in the bone, but if you look to the tissue that's in the CT scan out to the surface, you can actually see that the entire right face is enlarged and involved in this tumor, which can make it very difficultly to surgically treat. 06:26 The other bony abnormality that establishes the diagnosis of NF1 is tibial bone fracture with pseudarthrosis. 06:33 This is a tibial bone that has been incorrectly formed, it is weak, as a result of all those NF1+/- cells that are haploinsufficient. 06:43 They have one NF1 copy, but that mutation is insufficient for normal cell growth. 06:48 And so the bone is weak and can break. 06:50 And this patient has suffered a tibial bone fracture that has been unable to heal. 06:55 And as a result of that inability to heal, we see a false joint. 06:58 It looks like a joint in the middle of the tibia and fibula, but it's not. It's where a normal bone should be. 07:05 And this is a diagnostic criterion for NF1. 07:09 Lastly, let's think about some of the things that can form in the brain. 07:13 And the classic tumor that develops in the brain is listed here. It's an optic pathway glioma. 07:19 These are pilocytic astrocytoma. 07:21 They're those grade 1 low-grade tumors. 07:24 and they're very common occurring in about 20% of NF1 patients. 07:30 We'll walk through what they look like on imaging. 07:32 Here we see the appearance of a left optic pathway glioma on this T1-weighted precontrast imaging. 07:39 They show up as dark on the T1. 07:42 We see some brighter signal on the T2 image highlighting this optic nerve. 07:46 This enlarged thickened sausage like optic nerve in this patient on the left optic nerve. 07:54 And they enhance avidly with contrast. 07:56 And we see here on the T1-weighted postcontrast image have an enhancement on the entire length of this left optic nerve. 08:03 Many of these patients will present with vision loss and that's a common presenting feature of an optic pathway glioma. 08:09 But it turns out about 60% of patients will not suffer any symptoms from this tumor. 08:14 About a third of those patients can be watched. 08:16 A third of the patients may need treatment for this, but have normal visual function and no symptoms. 08:22 So important for these patients to be evaluated by a multidisciplinary team. 08:28 There are many manifestations of NF1, how do we keep them all straight? Well, not all of those symptoms we see in every patient. 08:36 And it turns out that the clinical manifestations of NF1 vary over the course of life. 08:42 In infancy, we think about Cafe-au-lait macules. 08:45 They are the most common presenting symptom. 08:47 And so when young children, pediatricians, and other providers should think to look for cafe-au-lait macules. 08:53 And an NF1 patient will have almost all of their cafe-au-lait macules, by two years of age. 08:58 And so that's the first thing we look at. 09:00 During childhood, we look at other clinical features that can help us to establish that second criterion and make the diagnosis of NF1. 09:07 And typically we're looking for axillary and inguinal freckling, vascular abnormalities in the optic pathway glioma. 09:14 Patients who develop an optic pathway glioma typically will develop that before the age of seven or 11. 09:20 And after the teenage years, there's no likelihood of that tumor that optic pathway glioma contributing to vision loss or other symptoms. 09:28 In puberty, therefore, we look at other things. 09:30 We worry about bony abnormality until the bones have formed. 09:34 And the growth plates have solidified. 09:37 Neurofibromas often start to develop during puberty, and can develop all throughout the entirety of life. 09:43 New ones can occur, and the ones that patients have can increase in size. 09:47 We saw how Lisch nodules are uncommon in young children, but increased with age, and by the time of 19, 20, 21, the vast majority of NF1 patients will have evidence of Lisch nodules. 09:58 And then in adulthood, we about other things. 10:01 We worry about vascular abnormalities, and high blood pressure from pheochromocytomas. 10:05 There's an increased risk of early onset breast cancer that all patients should be screened for. 10:09 And we worry about some changes with vision and early onset cataracts. 10:13 All throughout life, we see learning disabilities, and about 75% of patients. 10:17 That's really important to screen for monitor throughout the entirety of these patients course.
About the Lecture
The lecture Neurofibromatosis Type 1: Clinical Presentation by Roy Strowd, MD is from the course CNS Tumors.
Included Quiz Questions
Which of the following is a dermatological finding of neurofibromatosis type 1?
- Café au lait macules
- Port-wine stain in the dermatomal region of the trigeminal nerve
- Ash-leaf spots
- Shagreen patch
- Ungual fibromas
On what part of the body might patients with neurofibromatosis type 1 demonstrate freckling?
- Inguinal area
- Scalp
- Shoulders
- Abdomen
- Cheeks
Which of the following is an ophthalmological finding of neurofibromatosis type 1?
- Lisch nodules
- Cataracts
- Uveitis
- Amblyopia
- Kayser–Fleischer rings
Which of the following tumors is associated with neurofibromatosis type 1?
- Optic glioma
- Vestibular schwannoma
- Cardiac rhabdomyoma
- Angiomyolipoma
- Subependymal giant cell astrocytoma (SEGA)
Adults with neurofibromatosis type 1 should be screened for which of the following cancers?
- Breast cancer
- Ovarian cancer
- Testicular cancer
- Lung cancer
- Skin cancer
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |