Playlist
Show Playlist
Hide Playlist
Myelodysplasia – Hematopoietic Malignancies and Aplastic Anemia
-
Slides Other haemopoietic malignancies and aplastic anaemia.pdf
-
Download Lecture Overview
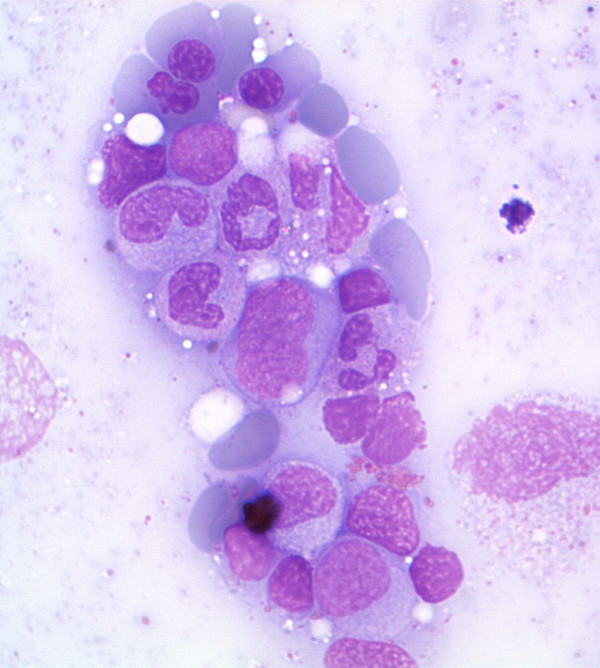
00:01 Hello, In other lectures, we focused on leukaemia and lymphoma, but now I want to focus on other haemopoietic malignancies and aplastic anaemia. We will learn in this lecture, the myelodysplasia and myeloproliferative disease are clonal disorders of the myeloid lineage within the bone marrow. Myeloma is a malignant disorder of plasma cells and is treated with a wide range of novel therapies. And finally aplastic anaemia results in the loss of stem cells in the bone marrow and may result from an autoimmune process. 00:43 Let us start with myelodysplasia, break the word down myeloid bone marrow, dysplasia dysplastic or deficient function of the bone marrow. This is a group of disorders, which are clonally derived of a haemopoietic stem cell and they are characterized by bone marrow failure in association with dysplastic features in one or more cell lineages. What do I mean by that? What does dysplastic mean? It means that the cells when we look at them at the microscope display abnormal features. Let me show you by moving to the right-hand side of the screen, you will see three figures there. On the top left, believe it or not, these are neutrophils, but they do not look like normal neutrophils, I hope you agree. They are hypergranule. 01:39 We do not see the granules that you see in the normal neutrophil and they are also not so heavily lobed, just two lobes. So these are dysfunctional neutrophils. On the top right an unusual cell is a megakaryocyte in the bone marrow, but again very abnormal looking not enough nuclei much small of the normal of the very prominent cytoplasm. And at the bottom, that is a special stain for iron in erythroblasts in the bone marrow and you will see around the red nucleus ring of iron material sideroblasts and we will talk about that in the next couple of slides. You can see this is a disorder characterized by a very proliferative bone marrow producing very abnormal cells. This is due to the accumulation of a range of DNA mutations and epigenetic modifications in the haemopoietic stem cells. It is often seen in people who are quite elderly and therefore it can be regarded as a premalignant and also . . . malignant in some cases disorder of the haemopoietic stem cell. 03:01 The classification of myelodysplasia is really quite complicated. We do not need to go into it in great detail in this lecture, but there are a few points to help you. You may get these dysplastic changes just in one lineage down the red cells leading to refractory anaemia or in the neutrophils or platelets or there may be two or more lineages involved and I think you can understand that the more lineages involved the worst the outlook is liked to be. Occasionally this erythroid dysplasia can be associated with those ring sideroblasts that I showed you on the previous sites surrounding the nucleus. That is the specific type of disease with a very common mutation in the gene SF3B1. If the blast cell count or the leukaemia count is increased in the bone marrow, then the diagnosis is called refractory anaemia with excess blasts and that is moving towards acute myeloid leukaemia that is very worrying because that is a difficult disease to treat. A special subtype is the 5q- syndrome. 04:16 This is more common in women and typically there is a macrocytic anaemia or red cells with increased platelet count and as the name suggests this disorder is diagnosed by having a karyotype or a chromosomal spread of the tumor and recognizing loss of the long arm of chromosome 5 and finally if the monocyte count is raised above the level of 1 x 10 9 it is a chronic myelomonocytic leukaemia. So I do not think you need to retain all the details of this classification, but you can see some of the principles of this quite heterogenous disorder. Now how this disorder is were presented clinically? How is it present within patients? I said already that it is mainly a disorder of all the patients and the main clinical problems arise because the blood count is reduced. The haemoglobin is down leading to anaemia. The white cells are down leading to infection and the platelets are dysfunctional leading to bleeding. 05:24 I have just brought two slides there to show you the top you can see small bruises or purpura, very characteristic of people with low platelet counts or dysfunctional platelets and on the right a chest x-ray showing an area of infection. So like many hematological disorders, myelodysplasia is diagnosed on the basis of the histoexamination together with the blood count and the bone marrow and cytogenic analysis. Now we tend to divide myelodysplasia into patients low risk on patients at high risk. What do we mean by this? Well, low risk patients are likely to survive longer. We do not need to treat them quite as rapidly and in fact we often use different therapies whereas high-risk disease is very worrying, which I will show you in the next slide and scores were revolved where we use a range of different measurements to divide patients into these risk groups as you will see at the top. Patients with less than 5 percent blasts or leukaemic cells in the bone marrow and only one cytopenia and relatively feeble genetic damage are diagnosed as low-grade myelodysplasia. We tend to use supportive treatment, blood transfusions. We can give erythropoietin and similar drugs as well as growth factors such as Granulocyte-colony stimulating factor. The 5q- syndrome is well treated by a drug called lenalidomide and that is interesting in a special case. 07:16 At the bottom those, one example of these risk scores that can be used to assign patients to low or high risk group and you will see on the left the prognostic variables that are used the percentage of bone marrow blasts, the type of karyotype or chromosomal damage and also the cytogenetic. High-risk myelodysplasia is seen in patients who have very poor prognostic genetic change or they have a high number of blast counts in the bone marrow and are progressing towards the acute myeloid leukaemia. This is high-risk disease and the outlook is poor. Intensive chemotherapy such as it is used for acute myeloleukaemia can be used although the outlook with that is not very good because it tends to only control the disease for short periods of time. Azacytidine is an interesting demethylating therapy, which is valuable in some cases and finally we will only achieve cure really through the use of an allogeneic stem cell transplant particularly in the younger patients.
About the Lecture
The lecture Myelodysplasia – Hematopoietic Malignancies and Aplastic Anemia by Paul Moss, PhD, OBE, FMed, FRCPath is from the course Hematologic Disorders.
Included Quiz Questions
Which of the following anemias is 5q syndrome associated with?
- Macrocytic anemia
- Normocytic normochromic anemia
- Microcytic hypochromic anemia
- Hemolytic anemia
- Pernicious anemia
Which of the following statements is FALSE regarding myelodysplastic syndrome?
- Ring sideroblasts are erythroblasts showing a ring of copper deposits around their nuclei, seen with a special stain.
- Myeloid dysplasia of more than one lineage of dysplastic cells is a bad prognosis.
- Anemia, neutropenia, and thrombocytopenia are seen in myelodysplastic syndromes.
- Myelodysplastic syndromes can be pre-neoplastic.
- If the monocyte count is more than 1x10⁹/l it is considered chronic myelomonocytic leukemia.
Which of the following is the treatment of choice for 5q- syndrome?
- Lenalidomide
- Furosemide
- Nesiratide
- Methotrexate
- Cyclophosphamide
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text