Playlist
Show Playlist
Hide Playlist
Myasthenia Gravis: Clinical and Serological Tests – Diagnosis
-
Slides Strowd Myasthenia Gravis.pdf
-
Download Lecture Overview
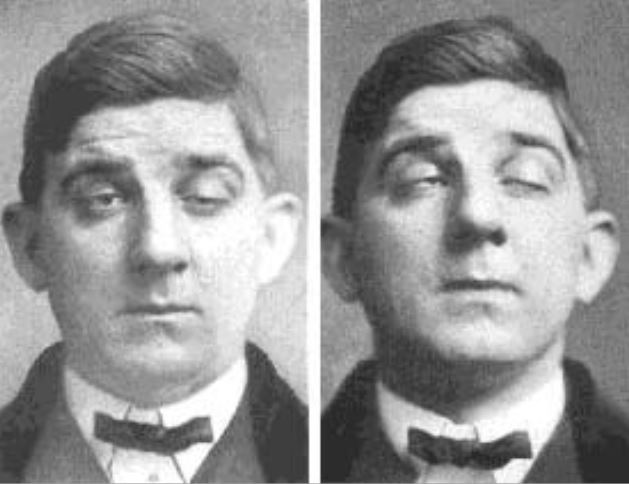
00:01 How do we evaluate patients? What do we do on exam? How do we use provocative testing? And what laboratory studies should we consider to work up a patient who were concerned may have myasthenia? Well, the first is we perform a comprehensive neurologic exam. 00:16 Looking for signs of weakness and fatigability. 00:19 If we see the presence of ptosis, there's two really neat examination techniques that can evaluate that ptosis and point to that problem being from the neuromuscular junction. 00:30 And so these tests are performed when there is prominent bulbar weakness or prominent ptosis. 00:35 The first is the ice-pack test. 00:37 This is a really neat test. 00:39 And we're looking for resolution of ptosis. 00:42 So we saw those images of patients whose eyes were closed, and we place an ice-pack, and we see that the eye opens. 00:49 Why does this happen? Well, it turns out when you cool down the neuromuscular junction, this improves neurotransmission. 00:56 And so we see better acetylcholine quanta released into the neuromuscular junction, and better depolarization of muscles. 01:04 To perform this test, a patient is put at the bedside, we get a cold ice-pack and place it over the eye. 01:12 After about a minute, we look for rapid resolution of ptosis. 01:16 And this occurs quickly and needs to be evaluated quickly after performing this test. 01:21 The second neat bedside test that can evaluate for the presence of a junctional disorder is the edrophonium test. 01:27 This is also called the Tensilon test. 01:29 And again, we're looking for resolution of ptosis. 01:33 This is a medication that can improve transmission at the neuromuscular junction. 01:37 And so we're also looking for the presence of ptosis prior to the test that resolves immediately after. 01:44 What about serologic testing? What studies can we do to evaluate for myasthenia gravis? Well remember, myasthenia is an inflammatory disorder. 01:53 It's an autoimmune condition. 01:55 And it's characterized by the presence of autoreactive antibodies. 01:59 So we're going to look at those in the circulating system. 02:03 The serologic studies that are performed include looking for acetylcholine receptor antibodies, anti-MuSK, the muscle specific kinase antibodies. 02:12 And there are some other increasingly described antibodies that we'll talk about. 02:16 And we can categorize the myasthenia as seropositive in patients who have the presence of one of those antibodies, and seronegative in those that have a clinical presentation consistent with myasthenia but the absence of antibodies. 02:31 So let's look a little bit closer at the postsynaptic acetylcholine receptor. 02:36 Myasthenia is characterized by antibodies that bind to recognize an auto react to this receptor. 02:43 And we can see antibodies that bind to many of these areas. 02:47 Here you can see the extracellular space, the sarcolemma, which is the cell membrane of the muscle and the muscle tissue itself. 02:55 The acetylcholine receptor lies on this membrane recognizes acetylcholine quanta in the synaptic cleft, and results in activation of the muscle as a result of bringing sodium in to the muscle cell. 03:08 Acetylcholine receptor antibodies bind to this receptor and result in the loss of function inability to bring sodium into the muscle and activate the muscle for contraction. 03:18 The second antibody that we see is the antibody to MuSK. 03:21 And you can see the MuSK component of this acetylcholine receptor here. 03:25 A docking enzyme that's critical for its action. 03:29 So let's look a little bit closer at the types of myasthenia based on serologic testing. 03:33 And understand the features of those antibody tests. 03:37 Well, acetylcholine receptor antibodies are present in the vast majority of myasthenics. 03:42 80% of myasthenics will find the presence of acetylcholine receptors. 03:47 And there's a 20% remission rate, which is great. 03:50 We also see acetylcholine receptor antibodies in patients with ocular myasthenia. 03:55 That myasthenia that has a predilection for the bulbar fibres and really ptosis with an absence of generalized weakness. 04:03 Anti-MuSK antibodies are the second antibody that we test for. 04:06 And these we find in approximately 30% to 40% of patients who don't have acetylcholine receptors. 04:13 So our test initially is to look for acetylcholine receptor antibodies. 04:16 And if positive a diagnosis of myasthenia is made. 04:19 If negative of the physician or clinician should consider testing for MuSK antibody positive myasthenia. 04:26 There's a smaller chance of remission rate with MuSK antibody myasthenia. 04:30 And patients often have more prominent ocular symptoms with a paucity of systemic complaints in some of these patients. 04:37 The last antibody that we can look for is the anti-striational protein. 04:41 And this is present in 80% of thymomatous myasthenia gravis or myasthenia gravis that occurs in a patient with a thymoma, and 30% of nonthymomatous myasthenic patients. 04:52 And these antibodies are slightly less specific than acetylcholine receptor and MuSK antibody myasthenia. 04:58 About 15% of patient will not have the presence of circulating antibodies and will be defined as seronegative myasthenia gravis. 05:07 So we have to trust our examination Patients who present with typical findings of a junctional disorder and have other testing that's consistent with a junctional problem can be diagnosed with myasthenia even in the absence of circulating antibodies. 05:21 What other diagnostic tests can be performed? Well, one that we rely on heavily in neurology is the EMG nerve conduction study. 05:30 And this stands for electromyography, which is looking at the muscle specifically with a needle and nerve conduction velocity testing, which is shocking nerves to see how they communicate. 05:41 You can see both of these tests here. 05:42 The picture on the bottom is demonstrating a nerve conduction velocity examination. 05:47 We take a probe and put it where a nerve is at the surface of the skin. 05:52 And we shocked both a sensory nerve or a motor nerve and see what happens. 05:56 For the sensory nerve, we're looking at conduction up that sensory nerve, and seeing how fast the conduction is. 06:02 And looking at the myelination of the sensory nerve and the number of axons in the sensory nerve to look for problems in nerve transmission. 06:10 We can also look at motor nerves, and we shock a motor nerve, and look at contraction of the muscle. 06:16 And that helps us to look at both the motor nerve, the neuromuscular junction, and the integrity of the muscle as well. 06:23 In the top picture, we're looking at an EMG or electromyography. 06:27 And this is where we take a small needle and put it into a muscle and record the signal around that muscle. 06:32 We can look for problems where nerves are not innervating muscles, or where muscles could be damaged. 06:39 When we're evaluating a neuromuscular junction disorder, when critical EMG nerve conduction test is repetitive stimulation. 06:46 And this is a special technique a way to do nerve conduction to look at repetitive activation of a muscle, to see the problem in the neuromuscular junction. 06:56 We see problems with repetitive stimulation about 90% of patients who have a neuromuscular junction disorder and specifically myasthenia gravis. 07:05 And the last test that we can look at is called Single-fiber EMG. 07:09 And this was looking very specifically not at the entire muscle itself, but individual neuromuscular junctions looking for problems with transmission across the junction, and that's called jitter. 07:20 And the presence of jitter on a single fiber EMG is highly specific for a diagnosis of a junctional disorder and is seen in patients with myasthenia gravis in up to 96% to 99% of those patients. 07:33 So these are the tools in our armamentarium to evaluate patients who have weakness that appears to be from a neuromuscular junction condition.
About the Lecture
The lecture Myasthenia Gravis: Clinical and Serological Tests – Diagnosis by Roy Strowd, MD is from the course Disorders of the Neuromuscular Junctions.
Included Quiz Questions
Muscle contraction is the final result of what activity in the sarcolemmal membrane initiated by recognition of acetylcholine by the AcH receptors?
- An influx of sodium into the muscle cell
- An influx of acetylcholine into the muscle cell
- An influx of potassium into the muscle cell
- An influx of calcium into the muscle cell
- An efflux of chloride ions out of the muscle cell
Which of the following best describes the function of the MuSK enzyme?
- It is a docking enzyme for the acetylcholine receptor that can be disrupted in some forms of myasthenia gravis.
- It is a subtype of the acetylcholine receptor that is directly stimulated by acetylcholine.
- It is an enzyme responsible for the degradation of acetylcholine receptors.
- It is a SNARE protein involved in the release of acetylcholine into the synaptic cleft.
- It is an enzyme that can cause a false-positive VDRL/RPR.
Which of the following statements about myasthenia gravis serologic testing is true?
- Patients who are anti-MuSK Ab positive have a smaller chance of remission than AChR Ab-positive patients.
- Anti-MuSK Ab are present in about 80% of myasthenics.
- AChR Ab are more commonly associated with ocular findings without systemic complaints.
- Anti-MuSK Abs are present in over 50% of patients with AChR Ab-negative testing.
- AChR Ab-positive patients have a 50% chance of remission.
Which of the following is not a characteristic finding in myasthenia gravis?
- Muscle weakness is exacerbated by the ice pack test.
- There is a decrement in muscle contraction with repetitive stimulation measured by EMG/NCV.
- Anti-striational antibodies are present with a thymoma.
- The symptoms are reversed with the edrophonium test.
- There is "jitter" on single-fiber EMG.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Muy completa. Buen repaso sobre la Miastenia (presentación clínica, test..)