Playlist
Show Playlist
Hide Playlist
Müllerian Duct Anomalies (MDA)
-
Slides Mullerian Anomalies.pdf
-
Download Lecture Overview
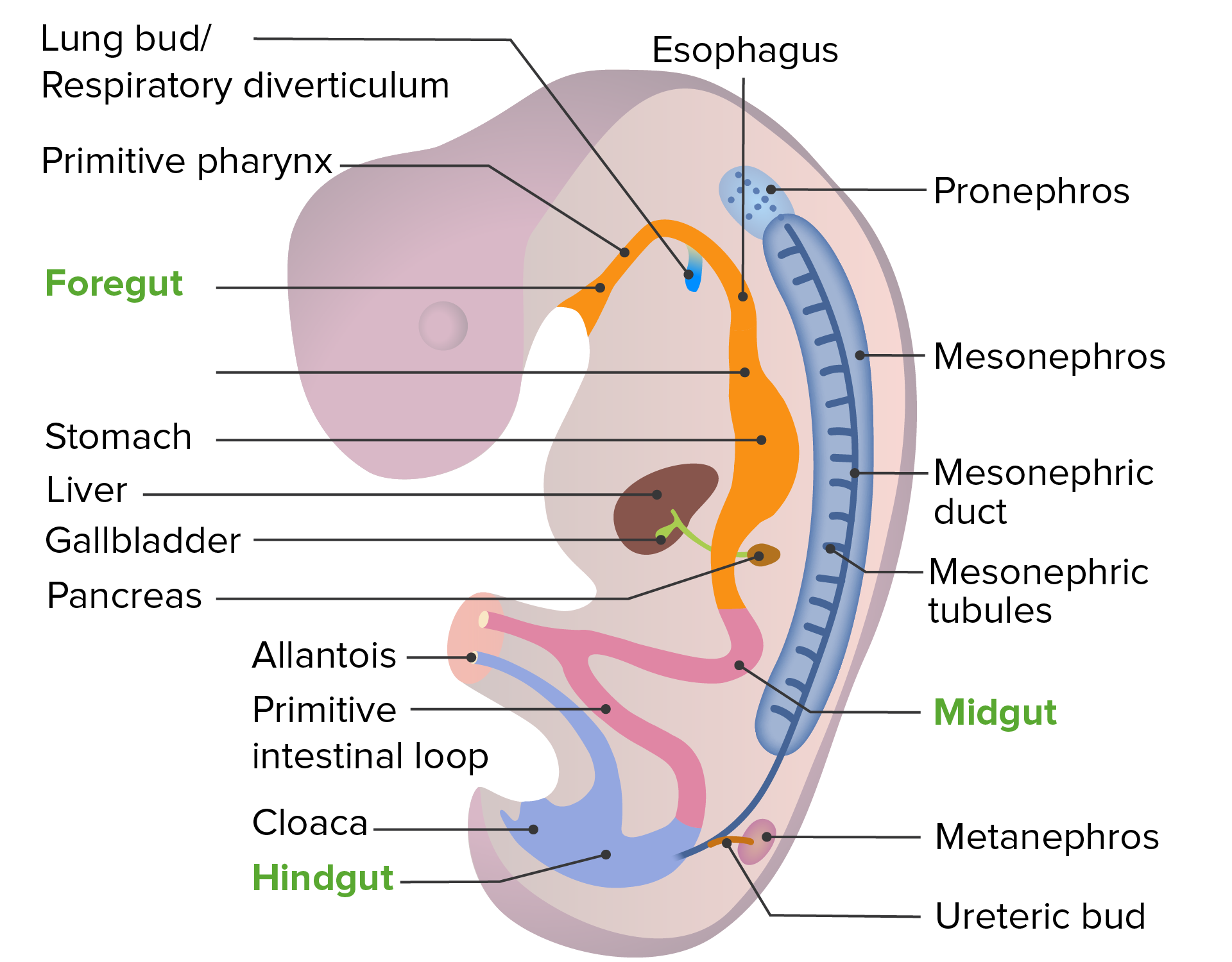
00:00 Hello. Now we're going to discuss Mullerian anomalies. First I want to tell you that in the current literature we referred to these anomalies or abnormalities as variants. So you may see that in a test question, don't be alarmed, it means the same thing. Now we'll talk about how Mullerian duct anomalies actually are the second most common cause of primary amenorrhea after gonadal dysgenesis. You can read more or listen more about gonadal dysgenesis and primary amenorrhea in other lectures. Abnormalities of the paramesonephros or the Mullerian ducts are common and are present in 7 to 10% of all women. They are associated with somatic anomalies such as renal anomalies, skeletal anomalies such as scoliosis and rarely cardiac or middle ear abnormalities. 00:57 We think that there may be a familial inheritance. Let's now look at this. What is this you think? Well, if you haven't read by now, it's a horseshoe kidney. This is a common anomaly we might see in a patient who has Mullerian agenesis or Mullerian anomalies. This is important to know if you're a surgeon and you need to operate on a woman. This is what it looks on an MRI. You can see here expands the entire abdomen. Let's now talk about the incidence of Mullerian defects. 01:36 In fertile and infertile women, it occurs in 3 to 4% of that population. It occurs in 5 to 10% of women who have recurrent miscarriage. That means she has had more than 2 miscarriages in life. 01:50 Some definitions say more than 3. Women with late miscarriage or preterm deliveries are overwhelmingly more likely to have Mullerian defect in greater than 25%. In all patients, we think that the incidence of congenital uterine anomalies accounts for 5 per 1000 female births. I now would like to go over the embryologic development in the uterus. Usually, we have 2 uterine tubes that form in the midline and between them a uterine septum occurs. This uterine septum should be resorbed and have a uniform combine uterine cavity. However, sometimes the uterine septum is not resorbed and that leads to a septate uterus. By the end of the third month, an immature uterus is formed and it should have a normal lumen. However, different confirmations of the uterine tubes that can come together lead to anomalies which we'll review in just a second. It's important to know that the newborn has a fully functional uterus, it's just small because it hasn't been exposed to estrogen yet. Now let's talk about the Mullerian anomalies or variants. You can have a uterine didelphys which is a double uterus and a double vagina and 2 cervices. Sometimes you can have a double uterus with a single vagina and potentially 2 cervices. If you're wondering do you need to do a Pap smear on both cervices? I'll let you answer that. The answer is yes. If she has 2 cervices which means 2 cervixes, then she will need a double Pap smear. You can also have a bicornuate uterus. You can have a bicornuate uterus with a small uterine horn on 1 side. 03:46 You can have a septate uterus that is divided in the middle and sometimes that septum can extend to the vagina or you can have a uterus that only has 1 duct on 1 side. We call that a unicornuate uterus. Let's now look at how these uteri would appear if you sent them for imaging. So, here in panel A we see the unicornuate uterus. In panel B, we see a bicornuate uterus. In panel C, we see a complete septate uterus that actually has a uterus with 2 cervices. We see here in panel D that we have a partial septate uterus. Lastly, this is a very uncommon finding, in panel E we have a uterus with DES exposure. They typically have a T-shaped uterus. Let's now talk about a case. This is a case that I actually had. "A 32-year-old G0 presented with infertility. During her evaluation, I did a transvaginal ultrasound and an HSG or hysterosalpingogram. Typically I use an HSG to check for tubal patency. It can also give me a snapshot of the cavity as well." We're going to look at some images in just a second. As we look at these images, I want you to think about what her diagnosis is, what abnormalities are we looking for? Is this finding contributing to her infertility? Let's review the first film. In radiology, I did a hysterosalpingogram with dye. 05:23 Here, you typically would see a uterine cavity and tubes bilaterally. However, in this patient, you can see the dye was injected and it went into 2 horns. What do you think she has? This is a frontal view. You can see here that the cervix is here at the bottom. At the top, you can see that there is dye going into 2 cavities or 2 cornua. This is the ultrasound and if you haven't guessed it already, I think she has a bicornuate uterus but how would you confirm? Still thinking? Okay, I'll tell you. Usually, we do a 3D ultrasound or MRI. This helps differentiate between a bicornuate uterus and a septate uterus. The exterior contour of the uterine cavity will help us to determine the diagnosis. Mullerian anomalies are associated with renal anomalies as well as vertebral findings. You can find that out with an MRI as well. Mullerian variants typically don’t have infertility. Their ovaries should be normal. However, they can suffer from gynecologic and obstetric concerns such as recurrent pregnancy loss, intrauterine growth restriction, and malpresentation. 06:44 Malpresentation means that they can be breech. The IUGR is because their uterus usually has an abnormal character to their blood supply. RPL or recurrent pregnancy loss is discussed in another lecture. Let's now talk about the specific variants that you can find. The most common is a septate uterus. The second most common is a bicornuate uterus followed by an arcuate uterus, although some would argue this is just a normal uterus and that we shouldn't classify it as an anomaly. 07:16 You can also have a unicornuate uterus or a uterine didelphys or double uterus, double cervix, and double vagina.
About the Lecture
The lecture Müllerian Duct Anomalies (MDA) by Lynae Brayboy, MD is from the course Abnormal Menstruation. It contains the following chapters:
- Müllerian Duct Abnormalities
- Classification of Müllerian Anomalies
- Müllerian Variant Case
Included Quiz Questions
Which of the following is the most common presentation of Mullerian defects?
- Women with late miscarriages and preterm delivery.
- Women with frequent thromboembolic events.
- Women who are infertile.
- Women who present with recurrent miscarriages.
- Women without menses.
Which of the following is usually NOT associated with Mullerian dysgenesis?
- Pancreatic divisum
- Horseshoe kidney fused in the upper pole
- Horseshoe kidney fused in the lower pole
- Vertebral anomalies
- Scoliosis
What uterine anomaly is caused due to a persistent urogenital septum?
- Septate uterus
- Double uterus and double vagina
- Double uterus and single vagina
- Bicornuate uterus
- Bicornuate uterus with small vaginal horn
Which of the following tests can be used to differentiate uterine septum and bicornuate uterus?
- 3D ultrasound
- Hysterosalpingogram
- CT scan
- Laparoscopy
- 2D ultrasound
Which of the following is the least common complication of having Mullerian variants?
- Infertility
- Recurrent pregnancy loss
- IUGR
- Malpresentation
Which of the following is the most common Müllerian duct anomaly?
- Septate uterus
- Bicornuate uterus
- Arcuate uterus
- Unicornuate uterus
- Uterus didelphys
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |