Playlist
Show Playlist
Hide Playlist
Mitral Valve Prolapse: Examination
-
Slides Valvular Heart Disease Mitral Regurgitation Cardiovascular Pathology.pdf
-
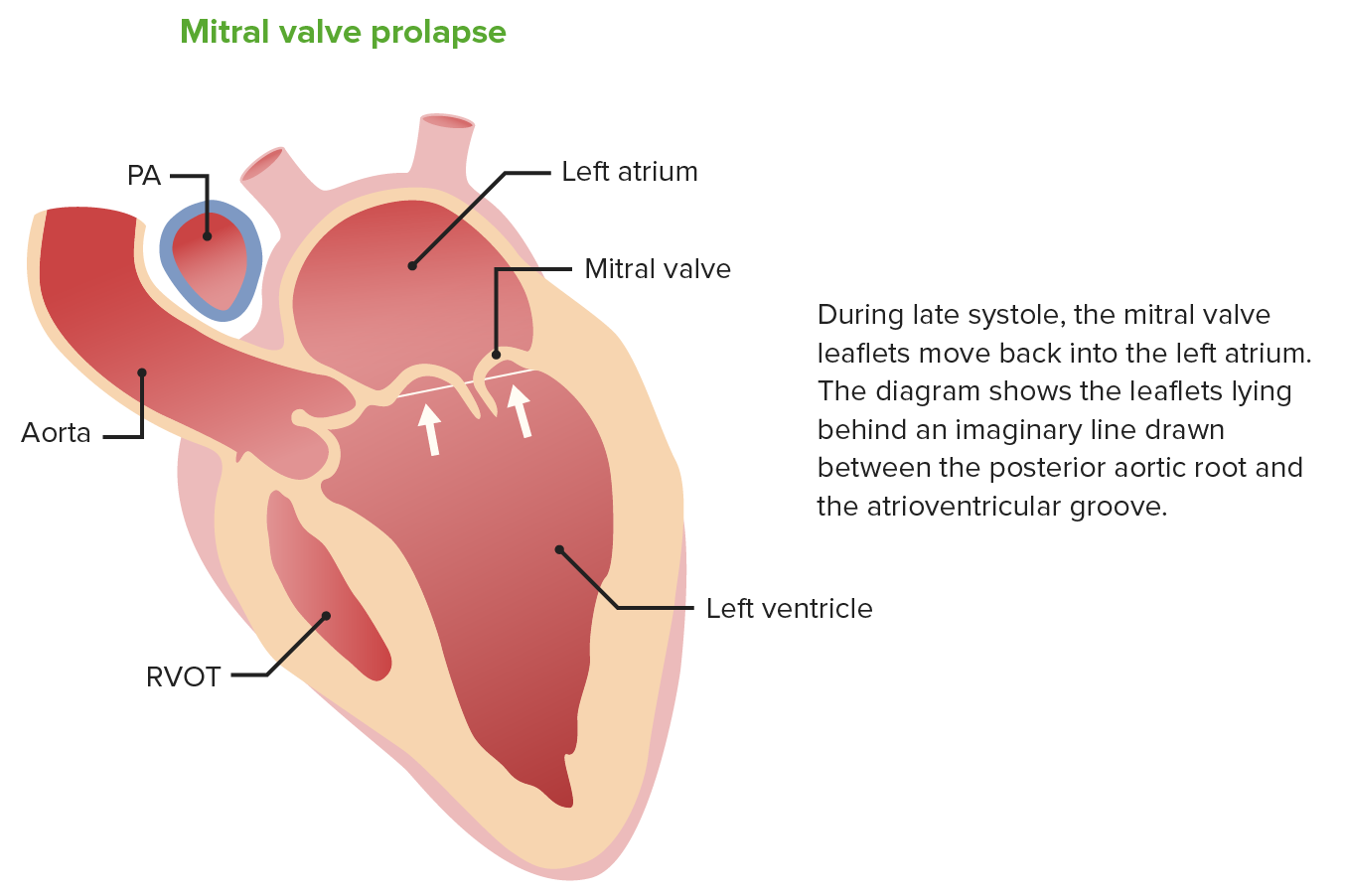
Download Lecture Overview
00:01 Here we go. 00:02 So, four components, S1, S2. We'll knock out the two. 00:07 MSC stands for midsystolic click, that's the third component. 00:13 What's the fourth component? You see that orange shaded area? That's the murmur. Four component. There you have it, one, two, three, four. 00:21 What are you trying to do objectively to manage your patient? You're trying to take that murmur and you wanna reduce the size of it. 00:28 What do you call this? You see the bottom picture? The bottom picture on your right says delayed, what's delayed? The murmur or the click got delayed it gets closer to S2 so the murmur becomes very, very shortened; that is lessening of your intensity of that murmur. 00:48 What does that mean? Delayed click that click gets closer to us, too, what happens to the size of the murmur? You're squishing the murmur and by doing so you're decreasing the intensity of the murmur. 01:00 What would you recommend as a doctor for that young lady? I keep saying young lady because that will be that is who will be the most common presentation, a young lady with midsystolic click, MVP and by recommending exercise which then increases pre-load, if you don't believe me, you ask any female out there that has an MVP and ask them what their doctor, if they know what they're doing, should be recommending exercise. 01:25 If that doesn't work, if exercise is not, not compatible with your patient, then you start thinking about something that will cause delayed contractility. 01:36 Maybe a beta blocker, cuz if you have beta blocker what happens? Oh, heart slows down, I get that, okay, and where's all my blood? Oh, in my heart does that increase preload? Correct. So what happens to the size of the murmur? It decreased. What happens to the click? It gets delayed. 01:52 What happens to the intensity of the murmur? Decreased. 01:54 Are you guys with me? Continue. 01:57 Patients do not always have regurgitation. Is that clear? Because if it was, then it would have a whole systolic murmur. Increase venous return delays click and shortens murmur, highlight that in your head forevermore. 02:10 Number one recommendation. Exercise. That bottom pictures shows exactly that. 02:15 Does delaying of the click, shortening of the murmur? Voila, you managed your patient. Decreased venous return, not good. 02:23 Let me give you an example of the maneuver, valsalva phase two. 02:28 What are you doing, ready for my face? Is that pretty? Well, I wasn't pretty to begin with but I just made it ridiculously unacceptable so I just had constipation. No, I didn't. Too much information. 02:40 That was epiglottis and I closed it and I was trying to exhale. 02:44 So what did I do? I increased my thoracic pressure, right? And then by doing so, you're compressing your pulmonary capillaries. 02:50 At first you increased it, no doubt, but phase two, you won't have any blood left to then return to the left side, so it's decreased the venous return to the left side. 03:01 Decreased. So you have decreased venous return on valsalva phase two. 03:05 What will happen to that click? It is early. And then what about the murmur? It is lengthened. Is that clear? What happens in the intensity of the murmur? It's increased. 03:15 So the lengthening of that murmur represents increased intensity; the shortening of that murmur represents decrease intensity. 03:23 If you've understood that much, there isn't a single questions that you could possibly get wrong anywhere with dealing with these murmurs. 03:31 We walked through aortic stenosis, aortic regurge, mitral regurge, and MVP. 03:36 A couple of others we have to walk through, but for the most part, there you have it. 03:40 Now, what we have here is the following. I want to show you these, you're gonna love this. 03:45 This is about mitral valve prolapse and then what happens to the four components. 03:50 Now, what you look at here on the top picture is an individual standing up. 03:56 Now before we begin, I want you to think of the following. 03:58 If you're standing up, where's my blood? In my legs. So what happens to the venous return? It's decreased. When you have decreased venous return there's decreased amount of the blood in your heart, so therefore what should the click look like? The click should be early, it should be right after S1. 04:14 And if you take a look at what's in yellow there and that click right after S1 is early, that's what that first line says. And then what about the murmur? It's lengthened and it's longer. 04:24 The murmur is what you're seeing in the middle and it is increased in size versus let's say that you have rapid squatting. 04:32 When you have rapid squatting, please understand that you're going to increase the amount of blood to the right side and when you do so, you have increased preload, that click at this point is going to be late, the murmur will be shortened. 04:46 And then we had handgrip. Handgrip is a little interesting. 04:50 Early, when we talked about handgrip and referred to the physiology, if you do a handgrip, you'll increase your TPR. 04:57 If you increase your TPR you increase your afterload. 05:00 Your afterload is much more affected in hand grip than it's preload, no doubt. 05:04 If you increase your afterload, what have you've done? You've increased the resistant of the left ventricle to eject blood, so there's more blood. Where? Well, yeah, more blood that you end up having in your heart. 05:15 So therefore, it kinda behaves like your squatting episode, rapid squatting. 05:19 You have a late click and you have a shorter type of murmur. 05:23 You've understood midsystolic, you've understood the physiology of these different maneuvers, standing up, squatting, hand grip. Once again, you won't be able to miss a question. 05:35 May I ask you a question here though? If it is aortic stenosis and you did a hand grip, what do you think happens to the intensity of the murmur? Take your time. Normally speaking, the blood should be moving, now, this is not on this table, but not to worry, if you've understood the physio, then this part here should make absolute sense. 05:55 Meaning to say, if you have aortic stenosis, crescendo/decrescendo murmur, I told you about calcification; if it's a young patient bicuspid aortic valve and if it's an older patient, senile dystrophic calcification. 06:07 And, normally, there should be a high gradient of blood from the left ventricle to the aorta. Are you with me? A high gradient, normally it should be injecting blood only into the aorta. 06:18 When you do a hand grip, when you increase your TPR, what then happens to the gradient? It decreases, so there's less blood crossing a stenotic aortic valve. 06:29 What happens to the intensity of the murmur? It would decrease. 06:32 Make sure that you work through this, if you haven't and it's not making sense yet, please make sure, review this portion before moving onto the next section. 06:42 This is not about frustration, this is about emboldening your ability to answer questions, to feel confident about what you're doing when you walked into the ward, walked into any room in which your knowledge is being tested, you should be able to answer with utmost confidence and not feel bad about anything that you're saying because you know that you're saying it correctly. 07:02 Confirm with echo MVP. What are you seeing? The prolapse of the valve into the left atrium. 07:08 Asymptomatic, ex in prognosis. What are you gonna recommend? You're going to recommend exercise, we're talking about MVP. 07:15 Now, that degree of MR determines the need for surgery. 07:19 At some point, could MVP result in a holosystolic murmur? Sure, and at that point you start thinking about, oh, I need to provide surgical replacement.
About the Lecture
The lecture Mitral Valve Prolapse: Examination by Carlo Raj, MD is from the course Valvular Heart Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following maneuvers decreases the length of the murmur in mitral valve prolapse?
- Rapid squatting
- Decreased preload
- Standing
- Decreased afterload
- Valsalva
Which of the following medications is used in the management of mitral valve prolapse and why?
- Beta-blockers, to slow the heart rate.
- Diuretics, to reduce preload
- Nitrates, to reduce preload and afterload.
- ACE inhibitors, to reduce fluid overload.
- Warfarin, to prevent pulmonary edema.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |