Playlist
Show Playlist
Hide Playlist
Minimal Change Disease – Nephrotic Syndrome
-
Slides Nephrotic Syndromes.pdf
-
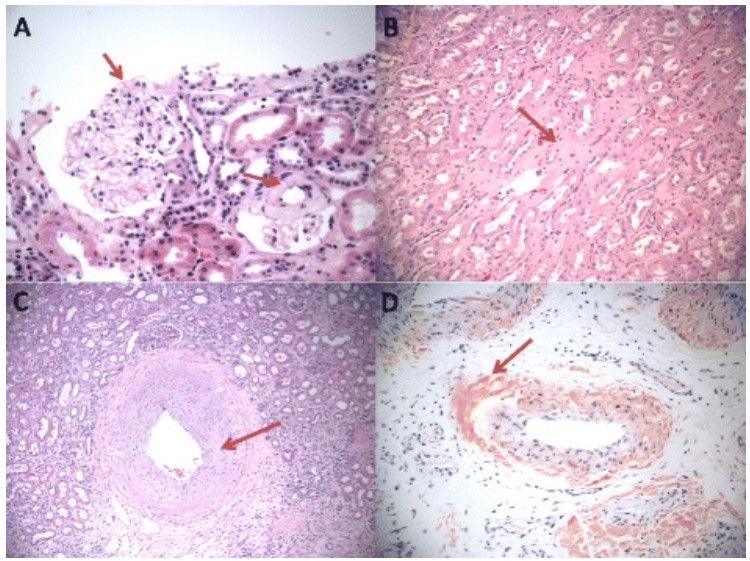
Download Lecture Overview
00:01 So minimal change disease really is the most common cause of nephrotic syndrome in children. 00:08 So about 90% of children less than the age of five years who get diagnosed with nephrotic syndrome is going to be due to minimal change disease. 00:15 Now interestingly, as children start to grow up about 50% of them over the age of 10 years have an increased in percentage developing FSGS. 00:24 So only 50% will be minimal change in the remainder is really due to FSGS. 00:30 In adult it's much less low, we only see about 10-15% of all nephrotic syndrome cases in adults being due to minimal change disease. 00:39 So when we think about the etiology or causes behind minimal change disease, there's three broad categories that we really need to think about. 00:46 Number 1, idiopathic, and all that means is that despite 40 Years of looking we still don't know the exact mechanism as to what causes minimal change disease. 00:56 But there are secondary form s too, things like drugs, and we just talked about one of them in our patient case example. 01:00 Remember she was taking high-dose ibuprofen. 01:03 So NSAIDs another reason that is kind of the enemy of the nephrologist can certainly precipitate or provoke nephrotic syndrome right with minimal change disease. 01:12 There certain antimicrobial agents that can do it as well as lithium. 01:16 And then finally neoplasm, Hodgkin's Disease and Non-Hodgkins Lymphoma, certain leukemias, and thymoma have all been associated with minimal change disease. 01:27 Okay, so when we think about the pathogenesis of minimal change disease, the exact cause certainly of idiopathic minimal changes not clear. 01:34 What we do know, is that there's some kind of systemic T-Cell dysfunction that's thought to result in a glomerular permeability factor. 01:42 And that permeability factor injures are podocytes leading to foot process effacement and proteinuria. 01:47 So I want you to focus on our schematic over here. 01:49 If you look at the top, then what you see is a normal glomerular capillary wall. 01:54 At the bottom portion, you see that the capillary lumen, It's lined by those endothelial cells that are in pink that yellow is the glomerular basement membrane. 02:03 And then those green little guys that look like a picket fence are are put aside foot processes and in between those foot processes, remember, they interdigitate with each other like this and they have a very elegant slip diaphragm and these guys really keep those macromolecules like albumin and other important things inside of that capillary lumen while they allow the ultra filtrate to be filtered into Bowman's space. 02:23 But look what happens when we have minimal change disease that permeability factor comes along we then get foot price, we then get actin cytoskeleton rearrangement and foot process of effacement. 02:33 So if you look at our schematic, you can see that foot processes instead of standing like a picket fence. 02:39 They're actually effaced and then the slit diaphragm that's between them is breached. 02:45 And so now we've got macromolecules like albumin and other large molecules that can escape into that glomerular filtrate into Bowman's space and ultimately the urine. 02:55 All right, so what do we see pathologically when we biopsy our patients. 02:58 On light microscopy, I want you to focus on what our actual pathological image looks like. 03:03 It's very reminiscent of our normal glomerulus that we showed in the beginning. 03:07 Why is that? because there are minimal changes histologically when we have minimal change disease that is why it's critical when you're diagnosing these patients and you're actually requesting the biopsy you want to make sure one of those cores is actually going in for electron microscopy because that's where you're going to clench your diagnosis. 03:25 So here's my representation of our electron micrograph showing minimal change disease and what's being shown here is an actual loop of capillary wall. 03:34 The inside you can see that dark portion that looks like a sea is a red blood cell, and then what my arrow is pointing to is actually the effacement of our podocytes foot processes. 03:43 All you can see is underlying basement membrane, but those foot processes instead of standing like a nice picket line are completely effaced. 03:50 So it diaphragms are breached macromolecules can now filter through. 03:56 So our patients typically when they have minimal change will present absolutely with nephrotic syndrome. 04:01 It is not subtle. 04:02 They usually present very profoundly. 04:05 They can have lipiduria. 04:07 Otherwise, the urine sediment is bland if I'm looking at it underneath the microscope. 04:11 They have no serum complement abnormalities. 04:14 So I'm not going to be looking for compliment on my serological tests. 04:17 And they often times or to a certain degree can present with renal failure typically due to tubular injury and I see that my older population oftentimes, it's because they're getting concurrent diuretics and they're very very vulnerable to developing ischemic injuries. 04:34 Historically, untreated minimal change disease was actually associated with a risk of mortality and that's due to infection. 04:40 Remember we talked about how those immunoglobulins get lost into the urine because of richment of that glomerular capillary wall. 04:47 So when that happens patients are at an increased risk of infection and a risk also of thromboembolism. 04:52 Why? remember these patients have very high grade proteinuria they're losing clotting inhibitors through their urine as well. 04:59 So our patients, fortunately are generally responsive to steroid therapy and have relatively a good prognosis. 05:07 Of course as the rule always goes in any glomerular disease, children are going to respond much better than adults. 05:13 So how do we treat our patients when they present to us? We are going to treat them usually with high-dose steroids. 05:18 We give them for 12 to 16 weeks. 05:20 So something like prednisone given at 1 milligram per kilogram. 05:24 It's a pretty long period of time four months and they get a progressive taper over a six-month period of time. 05:30 Because this is such an abrupt onset and the disease is relatively self-limiting, we don't have to use ACE or ARB's in her patients unless they're extremely hypertensive and statins aren't always needed, again, because the duration is much less shorter. 05:45 Now for some of our patients who are steroid dependent meaning that as I try to taper them off their steroids, they blossom again with their nephrotic syndrome, so I can't taper them or a patient who's had a relapse at least three times during a year. 05:58 Those patients are considered steroid dependent. 06:00 So in that population, I can actually give them that alkylating agent cyclophosphamide. 06:04 Give that for an eight-week duration and that can actually decrease their dependence on steroids. 06:09 We can also use cyclosporine as an alternative if patients are resistant to steroids. 06:14 But if I have a patient that's completely resistant, and their proteinuria is not decreasing at all. 06:20 I might want to consider re-biopsying them as I may have missed the diagnosis. 06:25 So a portion of those patients might end up actually having focal segmental glomerulosclerosis which we'll talk about shortly. 06:33 Finally, there are some people, were some patients who become steroid dependent that we can actually treat with other therapies that are a little bit less toxic than cyclophosphamide and that includes mycophenolate mofetil which is an anti metabolites, and rituximab, again, we've seen that before in membranous. 06:48 This isn't a monoclonal antibody to CD20 and that also has been successful in case studies in case series for people who have steroid dependent minimal change disease.
About the Lecture
The lecture Minimal Change Disease – Nephrotic Syndrome by Amy Sussman, MD is from the course Nephrotic Syndrome.
Included Quiz Questions
Which of the following is involved in the pathogenesis of minimal change disease?
- Systemic T-cell dysfunction
- Autoantibodies to the glomerular basement membrane
- Extensive activation of the complement system
- Autoantibodies to structures within the nucleus
- Persistent hepatitis B virus antigenemia
Which of the following is associated with minimal change disease?
- Absence of significant changes viewed under light microscopy
- Low C3 and C4 complement levels
- Elevated levels of IgA and IgG
- Elevated HDL levels
- Absence of significant changes viewed on electron microscopy
What is the first-line treatment for minimal change disease?
- Glucocorticoids
- ACE inhibitors/ARBs
- Cyclophosphamide
- NSAIDs
Which of the following is true regarding minimal change disease?
- It occurs more often in children than adults.
- Steroid therapy tends to worsen the disease course.
- Adults respond to therapy better than children.
- Serum complement levels are a good diagnostic test for minimal change disease.
- It is often associated with easy bruising and bleeding.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |