Playlist
Show Playlist
Hide Playlist
Mesenteric Ischemia
-
Slides GIP Mesenteric Ischemia.pdf
-
Download Lecture Overview
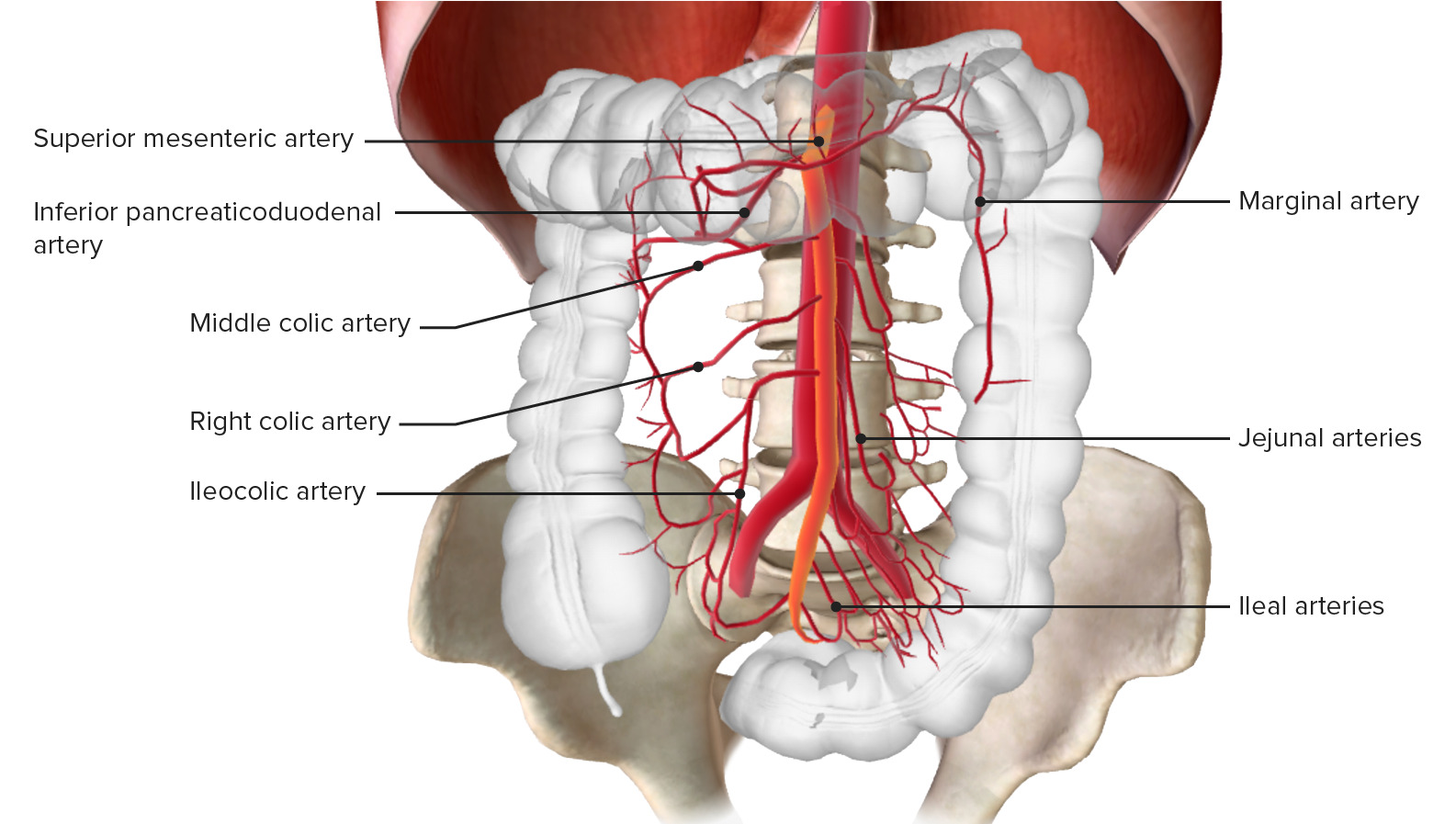
00:01 Welcome. In this presentation, we're going to be covering mesenteric ischemia. 00:04 Essentially, this is intestinal hypoperfusion and if it's severe enough and long enough, we will get frank ischemia and then, necrosis due to infarction. You can have either very acute, a sudden decrease in blood supply or you can have more chronic low-grade hypoperfusion. 00:23 If it's sudden, it's usually due to a decrease in blood flow through embolization or a volvulus or something else that acutely compromises vascular supply. 00:35 For chronic diseases, it's usually due to atherosclerosis, so, kind of a chronic occlusion of the vessel, the main vessels coming off of the aorta that are limiting flow into the GI tract. 00:49 So, on our road map for mesenteric ischemia, let's first look at the epidemiology. 00:54 About 0.1% of all hospital admission are due to acute mesenteric ischemia. 01:01 So, not a common cause but a very serious cause. 01:05 This is typically seen in the geriatric population, patients who are 60 years and older. 01:11 Unfortunately, although it has a relatively lower frequency of hospital admission, it has a relatively high mortality rate. 01:19 So, about 60% of patients who have this will end up infracting their bowel and having severe mortal complications. 01:28 In chronic disease, it's relatively rare to be a cause for hospitalization but can still have significant symptomatology. 01:37 In chronic disease, a majority of the cases are inpatients who are more elderly and it does occur more commonly in women. 01:46 In terms of the pathophysiology. Again, we're going to break this down in terms of acute and chronic. 01:52 In acute as I've already mentioned, it's going to be due at least 50% of the time to embolization. 01:58 So, an arrhythmia or endocarditis, or myocardial infarction leading to the formation of a thrombus or a vegetation within the lumen of the heart can have a subsequent effect of embolizing into distal vessels, including into the mesenteric arteries. That occlusion will cause an acute mesenteric ischemia. 02:25 Arterial thrombosis on the other hand will happen in the setting of more chronic atherosclerosis. 02:32 Acute plaque rupture of significant arterial disease can also lead to acute mesenteric ischemia. 02:40 Hypoperfusion can also be a cause of acute mesenteric ischemia. 02:45 So, just low blood flow with or without vascular compromise, say, due to atherosclerotic disease can lead to areas of relative hypoperfusion within the bowel. 02:56 What's being circled are actually the watershed zones in the large colon. 03:01 So, the one at the top at the splenic flexure is the watershed zone between the superior mesenteric artery and the inferior mesenteric artery and that anastomosis collateralization is going to be most susceptible to hypoperfusion. 03:16 The one on the bottom within the sigmoid colon is going to be at the watershed between inferior mesenteric artery distribution and the right iliac internal artery. 03:30 Venous thrombosis is a relatively infrequent cause of acute mesenteric ischemia but tumor or hypercoagulability can lead to occlusion of the vessel and that will lead to relatively poor flow through the venous circulation through the capillary bed and compromising the arterial inflow into the tissue. In chronic disease, the major cause overall is atherosclerosis where we have accumulation of a plaque. 04:02 And then, progressive, chronic occlusion of the vasculature. 04:07 So, we have diminished flow and it gets worse, and worse, and worse overtime. 04:12 If we have an acute change in the atherosclerotic plaque, that can give us acute mesenteric ischemia but this chronic progressive occlusion compromising flow is the cause of chronic. 04:24 There are rare causes as you can see here and read quite well. 04:29 For the mesenteric ischemia, but we're not going to go into any particular detail on these. 04:36 So, we're looking here at the perfusion of the inferior mesenteric artery and you can see again that predominantly, from the splenic flexure down to the sigmoid colon is what the inferior mesenteric artery is supposed to be perfusing. 04:52 On the other hand, we're showing the perfusion for the superior mesenteric artery and it goes more or less, when it goes for the entire small bowel but also provides perfusion from the cecum all the way up the ascending colon through the transverse colon, to the splenic flexure. 05:12 As we cut off the blood supply to the bowel, we're going to start seeing mucosal damage that will occur within about three hours of ischemia. 05:23 These cells have a relatively high metabolic rate and can die relatively quickly. 05:28 If the mucosa dies as a result of ischemia, then, we'll get gastrointestinal bleeding and we will begin to have this real pain. 05:38 That inflammation associated with the bleeding is going to release vasoactive mediators and bacteria and toxic byproducts that are going to further compromise the vascular flow into the tissue. 05:50 Within six hours, we'll have transmural necrosis of the bowel and at that time, now, we can have perforation and peritonitis. The clinical presentation depends on whether it's acute or chronic. 06:05 In acute mesenteric ischemia, the classic triad is said to be diffuse and severe abdominal pain, out of proportion to any clinical findings and it doesn't seem to be reproduced or worsened with palpation. 06:18 The gut is emptying, so, there is diarrhea and vomiting due to ischemia and then, increased bowel contractions. And there will be classically red, so called currant jelly stools. 06:30 Now, other things can do this. So, just because you have these findings doesn't mean acute mesenteric ischemia but certainly, the findings of these should send you in that general direction. 06:43 Between acute mesenteric ischemia where we haven't had infarction to now where we do have infarction, if there's peritonitis, so, now, if we have guarding, rigidity, and absent bowel sounds, if the patient has fever, tachycardia, and hypotension, signs suggestive of sepsis. 07:02 Or if there's bright red blood per rectum, then, we can start worrying that we have in fact gone beyond just ischemia and have gone into frank infarction and we're at risk of perforation. 07:14 With chronic mesenteric ischemia, we get episodic abdominal pain. It's the equivalent of intestinal angina. 07:22 As you eat, you increase the need for blood supply into the colon and if you're not getting adequate blood supply, a postprandial pain will kind of signal that intestinal angina. It tends to be dull and crampy. 07:40 It tends to be up in the areas, kind of epigastrium and into the splenic flexure. 07:46 So, at areas where we have our normal watershed areas between the inferior and superior mesenteric arteries. 07:53 With chronic ischemia, you may not be getting appropriate absorption of nutrition. 08:00 So, there will be weight loss. And in these settings, you frequently will hear, although, not always, an abdominal bruit due to atherosclerotic disease involving one of the major vessels, the superior mesenteric artery or the inferior mesenteric artery. How do we make the diagnosis? So, the laboratories are somewhat non-specific. If we see lactic acid that says that we have ischemia someplace. 08:24 An elevated LDH may also suggest that we have bowel ischemia. 08:29 A metabolic acidosis going along with a lactic acidosis is indicative potentially bowel ischemia if we don't have an ischemic focus someplace else. Leukocytosis with a left shift is indicative impending perforation and transmural infarction and you may have elevated amylases due to a contemporaneous pancreatitis due to poor perfusion. 08:53 Imaging studies are usually quite helpful. You can do plain x-ray and look for distended loops of bowel. 09:01 You can do an ultrasound looking for areas of induration and edema and CT with angiography is the preferred method for diagnosis where you try to see that there's normal perfusion of all portions of the colon. 09:15 So, what do we do about this? If it is a case of acute mesenteric ischemia, we are going to want to obviously provide fluid resuscitation to maintain blood pressure. 09:25 We're going to give broad spectrum antibiotics in anticipation that we're going to have a bowel perforation. 09:30 We want to decompress the upper GI tract. So, nothing by mouth and a nasogastric tube put down to section out anything that may be sloshing around in the stomach. 09:42 Pain control is a must. We will give system anticoagulation such as heparin because if the occlusion, the mesenteric ischemia, is due to a ruptured atherosclerotic plaque and thrombosis that will help us in terms of maintaining perfusion. You may also do endovascular angioplasty in the same way that we can put in a balloon and dilate a vessel in the setting of acute myocardial infarct. 10:08 We can do exactly the same thing in acute mesenteric ischemia. And in the event that none of that works, you can do surgery because now, you have loops of infarcted bowel and the relatively blue, black loops of bowel that you see there have infarcted and need to be removed before you have frank perforation. 10:29 With that, mesenteric ischemia top to bottom.
About the Lecture
The lecture Mesenteric Ischemia by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
What age demographic is most commonly diagnosed with acute mesenteric ischemia?
- Over 60 years old
- 50–60 years old
- 40–50 years old
- 30–40 years old
- Under 30 years old
What is the most common cause of acute mesenteric ischemia?
- Embolization
- Arterial thrombosis
- Hypoperfusion
- Venous thrombosis
- Vasculitis
In acute mesenteric ischemia, how long is it until the development of necrosis?
- 6 hours
- 3 hours
- 30 minutes
- 1 hour
- 1 day
What symptoms are part of the classic triad of acute mesenteric ischemia? Select all that apply.
- Diffuse and severe abdominal pain
- No worsening or reproduction with palpation
- Gut emptying
- Anemia
- Constipation
Which is NOT part of the initial management of acute mesenteric ischemia?
- Endovascular angioplasty
- Fluid resuscitation
- Broad-spectrum antibiotics
- Nasogastric decompression
- Pain control
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |